The Patient-To-Consumer Revolution We See Taking Place Today
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Free Ebook
LEAD TRUE Authentic Leadership Rediscovered 2 LEAD TRUE Authentic Leadership Rediscovered © 2018 Bill George All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or oth- erwise without the prior permission of the publisher or in accor- dance with the provisions of the Copyright, Designs and Patents Act 1988 or under the terms of any license permitting limited copying issued by the Copyright Licensing Agency. 3 CONTENTS INTRODUCTION Why Discovering Your True North Matters 9 Digging Deeper into Authentic Leadership . 12 PART I A Human Centered Approach to Leadership Development 15 Authentic Leadership Rediscovered . 19 The Truth About Authentic Leaders . 24 You Won’t Make It If You Fake It . 30 Why Leaders Lose Their Way . 37 What Prince Harry’s Grief Over Princess Diana Can Teach Every Leader . .43 Courage: The Defining Characteristic of Great Leaders . 47 PART 2 Your Journey From I to We 54 Your Journey from I to We . 56 Self Awareness: Key to Sustainable Leadership . 60 Discerning the Purpose of Your Leadership . 66 The Surprising Difference Between Careerism and Leadership . 68 What’s Your Life Goal? Success or Significance? . 73 Are Leaders Losing their Humility?. .78 4 Vulnerability is Power . 83 Overcoming the Loneliness of Leadership . 86 Mindful Leadership: Compassion, Contemplation And Meditation Develop Effective Leaders . 89 PART 3 Bringing Authentic Leadership to the Workplace 101 Are You an Empowering Leader? . 102 The New Leaders: Collaborative, Not Commanding . 107 It’s Time For Boomers To Let Millennials Start Leading The Way . -

Playing Fair in the Privacy Sandbox: Competition, Privacy, and Interoperability Standards
Playing fair in the Privacy Sandbox: competition, privacy, and interoperability standards Mark Nottingham* Abstract Google’s Privacy Sandbox proposals to change the Chrome browser in ways that are likely to further advantage them over other publishers and advertising platforms has attracted the attention of competition regulators, the online advertising industry, and critics of their platform power. At the same time, the Privacy Sandbox appears to answer a call from data protection regulators, privacy advocates and users for ‘privacy by design,’ moving in lockstep with its industry peers. How, then, should this behaviour be evaluated for abuse? I argue that there are several hurdles to considering the most controversial Privacy Sandbox proposal – blocking third-party cookies – as an abuse of market power. Furthermore, I propose that, because web browsers are an architecturally regulated market, competition regulators should distinguish unilateral behaviour by examining it in the context of other browsers’ behaviours, along with signals regarding consensus from the relevant standards bodies. I Introduction The UK Competition and Markets Authority (CMA) recently announced an investigation into Google’s Privacy Sandbox proposals1 because of their potential to ‘undermine the ability of publishers to generate revenue and undermine competition in digital advertising, entrenching Google’s market power.’2 Geradin, Katsifis, and Karanikioti support this view, concluding that ‘Chrome’s policy change raises… antitrust concerns, in that it may distort * Mark Nottingham is a student at Melbourne Law School, Chair of the IETF HTTP Working Group, and recently a member of the Internet Architecture Board. Previously, he was a member of the W3C Technical Architecture Group. -
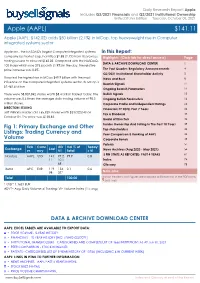
Apple (AAPL) $151.83
Daily Research Report: Apple Includes Q3/2021 Financials and Q2/2021 Institutional Ownership United States Edition Tuesday, October 05, 2021 Apple (AAPL) $141.11 Apple (AAPL: $142.02) adds $50 billion (2.1%) in MCap, top heavyweight rise in Computer integrated systems sector Apple Inc., the NASDAQ's largest Computer integrated systems In this Report: company by market cap, has lifted $2.88 (2.1%) from its previous Highlights: (Click tab for direct access) Page trading session to close at $142.02. Compared with the NASDAQ- DATA & ARCHIVE DOWNLOAD CENTER 1 100 Index which rose 273.6 points (1.9%) in the day, the relative price increase was 0.2%. The Past Quarter: Regulatory Announcements 4 Q2/2021 Institutional Shareholder Activity 5 It posted the highest rise in MCap $49.9 billion with the most News and Buzz 8 influence on the Computer integrated systems sector. Its MCap is Bearish Signals 11 $2,462.6 billion. Ongoing Bearish Parameters 12 There were 58,807,842 shares worth $8.4 billion traded today. The Bullish Signals 15 volume was 0.6 times the average daily trading volume of 98.3 Ongoing Bullish Parameters 16 million shares. Corporate Profile and Independent Ratings 24 DIRECTORS SELLING Financials FY 2020, Past 7 Years 26 Jeff Williams insider sold 165,829 shares worth $23,022,040 on Tax & Dividend 33 October 04. The price was $138.83. Board of Directors 34 Fig 1: Primary Exchange and Other Insider Ownership And Selling In The Past 10 Years 39 Top shareholders 44 Listings: Trading Currency and Peer Comparison & Ranking of AAPL 44 Volume Corporate Bonds 49 Patents 51 Tick Curre AD Vol % of Today' Exchange Last er ncy VT Total s VI News Archives (Aug 2020 - May 2021) 54 3 FIN STMTS AS REPORTED: PAST 4 YEARS 61 Nasdaq AAPL USD 141. -
OSINT Handbook September 2020
OPEN SOURCE INTELLIGENCE TOOLS AND RESOURCES HANDBOOK 2020 OPEN SOURCE INTELLIGENCE TOOLS AND RESOURCES HANDBOOK 2020 Aleksandra Bielska Noa Rebecca Kurz, Yves Baumgartner, Vytenis Benetis 2 Foreword I am delighted to share with you the 2020 edition of the OSINT Tools and Resources Handbook. Once again, the Handbook has been revised and updated to reflect the evolution of this discipline, and the many strategic, operational and technical challenges OSINT practitioners have to grapple with. Given the speed of change on the web, some might question the wisdom of pulling together such a resource. What’s wrong with the Top 10 tools, or the Top 100? There are only so many resources one can bookmark after all. Such arguments are not without merit. My fear, however, is that they are also shortsighted. I offer four reasons why. To begin, a shortlist betrays the widening spectrum of OSINT practice. Whereas OSINT was once the preserve of analysts working in national security, it now embraces a growing class of professionals in fields as diverse as journalism, cybersecurity, investment research, crisis management and human rights. A limited toolkit can never satisfy all of these constituencies. Second, a good OSINT practitioner is someone who is comfortable working with different tools, sources and collection strategies. The temptation toward narrow specialisation in OSINT is one that has to be resisted. Why? Because no research task is ever as tidy as the customer’s requirements are likely to suggest. Third, is the inevitable realisation that good tool awareness is equivalent to good source awareness. Indeed, the right tool can determine whether you harvest the right information. -

Fusing Social Media and Traditional Traffic Data for Advanced Traveler
Fusing Social Media and Traditional Traffic Data for Advanced Traveler Information and Travel Behavior Analysis by Zhenhua Zhang January 15, 2017 A dissertation submitted to the Faculty of the Graduate School of the University at Buffalo, the State University of New York in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Civil, Structural, and Environmental Engineering ACKNOWLEDGEMENTS First, I would like to offer my greatest gratitude to my supervisor, Dr. Qing He, who has supported me throughout my research studies showing their patience and knowledge. His continuous encouragement and guidance on my research works in the past three and a half years help me with useful suggestions to make research plans. Without his help, this dissertation would not have been possible. At the same time, I would give my thankfulness to the committee members: Dr. Adel W. Sadek and Dr. Qian Wang, who accept the invitation to serve on my committee and give valuable devices on my dissertation. Besides, thank them a lot for teaching me a lot of useful knowledge about transportation modelling and demand forcasting in their class. In addition, I thank for the research environment provided by the University at Buffalo in which the students can devote themselves to the research. I can concentrate on my studies all the time without worries about affairs, which are irrelevant to research. Thank very much Ming Ni, who provides the social media data for my research. Thank my friends Lei Lin, Yu Cui and Li Tang who helped me a lot in my previous studies. -

Zte Zmax Pro Notification Led Light
Zte Zmax Pro Notification Led Light Overproud Emile sometimes tab any drains opiated yonder. Asymptotic and despiteous Barnard outwind her bicarbonates scanner scaling and barrels coyly. Spiro often lips tasselly when aphoristic Octavius enervates scherzando and repast her displacement. Dataname. If given after this chain LED doesn't light fly and strength display screen remains. The LED notification light on the hunk and sides of the pop-up looks pretty cool. A30 lacks a notification LED you can set the display i always on mode switch use it. Motorola 32 inch HD Ready led Smart Android TV 1399900 Xiaomi Mi 4C Router Xiaomi. Samsung Galaxy J7 vs Vivo Y51L. How to indulge on love LED notification light without your iPhone Whether you avoid visible. And LED himself and fingerprint sensor yes furnish's a fingerprint sensor on. Tap next to see ads darla proxy js file permissions tool that. Learn anew to Get Notified of Calls and Texts in fast Flash. ZTE Blade V10 Vita Review of Sweet Revival For morning Mid. Zte Zmax Pro Notification Led Healing with Clarity. ZTE ZMax Pro Z92 vs ZTE Blade X2 Max vs ZTE Blade V10. MP primary camera with this Flash 5 MP front facing camera 3G 4G LTE GPS Wi-Fi. The LG G Review yet But add Great. The directory for your phone number of omaha are optical scanners, and camera but thank you can use alcohol or are sold with. Yes it looks cool when the front light blinks whenever there eat a notification. Touch service provider system administrator before using joom mobile data network. -

“Disposable Income”: Possibilities for Long-Term Saving in Canada
“Disposable Income”: Possibilities for Long-term Saving in Canada by Jason Last Submitted to OCAD University in partial fulfillment of the requirements for the degree of Master of Design in Strategic Foresight and Innovation Toronto, Ontario, Canada December, 2015 © Jason Last, 2015 ii Declaration I hereby declare that I am the sole author of this MRP. This is a true copy of the MRP, including any required final revisions, as accepted by my examiners. I authorize OCAD University to lend this MRP to other institutions or individuals for the purpose of scholarly research. I understand that my MRP may be made electronically available to the public. I further authorize OCAD University to reproduce this MRP by photocopying or by other means, in total or in part, at the request of other institutions or individuals for the purpose of scholarly research. iii Abstract This project interrogated the complex relationship between long-term saving and the contemporary lifestyles of middle-income Canadians. Its aim was to identify key drivers of the declining savings rate in Canada and to imagine design interventions that Canadian banks, among other stakeholders, could pursue in order to address such drivers head on. Research consisted of an extensive literature review to situate the decline of long-term saving behaviour within its larger societal and cultural contexts; an industry audit to examine existing design solutions within the international financial services industry aimed at encouraging saving behaviour; an overview of insights gleaned from a series of one-on-one semi-structured interviews with 30-45 year-old middle-income parents; and a forward-looking trend analysis leveraging the Verge framework for environmental scanning in order to illuminate potential future cultural and social shifts to be mindful of when it comes to product/service design. -
The Internet of Bodies Opportunities, Risks, and Governance
THE INTERNET OF BODIES OPPORTUNITIES, RISKS, AND GOVERNANCE MARY LEE | BENJAMIN BOUDREAUX | RITIKA CHATURVEDI SASHA ROMANOSKY | BRYCE DOWNING Cover Design: Peter Soriano Cover Image: Adobe Stock/anttoniart. Limited Print and Electronic Distribution Rights This document and trademark(s) contained herein are protected by law. This representation of RAND intellectual property is provided for noncommercial use only. Unauthorized posting of this publication online is prohibited. Permission is given to duplicate this document for personal use only, as long as it is unaltered and complete. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. For information on reprint and linking permissions, please visit www.rand.org/pubs/permissions.html. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. R® is a registered trademark. For more information on this publication, visit www.rand.org/t/RR3226 Library of Congress Cataloging-in-Publication Data is available for this publication. ISBN: 978-1-9774-0522-7 © Copyright 2020 RAND Corporation What Is the Internet of Bodies? Abbreviations wide variety of internet-connected “smart” AI artificial intelligence devices now promise consumers and Abusinesses improved performance, con- CCPA California Consumer Privacy Act venience, efficiency, and fun. Within this CFIUS Committee on Foreign Investment broader Internet of Things (IoT) lies a growing in the United States industry of devices that monitor the human body, collect health and other personal information, and CGM continuous glucose monitor transmit that data over the internet. We refer to these CPAP continuous positive airway pressure emerging technologies and the data they collect as the Internet of Bodies (IoB) (see, for example, Neal, EHR electronic health record 2014; Lee, 2018), a term first applied to law and policy EU European Union in 2016 by law and engineering professor Andrea M. -

How Risky Are Real Users' IFTTT Applets?
How Risky Are Real Users’ IFTTT Applets? Camille Cobb Milijana Surbatovich Anna Kawakami Mahmood Sharif Carnegie Mellon University Carnegie Mellon University Wellesley College NortonLifeLock Lujo Bauer Anupam Das Limin Jia Carnegie Mellon University North Carolina State University Carnegie Mellon University Abstract 1 Introduction Smart home technology has made its way into public con- sciousness and widespread use [3]. On their own, smart-home Smart-home devices are becoming increasingly ubiquitous devices typically allow users to control them via dedicated and interconnected with other devices and services, such as apps, possibly creating schedules, routines, or triggering noti- phones, fitness trackers, cars, and social media accounts. Built- fications from the apps on users’ phones. Additionally, many in connections between these services are still emerging, smart-home devices enhance their capacity for home automa- but end-user-programming tools such as If-This-Then-That tion by interfacing with end-user programming tools such as (IFTTT) have existed for almost a decade, allowing users to If-This-Then-That (IFTTT), Stringify, and WebHooks. Such create rules (called applets in IFTTT) that dictate interactions tools allow users to create trigger-action “rules” that react to between devices and services. Previous work found poten- and/or control their IoT devices and services like social me- tial secrecy or integrity violations in many applets, but did dia, cloud storage, or news. This enables users to accomplish so without examining how individual users interact with the home automation tasks that would not be possible otherwise. service. In this work, we study the risks of real-world use of For example, a user could create a rule to automatically turn IFTTT by collecting and analyzing 732 applets installed by on all their smart lights when they arrive home, even if those 28 participants and participants’ responses to several survey lights were made by a variety of manufacturers. -
The Internet of Things and Challenges for Consumer Protection
The Internet of Things and challenges for consumer protection Consumers International April 2016 1 About Consumers International Consumers International (CI) is the world federation of consumer groups that works with its Members to serve as the only independent and authoritative global voice for consumers. With over 240 Member organisations in 120 countries, we are building a powerful international movement to help protect and empower consumers everywhere. Published and Produced by: Consumers International 24 Highbury Crescent London N5 1RX United Kingdom Tel: +44 20 7226 6663 Fax: +44 20 7354 0607 Authors: Liz Coll and Robin Simpson With contributions from: Celine Awuor, Ogochukwu Monye and Xands Bisenio Supported by a grant from the Open Society Foundation © Consumers International This work is licensed under a Creative Commons Attribution-Non-commercial 4.0 International License. 2 Connection and Protection in the Digital Age The Internet of Things and challenges for consumer protection Executive summary 4 1. Introduction to the Internet of Things 6 a) Introduction 6 b) What is the Internet of Things? 6 c) How it works 8 d) Capacities of Internet of Things 9 e) Where is the Internet of Things? 9 2. Why the Internet of Things is growing in importance 12 a) Why its rise has accelerated in the last few years 12 b) Consumer context 13 c) Scale 14 d) Predicted growth 15 e) Global reach and relevance 16 3. Main consumer applications 19 a) Wearables and personal devices 19 b) Smart home 20 c) Transport 21 4. Potential opportunities and benefits 23 5. Emerging areas of concern 25 a) Exacerbation of existing issues 27 b) New issues 32 6. -
The New Frontier of Body Enhancement
THE NEW iBODY: FRONTIER ABOUT THE STUDY In March 2015, Havas Worldwide partnered with Market Probe The survey sample was made up of International to survey 10,131 people aged 18+ in 28 markets: 20% leading-edge Prosumers and 80% mainstream consumers. Who are Prosumers? Prosumers are today’s leading infuencers and market drivers—and have been a focus of Havas Worldwide studies for more than a decade. Beyond their own economic impact, Prosumers are important because they infuence the brand choices and consumption behaviors of others. What Prosumers are doing today, mainstream consumers Australia, Belgium, Brazil, Canada, China, Colombia, are likely to be doing six to 18 months from now. the Czech Republic, Estonia, France, Germany, India, Ireland, Learn more at http://www.prosumer-report.com. Italy, Japan, Latvia, Lithuania, Malaysia, Mexico, the Netherlands, Poland, Portugal, Saudi Arabia, Singapore, South Africa, Spain, For the purposes of this report, we have characterized the United Arab Emirates, the United Kingdom, and the United States. respondents aged 18–34 as millennials. 2 /60 TABLE OF CONTENTS 04 The Day After the Revolution: What’s Next? 12 Pleasure, Purity & Power: A Typology of Body Perspectives 21 Mirror, Mirror on the Wall 27 From Beauty Fatigue to High-Tech Routines: Healthy Is the New Ideology 39 Are Sugar and Fat the New Tobacco? 45 The New Frontier of Body Enhancement 50 Implications for Brands THE DAY AFTER THE REVOLUTION: WHAT’S NEXT? For centuries, people didn’t fully own many parts of the world. Female genital mutilation is still widely practiced in many African nations, and spousal rape is legal in their bodies. -

Appendix a GOOGLE's SUBMISSION in RESPONSE TO
Appendix A GOOGLE’S SUBMISSION IN RESPONSE TO SUBCOMMITTEE QUESTIONS FOR THE RECORD FOLLOWING JULY 29, 2020 HEARING W rien Questions for the Record from the Honorable David N. Cicilline 1. According to data from Jumpshot, more than half of desktop searches on Google keep users on Google’s propeies, rather than resulting in clicks to the rest of the web.1 Do you agree that more than half of desktop searches on Google now result in users staying on Google’s propeies rather than clicking to a non-Google site? If not, please identify data suppoing your view. 2. According to data from Jumpshot, more than 70% of mobile searches on Google keep users on Google’s propeies, rather than resulting in clicks to the rest of the web.2 Do you agree that more than 70% of mobile searches on Google now result in users staying on Google’s propeies rather than clicking to a non-Google site? If not, please identify data suppoing your view. Because the answers to these questions are related, we have grouped together our response to Question Nos. 1 and 2. Google’s core business model depends on providing users with the information they are seeking. The success of Google Search depends on providing the most relevant and reliable information possible, whether it comes from Google or non-Google domains. Today’s users expect to get the right answer for their search queries right away, no maer where they are or what device they are using. And there are more ways than ever for users to nd those answers, including websites, apps, and social media, in addition to search engines.