Global Aids Monitoring Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HIV/AIDS Beh Dukw Haviour Wi Refug Ral Surv Gee Cam Veillanc
HIV/AIDS Behavioural Surveillance Survey (BSS) Dukwi Refugee Camp, Botswana May 2013 UNHCR & Botswana Ministry of Health 1 Acknowledgements The 2012 Botswana Behavioural Surveillance Survey (BSS) was a joint effort of UNHCR and the Botswana Ministry of Health, with funding from UNAIDS and WHO, and the support of Botswana Red Cross Society. The BSS was initiated and coordinated by Ms. Marian Schilperoord of UNHCR Geneva, and Dr. Njogu Patterson of UNHCR Pretoria, whose depth of experience overseeing similar surveys was incredibly valuable. Dr. Emmanuel Baingana of UNAIDS and Dr. Eugene Nyarko of WHO lent invaluable advice and support during critical phases of the project, and we are exceptionally grateful. The investigation team was led by the Principal Investigator Ms. Aimee Rose who managed the adaptation of the protocol and tools, field work, analysis and reporting. Dr. Marina Anderson, Co‐ Principal Investigator from the Ministry of Health, provided excellent technical oversight and coordination with the Ministry of Health. Three Investigators from the Ministry of Health, Ms. Lumba Nchunga, Ms. Betty Orapeleng and Ms. Bene Ntwayagae, provided input in each phase of the survey, from protocol development, pre‐planning missions to Dukwi Camp, monitoring of training and field work, and report compilation. The team benefitted from the dedicated support of UNHCR Country Representative Lynn Ngugi. We give special appreciation to UNHCR Program Officer Galefele Beleme for her tireless work on recruiting, finance, and logistics, and numerous other issues. UNHCR Head of Field Office Jane Okello facilitated the survey’s success at Dukwi Camp, with superb assistance from UNHCR staff Niroj Shrestha, Gracias Atwine, and Onkemetse Leburu. -

Populated Printable COP 2009 Botswana Generated 9/28/2009 12:01:26 AM
Populated Printable COP 2009 Botswana Generated 9/28/2009 12:01:26 AM ***pages: 415*** Botswana Page 1 Table 1: Overview Executive Summary None uploaded. Country Program Strategic Overview Will you be submitting changes to your country's 5-Year Strategy this year? If so, please briefly describe the changes you will be submitting. X Yes No Description: test Ambassador Letter File Name Content Type Date Uploaded Description Uploaded By Letter from Ambassador application/pdf 11/14/2008 TSukalac Nolan.pdf Country Contacts Contact Type First Name Last Name Title Email PEPFAR Coordinator Thierry Roels Associate Director GAP-Botswana [email protected] DOD In-Country Contact Chris Wyatt Chief, Office of Security [email protected] Cooperation HHS/CDC In-Country Contact Thierry Roels Associate Director GAP-Botswana [email protected] Peace Corps In-Country Peggy McClure Director [email protected] Contact USAID In-Country Contact Joan LaRosa USAID Director [email protected] U.S. Embassy In-Country Phillip Druin DCM [email protected] Contact Global Fund In-Country Batho C Molomo Coordinator of NACA [email protected] Representative Global Fund What is the planned funding for Global Fund Technical Assistance in FY 2009? $0 Does the USG assist GFATM proposal writing? Yes Does the USG participate on the CCM? Yes Generated 9/28/2009 12:01:26 AM ***pages: 415*** Botswana Page 2 Table 2: Prevention, Care, and Treatment Targets 2.1 Targets for Reporting Period Ending September 30, 2009 National 2-7-10 USG USG Upstream USG Total Target Downstream (Indirect) -

Department of Road Transport and Safety Offices
DEPARTMENT OF ROAD TRANSPORT AND SAFETY OFFICES AND SERVICES MOLEPOLOLE • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate Tel: 5920148 Fax: 5910620 P/Bag 52 Molepolole Next to Molepolole Police MOCHUDI • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Transport Inspectorate P/Bag 36 Mochudi Tel : 5777127 Fax : 5748542 White House GABORONE Headquarters BBS Mall Plot no 53796 Tshomarelo House (Botswana Savings Bank) 1st, 2nd &3rd Floor Corner Lekgarapa/Letswai Road •Registration & Licensing of vehicles and drivers •Road safety (Public Education) Tel: 3688600/62 Fax : Fax: 3904067 P/Bag 0054 Gaborone GABORONE VTS – MARUAPULA • Registration & Licensing of vehicles and drivers • Driver Examination (Theory & Practical Tests) • Vehicle Examination Tel: 3912674/2259 P/Bag BR 318 B/Hurst Near Roads Training & Roads Maintenance behind Maruapula Flats GABORONE II – FAIRGROUNDS • Registration & Licensing of vehicles and drivers • Driver Examination : Theory Tel: 3190214/3911540/3911994 Fax : P/Bag 0054 Gaborone GABORONE - OLD SUPPLIES • Registration & Licensing of vehicles and drivers • Transport Permits • Transport Inspectorate Tel: 3905050 Fax :3932671 P/Bag 0054 Gaborone Plot 1221, Along Nkrumah Road, Near Botswana Power Corporation CHILDREN TRAFFIC SCHOOL •Road Safety Promotion for children only Tel: 3161851 P/Bag BR 318 B/Hurst RAMOTSWA •Registration & Licensing of vehicles and drivers •Driver Examination (Theory & Practical -
Directory of Financial Institutions Operating in Botswana As at December 31, 2019
PAPER 4 BANK OF BOTSWANA DIRECTORY OF FINANCIAL INSTITUTIONS OPERATING IN BOTSWANA AS AT DECEMBER 31, 2019 PREPARED AND DISTRIBUTED BY THE BANKING SUPERVISION DEPARTMENT BANK OF BOTSWANA Foreword This directory is compiled and distributed by the Banking Supervision Department of the Bank of Botswana. While every effort has been made to ensure the accuracy of the information contained in this directory, such information is subject to frequent revision, and thus the Bank accepts no responsibility for the continuing accuracy of the information. Interested parties are advised to contact the respective financial institutions directly for any information they require. This directory excludes collective investment undertakings and International Financial Services Centre non-bank entities, whose regulation and supervision falls within the purview of the Non-Bank Financial Institutions Regulatory Authority. Lesedi S Senatla DIRECTOR BANKING SUPERVISION DEPARTMENT 2 DIRECTORY OF FINANCIAL INSTITUTIONS OPERATING IN BOTSWANA TABLE OF CONTENTS 1. CENTRAL BANK ..................................................................................................................................... 5 2. COMMERCIAL BANKS ........................................................................................................................... 7 2.1 ABSA BANK BOTSWANA LIMITED ........................................................................................................... 7 2.2 AFRICAN BANKING CORPORATION OF BOTSWANA LIMITED .................................................................. -

The Big Governance Issues in Botswana
MARCH 2021 THE BIG GOVERNANCE ISSUES IN BOTSWANA A CIVIL SOCIETY SUBMISSION TO THE AFRICAN PEER REVIEW MECHANISM Contents Executive Summary 3 Acknowledgments 7 Acronyms and Abbreviations 8 What is the APRM? 10 The BAPS Process 12 Ibrahim Index of African Governance Botswana: 2020 IIAG Scores, Ranks & Trends 120 CHAPTER 1 15 Introduction CHAPTER 2 16 Human Rights CHAPTER 3 27 Separation of Powers CHAPTER 4 35 Public Service and Decentralisation CHAPTER 5 43 Citizen Participation and Economic Inclusion CHAPTER 6 51 Transparency and Accountability CHAPTER 7 61 Vulnerable Groups CHAPTER 8 70 Education CHAPTER 9 80 Sustainable Development and Natural Resource Management, Access to Land and Infrastructure CHAPTER 10 91 Food Security CHAPTER 11 98 Crime and Security CHAPTER 12 108 Foreign Policy CHAPTER 13 113 Research and Development THE BIG GOVERNANCE ISSUES IN BOTSWANA: A CIVIL SOCIETY SUBMISSION TO THE APRM 3 Executive Summary Botswana’s civil society APRM Working Group has identified 12 governance issues to be included in this submission: 1 Human Rights The implementation of domestic and international legislation has meant that basic human rights are well protected in Botswana. However, these rights are not enjoyed equally by all. Areas of concern include violence against women and children; discrimination against indigenous peoples; child labour; over reliance on and abuses by the mining sector; respect for diversity and culture; effectiveness of social protection programmes; and access to quality healthcare services. It is recommended that government develop a comprehensive national action plan on human rights that applies to both state and business. 2 Separation of Powers Political and personal interests have made separation between Botswana’s three arms of government difficult. -

Botswana Semiology Research Centre Project Seismic Stations In
BOTSWANA SEISMOLOGICAL NETWORK ( BSN) STATIONS 19°0'0"E 20°0'0"E 21°0'0"E 22°0'0"E 23°0'0"E 24°0'0"E 25°0'0"E 26°0'0"E 27°0'0"E 28°0'0"E 29°0'0"E 30°0'0"E 1 S 7 " ° 0 0 ' ' 0 0 ° " 7 S 1 KSANE Kasane ! !Kazungula Kasane Forest ReserveLeshomo 1 S Ngoma Bridge ! 8 " ! ° 0 0 ' # !Mabele * . MasuzweSatau ! ! ' 0 ! ! Litaba 0 ° Liamb!ezi Xamshiko Musukub!ili Ivuvwe " 8 ! ! ! !Seriba Kasane Forest Reserve Extension S 1 !Shishikola Siabisso ! ! Ka!taba Safari Camp ! Kachikau ! ! ! ! ! ! Chobe Forest Reserve ! !! ! Karee ! ! ! ! ! Safari Camp Dibejam!a ! ! !! ! ! ! ! X!!AUD! M Kazuma Forest Reserve ! ShongoshongoDugamchaRwelyeHau!xa Marunga Xhauga Safari Camp ! !SLIND Chobe National Park ! Kudixama Diniva Xumoxu Xanekwa Savute ! Mah!orameno! ! ! ! Safari Camp ! Maikaelelo Foreset Reserve Do!betsha ! ! Dibebe Tjiponga Ncamaser!e Hamandozi ! Quecha ! Duma BTLPN ! #Kwiima XanekobaSepupa Khw!a CHOBE DISTRICT *! !! ! Manga !! Mampi ! ! ! Kangara # ! * Gunitsuga!Njova Wazemi ! ! G!unitsuga ! Wazemi !Seronga! !Kaborothoa ! 1 S Sibuyu Forest Reserve 9 " Njou # ° 0 * ! 0 ' !Nxaunxau Esha 12 ' 0 Zara ! ! 0 ° ! ! ! " 9 ! S 1 ! Mababe Quru!be ! ! Esha 1GMARE Xorotsaa ! Gumare ! ! Thale CheracherahaQNGWA ! ! GcangwaKaruwe Danega ! ! Gqose ! DobeQabi *# ! ! ! ! Bate !Mahito Qubi !Mahopa ! Nokaneng # ! Mochabana Shukumukwa * ! ! Nxabe NGAMILAND DISTRICT Sorob!e ! XurueeHabu Sakapane Nxai National Nark !! ! Sepako Caecae 2 ! ! S 0 " Konde Ncwima ° 0 ! MAUN 0 ' ! ! ' 0 Ntabi Tshokatshaa ! 0 ° ! " 0 PHDHD Maposa Mmanxotai S Kaore ! ! Maitengwe 2 ! Tsau Segoro -
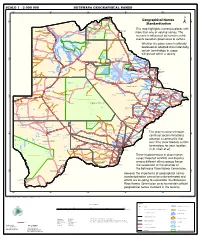
Geographical Names Standardization BOTSWANA GEOGRAPHICAL
SCALE 1 : 2 000 000 BOTSWANA GEOGRAPHICAL NAMES 20°0'0"E 22°0'0"E 24°0'0"E 26°0'0"E 28°0'0"E Kasane e ! ob Ch S Ngoma Bridge S " ! " 0 0 ' ' 0 0 ° Geographical Names ° ! 8 !( 8 1 ! 1 Parakarungu/ Kavimba ti Mbalakalungu ! ± n !( a Kakulwane Pan y K n Ga-Sekao/Kachikaubwe/Kachikabwe Standardization w e a L i/ n d d n o a y ba ! in m Shakawe Ngarange L ! zu ! !(Ghoha/Gcoha Gate we !(! Ng Samochema/Samochima Mpandamatenga/ This map highlights numerous places with Savute/Savuti Chobe National Park !(! Pandamatenga O Gudigwa te ! ! k Savu !( !( a ! v Nxamasere/Ncamasere a n a CHOBE DISTRICT more than one or varying names. The g Zweizwe Pan o an uiq !(! ag ! Sepupa/Sepopa Seronga M ! Savute Marsh Tsodilo !(! Gonutsuga/Gonitsuga scenario is influenced by human-centric Xau dum Nxauxau/Nxaunxau !(! ! Etsha 13 Jao! events based on governance or culture. achira Moan i e a h hw a k K g o n B Cakanaca/Xakanaka Mababe Ta ! u o N r o Moremi Wildlife Reserve Whether the place name is officially X a u ! G Gumare o d o l u OKAVANGO DELTA m m o e ! ti g Sankuyo o bestowed or adopted circumstantially, Qangwa g ! o !(! M Xaxaba/Cacaba B certain terminology in usage Nokaneng ! o r o Nxai National ! e Park n Shorobe a e k n will prevail within a society a Xaxa/Caecae/Xaixai m l e ! C u a n !( a d m a e a a b S c b K h i S " a " e a u T z 0 d ih n D 0 ' u ' m w NGAMILAND DISTRICT y ! Nxai Pan 0 m Tsokotshaa/Tsokatshaa 0 Gcwihabadu C T e Maun ° r ° h e ! 0 0 Ghwihaba/ ! a !( o 2 !( i ata Mmanxotae/Manxotae 2 g Botet N ! Gcwihaba e !( ! Nxharaga/Nxaraga !(! Maitengwe -

Geology and Paragenesis of the Boseto Copper Deposits, Kalahari
GEOLOGY AND PARAGENESIS OF THE BOSETO COPPER DEPOSITS, KALAHARI COPPERBELT, NORTHWEST BOTSWANA by Wesley S. Hall A thesis submitted to the Faculty and the Board of Trustees of the Colorado School of Mines in partial fulfillment of the requirements for the degree of Master of Science (Geology) Golden, Colorado Date _________________________ Signed: ______________________________ Wesley S. Hall Signed: ______________________________ Dr. Murray W. Hitzman Thesis Advisor Golden, Colorado Date _________________________ Signed: ______________________________ Dr. John D. Humphrey Associate Professor and Head Department of Geology & Geological Engineering ii ABSTRACT Detailed lithostratigraphic, structural, and petrographic studies coupled with fluid inclusion and stable isotopic analyses and geochronological studies indicate that the Boseto copper deposits formed initially during diagenesis as metalliferous brines ascended along basin faults and moved along a stratigraphic redox boundary between continental red beds and an overlying reduced marine siliciclastic sequence. The hanging wall rocks to copper-silver ore zones comprise comprises a series of at least three stacked coarsening upwards cycles deposited in a deltaic depositional setting. Early copper mineralization may have been accompanied by regionally extensive albitization. Later multiple pulses of faulting and hydrothermal fluid flow associated with a southeast-vergent folding event in the Ghanzi-Chobe belt resulted in extensive networks of bedding-parallel and discordant quartz-carbonate-(Cu-Fe-sulfide) veins. This contractional deformation-related vein and shear system was responsible for significant remobilization of pre-existing vertically and laterally zoned copper sulfide minerals into high- grade zones by hot (250-300˚C), syn-orogenic, metamorphic-derived hydrothermal fluids. Orientation analysis indicates that the mineralized veins probably formed in association with a flexural slip folding processes. -
Estimating the Level of Economic Activities in Botswana Through Night Light Data
ESTIMATING THE LEVEL OF ECONOMIC ACTIVITIES IN BOTSWANA THROUGH NIGHT LIGHT DATA October 2019 Report by the Centre for Applied Research and Econsult Contents 1 Introduction ................................................................................................................................... 1 2 Literature review ............................................................................................................................ 2 2.1 Nightlights and Economic Activity ......................................................................................... 2 2.1.1 Nightlights and Human Activity .................................................................................... 2 2.1.2 Nightlights and GDP ...................................................................................................... 3 2.1.3 Nightlights and Income Growth .................................................................................... 4 2.1.4 Application of Nightlight Data ...................................................................................... 5 2.2 Application to Environmental Issues ..................................................................................... 6 3 Approach and Methods .................................................................................................................. 8 3.1 Night-Light Data ..................................................................................................................... 8 3.2 National Accounts Data ...................................................................................................... -

Copyright Government of Botswana CHAPTER 69:04
CHAPTER 69:04 - PUBLIC ROADS: SUBSIDIARY LEGISLATION INDEX TO SUBSIDIARY LEGISLATION Declaration of Public Roads and Width of Public Roads Order DECLARATION OF PUBLIC ROADS AND WIDTH OF PUBLIC ROADS ORDER (under section 2 ) (11th March, 1960 ) ARRANGEMENT OF PARAGRAPHS PARAGRAPHS 1. Citation 2. Establishment and declaration of public roads 3. Width of road Schedule G.N. 5, 1960, L.N. 84, 1966, G.N. 46, 1971, S.I. 106, 1971, S.I. 94, 1975, S.I. 95, 1975, S.I. 96, 1975, S.I. 97, 1982, S.I. 98, 1982, S.I. 99, 1982, S.I. 100, 1982, S.I. 53, 1983, S.I. 90, 1983, S.I. 6, 1984, S.I. 7, 1984, S.I. 151, 1985, S.I. 152, 1985. 1. Citation This Order may be cited as the Declaration of Public Roads and Width of Public Roads Order. 2. Establishment and declaration of public roads The roads described in the Schedule hereto are established and declared as public roads. 3. Width of road The width of every road described in the Schedule hereto shall be 30,5 metres on either side of the general run of the road. SCHEDULE Description District Distance in kilometres RAMATLABAMA-LOBATSE Southern South 48,9 East Commencing at the Botswana-South Africa border at Ramatlabama and ending at the southern boundary of Lobatse Township as shown on Plan BP225 deposited with the Director of Surveys and Lands, Gaborone. LOBATSE-GABORONE South East 65,50 Copyright Government of Botswana ("MAIN ROAD") Leaving the statutory township boundary of Lobatse on the western side of the railway and entering the remainder of the farm Knockduff No. -
Republic of Botswana the Project for Enhancing National Forest Monitoring System for the Promotion of Sustainable Natural Resource Management
DEPARTMENT OF FORESTRY AND RANGE RESOURCES (DFRR) MINISTRY OF ENVIRONMENT, NATURAL RESOURCES CONSERVATION AND TOURISM (MENT) REPUBLIC OF BOTSWANA REPUBLIC OF BOTSWANA THE PROJECT FOR ENHANCING NATIONAL FOREST MONITORING SYSTEM FOR THE PROMOTION OF SUSTAINABLE NATURAL RESOURCE MANAGEMENT PROJECT COMPLETION REPORT DECEMBER 2017 JAPAN INTERNATIONAL COOPERATION AGENCY(JICA) ORIENTAL CONSULTANTS GLOBAL CO., LTD. JAPAN FOREST TECHNOLOGY ASSOCIATION GE JR 17-131 DEPARTMENT OF FORESTRY AND RANGE RESOURCES (DFRR) MINISTRY OF ENVIRONMENT, NATURAL RESOURCES CONSERVATION AND TOURISM (MENT) REPUBLIC OF BOTSWANA REPUBLIC OF BOTSWANA THE PROJECT FOR ENHANCING NATIONAL FOREST MONITORING SYSTEM FOR THE PROMOTION OF SUSTAINABLE NATURAL RESOURCE MANAGEMENT PROJECT COMPLETION REPORT DECEMBER 2017 JAPAN INTERNATIONAL COOPERATION AGENCY(JICA) ORIENTAL CONSULTANTS GLOBAL CO., LTD. JAPAN FOREST TECHNOLOGY ASSOCIATION DFRR/JICA: Botswana Forest Distribution Map Zambia Angola Zambia Legend KASANE Angola ! ! Settlement CountryBoundary Riparian Forest Typical Forest Woodland Zimbabwe Zimbabwe Bushland/Shrubland Savanna/Grassland/Forbs MAUN ! NATA Baregorund ! TUTUME ! Desert/Sand Dunes Marsh/Wetland FRANCISTOWN Waterbody/Pan ! ORAPA Namibia ! TONOTA ! GHANZI Angola Zambia Namibia ! SELEBI-PHIKWE BOBONONG ! ! Zimbabwe SEROWE ! PALAPYE ! Namibia MAHALAPYE ! South Africa KANG ! MOLEPOLOLE MOCHUDI ! ! JWANENG ! GABORONE ! ´ 0 50 100 200 RAMOTSWA ! KANYE Kilometres ! Coordinate System: GCS WGS 1984 Datum: WGS 1984 LOBATSE ! Botswana Forest Distribution Map Produced from -

List of Schools Visited for Monitoring Visits
LIST OF SCHOOLS VISITED FOR MONITORING VISITS CENTRAL INSPECTORAL AREA LOCATION NAME OF SCHOOL MMADINARE Diloro Diloro MMADINARE Mmadinare Kelele MMADINARE Kgagodi Kgagodi MMADINARE Mmadinare Mmadinare MMADINARE Mmadinare Phethu Mphoeng MMADINARE Robelela Robelela MMADINARE Gojwane Sedibe MMADINARE Serule Serule MMADINARE Mmadinare Tlapalakoma BOTETI Rakops Etsile BOTETI Khumaga Khumaga BOTETI Khwee Khwee BOTETI Mopipi Manthabakwe BOTETI Mmadikola Mmadikola BOTETI Letlhakane Mokane BOTETI Mokoboxane Mokoboxane BOTETI Mokubilo Mokubilo BOTETI Moreomaoto Moreomaoto BOTETI Mosu Mosu BOTETI Motlopi Motlopi BOTETI Letlhakane Retlhatloleng Selibe Phikwe Selibe Phikwe Boitshoko Selibe Phikwe Selibe Phikwe Boswelakgomo Selibe Phikwe Selibe Phikwe Phikwe Selibe Phikwe Selibe Phikwe Tebogo BOBIRWA Bobonong Bobonong BOBIRWA Gobojango Gobojango BOBIRWA Bobonong Mabumahibidu BOBIRWA Bobonong Madikwe BOBIRWA Mogapi Mogapi BOBIRWA Molalatau Molalatau BOBIRWA Bobonong Rasetimela BOBIRWA Semolale Semolale BOBIRWA Tsetsebye Tsetsebye 1 | P a g e MAHALAPYE WEST Bonwapitse Bonwapitse MAHALAPYE WEST Mahalapye Leetile MAHALAPYE WEST Mokgenene Mokgenene MAHALAPYE WEST Moralane Moralane MAHALAPYE WEST Mosolotshane Mosolotshane MAHALAPYE WEST Otse Setlhamo MAHALAPYE WEST Mahalapye St James MAHALAPYE WEST Mahalapye Tshikinyega MHALAPYE EAST Mahalapye Flowertown MHALAPYE EAST Mahalapye Mahalapye MHALAPYE EAST Matlhako Matlhako MHALAPYE EAST Mmaphashalala Mmaphashalala MHALAPYE EAST Sefhare Mmutle PALAPYE NORTH Goo-Sekgweng Goo-Sekgweng PALAPYE NORTH Goo-Tau Goo-Tau