Program Review for the Lions-Carter Center Sightfirst River Blindness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Districts of Ethiopia
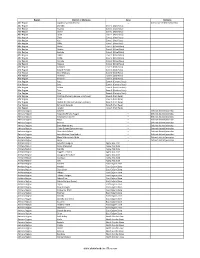
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

Honey Bee Floras Along the Agro-Ecology, Jimma Zone, Southwest Ethiopia
ISSN 2664-4169 (Print) & ISSN 2664-7923 (Online) South Asian Research Journal of Biology and Applied Biosciences Abbreviated Key Title: South Asian Res J Bio Appl Biosci | Volume-3 | Issue-4 | July-Aug -2021 | DOI: 10.36346/sarjbab.2021.v03i04.001 Original Research Article Honey Bee Floras along the Agro-Ecology, Jimma Zone, Southwest Ethiopia Abera Hailu Degaga1*, Minyahel Tilahun1 1College of Agriculture and Natural Resource, Wolkite University, P.O.Box 07, Wolkite, Ethiopia *Corresponding Author Abera Hailu Degaga Email: [email protected] Article History Received: 29.06.2021 Accepted: 03.08.2021 Published: 08.08.2021 Abstract: Ethiopia is home to diverse plant species that provide nectar and pollen as bees forage. In this study, honey bee forages were assessed in three different agro-ecology districts, Jimma Zone, Southwest, Ethiopia. Random sampling techniques was used to collect the data, ninety beekeepers were interviewed using structured questioner. Key informants were interviewed with in all study areas. ANOVA of GLM and Regression were done using Minitab statistical software. Accordingly 42 honey bee’ forages; 28 trees, 6 shrubs and 8 herbs were mentioned by respondents which belong to 22 families, Fabaceae and Asteraceae were the first and second dominant family respectively. Natural forest trees, cultivated crops and fruits were identified as bee forage. Beekeepers experience and their knowledge on seasonal availability of bee forage and honey bee poisonous plants found in their locality were also assessed. In the study area traditional forest beekeeping system is practiced to produce honey. Different bee forages bear flower at different months and visited by honey bees for different number of days. -
Airs Ethiopia Community-Based Irs Model: Comparative Evaluation
PMI | Africa IRS (AIRS) Project Indoor Residual Spraying (IRS 2) Task Order Four AIRS ETHIOPIA COMMUNITY-BASED IRS MODEL: COMPARATIVE EVALUATION MARCH 2013 Recommended Citation: Africa Indoor Residual Spraying Project. March 2013. AIRS Ethiopia. Community-Based IRS Model: Comparative Evaluation. Bethesda, MD. AIRS Project, Abt Associates Inc. Contract: GHN-I-00-09-00013-00 Task Order: AID-OAA-TO-11-00039 Submitted to: United States Agency for International Development/PMI Prepared by: Abt Associates Inc. Abt Associates Inc. I 4550 Montgomery Avenue I Suite 800 North I Bethesda, Maryland 20814 I T. 301.347.5000 I F. 301.913.9061 I www.abtassociates.com AIRS ETHIOPIA COMMUNITY-BASED IRS MODEL: COMPARATIVE EVALUATION MARCH 2013 The views expressed in this document do not necessarily reflect the views of the United States Agency for International Development or the United States Government. CONTENTS Acronyms .................................................................................................................................... v 1. Pilot of Community-Based IRS ............................................................................................. 1 1.1 Introduction ......................................................................................................................................................... 1 1.2 Health Extension Program in Ethiopia ........................................................................................................... 1 1.3 Definition of Two IRS Models ........................................................................................................................ -

The Coffee-Food Security Interface for Subsistence Households in Jimma Zone Ethiopia
The Coffee-Food Security Interface for Subsistence Households in Jimma Zone Ethiopia John C. Beghin Yalem Teshome* North Carolina State University Department of Agricultural and Resource Economics Working Paper No. 17-002 July 2016 The Coffee-Food Security Interface for Subsistence Households in Jimma Zone Ethiopia John C. Beghin Yalem Teshome* Abstract: We investigate food security in three villages in rural Ethiopia for smallholder farmers growing staple crops and coffee, and facing variable coffee and commercial input prices. The surveys were conducted in the coffee growing region of Oromia (Jimma Zone). Commercial input use among these smallholders remains sporadic, although most farmers use them occasionally. A major impediment to systematic usage is the price of these inputs. Policies lowering the unit cost and increasing the local availability of commercial inputs would be useful to systematically boost production and income generation. These smallholders rely on a major coffee cooperative to market their coffee. The cooperative helps with transportation and easing market participation decisions—it provides better prices and some market information. Many farmers rely on credit and banking services offered by the cooperative. The food insecure households are more likely to be led by a female head and to be constrained by extremely small land holdings than food-secure households. These food insecure households tend to work outside of their own farm more often than food-secure households, but in lower-return activities. In our sample, food shortages and household size do not seem to be related, although food shortages are less likely in households with more children. Despite the fast growing economy of Ethiopia, many of these households still face considerable impediments to improve their economic livelihoods and market participation because of bad roads, poor telecommunication infrastructure and limited land. -

Distribution of Head Smudge
Research Article Open Access Journal of Research Article Biomedical Science ISSN: 2690-487X Distribution of Head Smudge (Helminthosporium Miyakei) of Tef Disease During Short Rainy and Main Cropping Seasons in Some Parts of Oromia and Southern Nation Nationality and People Regions of Ethiopia Ashenafi Gemechu Degete* Ethiopian Institute of Agricultural Research (EIAR), Debre Zeit Agricultural Research Center, Ethiopia ABSTRACT Helminthosporium miyakei Head smudge of tef caused by is among the most economically important disease causing significant economic losses of yield and quality. To investigate the distribution of this disease in belg (short rainy) and main (long rainy) seasons in Oromia and SNNP regions, disease assessment survey was conducted in 2019 main season and 2020 belg season from September 25 to May 22-25 G. C. Tef fields were randomly selected at 5-10 km intervals along accessible routes. The result showed head smudge prevalence and intensity varied across locations within the zone and among districts. From a total of forty-two fields surveyed during main and belg seasons (twenty-three fields during the main season and ninteen fields during belg season) were assessed. Quncho was the most prevalent 34.78% and followed by Magna having the prevalence of 26.1% during the main season. Of the assessed areas, the highest incidence was observed in Sokoru districts of Jimma and Wondogenet of West Arsi Zone accounting for about 100% and with the mean severity value of 97%. The highest mean value of incidence was recorded on varieties Tesfa and Quncho with the mean value of 100 and 83.33% followed by local tef variety (80%) during the main cropping season, respectively. -

The Effect of Global Coffee Price Changes on Rural Livelihoods and Natural Resource Management in Ethiopia
The Effect of Global Coffee Price Changes on Rural Livelihoods and Natural Resource Management in Ethiopia A Case Study from Jimma Area Aklilu Amsalu, with Eva Ludi NCCR North-South Dialogue, no. 26 2010 The present study was carried out at the following partner institutions of the NCCR North-South: Overseas Development Institution (ODI) London, UK Department of Geography & Environmental Studies Addis Ababa University, Ethiopia Regional Coordination Office, JACS East Africa Addis Abeba, Ethiopia Swisspeace Bern, Switzerland The NCCR North-South (Research Partnerships for Mitigating Syndromes of Global Change) is one of twenty National Centres of Competence in Research established by the Swiss National Science Foundation (SNSF). It is implemented by the SNSF and co- funded by the Swiss Agency for Development and Cooperation (SDC), and the participating institutions in Switzerland. The NCCR North-South carries out disciplinary, interdisciplinary and transdisciplinary research on issues relating to sustainable development in developing and transition countries as well as in Switzerland. http://www.north-south.unibe.ch The Effect of Global Coffee Price Changes on Rural Livelihoods and Natural Resource Management in Ethiopia A Case Study from Jimma Area Aklilu Amsalu, with Eva Ludi NCCR North-South Dialogue, no. 26 2010 Citation Aklilu Amsalu, Ludi E. 2010. The Effect of Global Coffee Price Changes on Rural Livelihoods and Natural Resource Management in Ethiopia: A Case Study from Jimma Area. NCCR North-South Dialogue 26. Bern, Switzerland: NCCR North-South. Editing Stefan Zach, z.a.ch gmbh, Switzerland Cover photos Left: Typical landscape in the Jimma area – a mosaic of coffee forests and crop land. -

Eastern Nile Technical Regional Office
. EASTERN NILE TECHNICAL REGIONAL OFFICE TRANSBOUNDARY ANALYSIS FINAL COUNTRY REPORT ETHIOPIA September 2006 This report was prepared by a consortium comprising Hydrosult Inc (Canada) the lead company, Tecsult (Canada), DHV (The Netherlands) and their Associates Nile Consult (Egypt), Comatex Nilotica (Sudan) and A and T Consulting (Ethiopia) DISCLAIMER The maps in this Report are provided for the convenience of the reader. The designations employed and the presentation of the material in these maps do not imply the expression of any opinion whatsoever on the part of the Eastern Nile Technical Office (ENTRO) concerning the legal or constitutional status of any Administrative Region, State or Governorate, Country, Territory or Sea Area, or concerning the delimitation of any frontier. WATERSHED MANAGEMENT CRA CONTENTS DISCLAIMER ........................................................................................................ 2 LIST OF ACRONYMS AND ABBREVIATIONS .................................................. viii EXECUTIVE SUMMARY ...................................................................................... x 1. BACKGROUND ................................................................................................ 1 1.1 Introduction ............................................................................................. 1 1.2 Primary Objectives of the Watershed Management CRA ....................... 2 1.3 The Scope and Elements of Sustainable Watershed Management ........ 4 1.3.1 Watersheds and River Basins 4 -

Availability and Utilization of Medical Devices in Jimma Zone Hospitals, Southwest Ethiopia: a Case Study Beyene Wondafrash Ademe1*, Bosena Tebeje2 and Ashagre Molla3
Ademe et al. BMC Health Services Research (2016) 16:287 DOI 10.1186/s12913-016-1523-2 RESEARCH ARTICLE Open Access Availability and utilization of medical devices in Jimma zone hospitals, Southwest Ethiopia: a case study Beyene Wondafrash Ademe1*, Bosena Tebeje2 and Ashagre Molla3 Abstract Background: Health systems throughout the world, whether in developed or developing countries, are struggling with the challenge of how to manage health-care delivery in conditions of resource constraint. The availability and utilization of various health care equipments at all levels of the health care system has been emphasized for effective and efficient service delivery. In Ethiopia lack of proper management of medical equipment limited the capacity of health institutions to deliver adequate health care. The main objective of this study was to assess availability and utilization of medical devices and identify reported reasons that affect availability and utilization of medical devices among hospitals in Jimma Zone. Methods: A cross-sectional multiple case-study using mixed quantitative and qualitative methods was used. Three hospitals of Jimma Zone were included in the study. Adapted and pre-tested structured English version checklist for availability and utilization of medical equipment and document review as well as interview guide for in-depth interview were used for data collection. Data were collected by observation of availability of the devices, interviewing selected professionals and document review of health care services using devices in the study hospitals. Data were analyzed using SPSS 16.0 statistical software. Descriptive analysis was made to determine the availability and functional status of medical devices. For qualitative part responses were transcribed, categorized and thematically analyzed. -

Federal Democratic Republic of Ethiopia Project for Supporting Sustainable Forest Management Through REDD+ and Certified Forest Coffee Production and Promotion
Federal Democratic Republic of Ethiopia Oromia Environment Forest and Climate Change Authority (OEFCCA) Oromia Forest and Wildlife Enterprise (OFWE) Federal Democratic Republic of Ethiopia Project for Supporting Sustainable Forest Management through REDD+ and Certified Forest Coffee Production and Promotion Project Completion Report November 2020 Japan International Cooperation Agency Japan International Forest Promotion and Cooperation Center Appropriate Agriculture International Co., LTD GE JR 20-076 Federal Democratic Republic of Ethiopia Project for Supporting Sustainable Forest Management through REDD+ and Certified Forest Coffee Production and Promotion Project Completion Report Table of Contents Map List of Abbreviation Summary ....................................................................................................................... 1 Chapter 1 Outline of the Project .................................................................................... 7 1-1 Background of the Project .................................................................................... 7 1-2 Objectives of the Project ...................................................................................... 8 1-3 Target of the Project ............................................................................................ 8 1-4 Implementation Agency ....................................................................................... 8 1-5 Input for the Project ............................................................................................ -

Enabling Successful Migration for Youth in Addis Ababa Quantitative Survey
Enabling Successful Migration for Youth in Addis Ababa Quantitative Survey Z1 Respondent Code Sequential number according to order of the respondent (101, 102, 103, etc.) Z2 Interviewer Code Z3 Date of Interview (DD/MM/YY) / / 1 8 Z4 Location Code Based on site Z5 Start time of Interview (according to Western clock) : CONSENT: Did you complete the entire verbal script for consent, answer all questions from the respondent, and and receive a fully informed consent to participate? Investigator name: Investigator Signature: Are you willing to go ahead? Yes → continue to A1 No → stop the survey, thank the respondent, and approach another potential respondent 1 I. DEMOGRAPHIC CHARACTERISTICS A1 How old are you? Enter age A2 Sex 0 = male 1 = female 8 = don’t know 9 = refused to answer A3 Where in Ethiopia are you from? Enter code for region Enter code for zone Enter name of woreda Enter name of kebele A4 Where in Addis Ababa do you live? Enter code for subcity Enter name of district A5 Which year did you first arrive in Enter year (according to Western Addis? calendar, not Ethiopian) A6 How much time (cumulative) have Enter total number of months you spent in Addis Ababa? A7 What is your marital status? 1 = married 2 = engaged, 3 = in a partnership 4 = single 5 = widowed 6 = divorced/separated 8 = don’t know 9 = refused to answer A8 Do you have any children? 0 = no 1 = yes 8 = don’t know 9 = refused to answer A9 What is your religion? 1 = Ethiopian Orthodox 2 = Muslim 3 = Protestant 4 = Traditional/local 5 = Catholic 6 = Other 8 = Don’t know -

Annual Report 2019
>> ANNUAL REPORT, PROJECT 200452, MARCH 31ST, 2020 ANNUAL REPORT 2019 STRENGTHENING THE HEALTH SYSTEM IN JIMMA ZONE (OROMIA REGION, ETHIOPIA) THROUGH PERFORMANCE BASED FINANCING (2019-2023) MARCH 31ST, 2020, THE HAGUE, THE NETHERLANDS INGE BARMENTLO POLITE DUBE MOSES MUNYUMAHORO MAARTEN ORANJE CARMEN SCHAKEL ANNUAL REPORT 2019 - STRENGTHENING THE HEALTH SYSTEM IN JIMMA ZONE, ETHIOPIA MARCH 2020 © CORDAID 2 ANNUAL REPORT 2019 - STRENGTHENING THE HEALTH SYSTEM IN JIMMA ZONE, ETHIOPIA TABLE OF CONTENTS LIST OF ABBREVIATIONS ................................................................................................ 4 EXECUTIVE SUMMARY ..................................................................................................... 5 PROJECT BACKGROUND ................................................................................................. 8 1. OUTCOME 1: IMPROVED HEALTH SERVICE DELIVERY ........................................... 9 2. OUTCOME 2: IMPROVED GOVERNANCE OF HEALTH SERVICE DELIVERY ......... 57 3. OUTCOME 3: AN ENHANCED HEALTH INFORMATION SYSTEM............................ 61 CONCLUSIONS ................................................................................................................ 63 ANNEXES ......................................................................................................................... 66 Annex 1: Theory of Change (From: Original Proposal PBF Jimma Zone, October 2018)................. 67 Annex 2: Logical Framework (From: Original Proposal PBF Jimma Zone, October 2018) -

Determinants of Health Service Utilization
abetes & Di M f e o t a l b a o n l r i s u m o J Journal of Diabetes and Metabolism Amente and Kebede, J Diabetes Metab 2016, 7:11 ISSN: 2155-6156 DOI: 10.4172/2155-6156.1000713 Research Article Open Access Determinants of Health Service Utilization among Older Adults in Bedele Town, Illubabor Zone, Ethiopia Tadele Amente* and Birtukan Kebede Wollega University, Ethiopia *Corresponding author: Tadele Amente, Wollega University, Ethiopia, Tel: +251886228264; E-mail: [email protected] Received date: Oct 21, 2016; Accepted date: Nov 03, 2016; Published date: Nov 10, 2016 Copyright: © 2016 Amente T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: In any country use of health services by elderly could vary according to the cultural, social, economic and demographic situation of the person who may need care. In certain contexts, it particularly varies with age and sex of the potential service user. However, studies that document on health service utilization among elderly population are generally scarce in Ethiopia and particularly, in the study area. Objective: This study aimed to assess utilization of health services and associated factors among population of older adults. Methods: A community based cross sectional study carried on 284 elderly populations residing in Bedele Town from February-March 2013 by using a structured questioner interview by four trained high school students through simple random sampling technique in all kebeles of the Town.