Meghalaya Health Systems Strengthening Project Environmental and Social Management Framework Executive Summary
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Meghalaya Receives Agriculture Award Meghalaya Receives
March, 2018 MEGNEWS MEGNEWSMONTHTLY NEWS BULLETIN A PUBLICATION OF THE DIRECTORATE OF INFORMATION & PUBLIC RELATIONS, MEGHALAYA TOLL - FREE DATE: March 29, 2018 FOR FREE DISTRIBUTION ISSUE NO. 104 NO. - 1800-345-3644 CM attends Natural CM attends International CM urges Youth to Workshop on Continuing Two-Day Mega Health Swearing - in Ceremony On the Lighter Side Resource Management Inter-Disciplinary Seminar look for opportunities Professional Development Mela Concludes of New CM and Cabinet and Climate Change Meet beyond State at Regional of Counsellors Ministers at Tura 2 3 Colloquium 4 5 6 7 8 Meghalaya Receives Agriculture award Prime Minister, Shri. Narendra Modi on 17th March 2018 awarded Meghalaya an award, which was possible because of the hard work of the farmers and the for its growth in the agriculture sector. Chief Minister of Meghalaya, Shri. officials of the Department of Agriculture and other stakeholders. Shri. Modi Conrad K. Sangma received the award on behalf of the people of the State in handed over the award to the Chief Minister during the Krishi Unnati Mela presence of Agriculture Minister, Shri. Banteidor Lyngdoh. held at India Agriculture Research Institute Mela Groud at Pusa in New Delhi. Addressing the gathering, the Prime Minister said that such Unnati Melas The Chief Minister has dedicated the award to the people of the State especially play a key role in paving the way for New India. He said that today, he has farmers. “It gives an immense pleasure that I have received the award on behalf the opportunity to simultaneously speak to two sentinels of New India – of the farmers of the State, who have scripted a success story. -

Urban Development
MMEGHALAYAEGHALAYA SSTATETATE DEVELOPMENTDEVELOPMENT RREPORTEPORT CHAPTER VIII URBAN DEVELOPMENT 8.1. Introducti on Urbanizati on in Meghalaya has maintained a steady growth. As per 2001 Census, the state has only 19.58% urban populati on, which is much lower than the nati onal average of 28%. Majority of people of the State conti nue to live in the rural areas and the same has also been highlighted in the previous chapter. As the urban scenario is a refl ecti on of the level of industrializati on, commercializati on, increase in producti vity, employment generati on, other infrastructure development of any state, this clearly refl ects that the economic development in the state as a whole has been rather poor. Though urbanizati on poses many challenges to the city dwellers and administrators, there is no denying the fact that the process of urbanizati on not only brings economic prosperity but also sets the way for a bett er quality of life. Urban areas are the nerve centres of growth and development and are important to their regions in more than one way. The current secti on presents an overview of the urban scenario of the state. 88.2..2. UUrbanrban sseett llementement andand iitsts ggrowthrowth iinn tthehe sstatetate Presently the State has 16 (sixteen) urban centres, predominant being the Shillong Urban Agglomerati on (UA). The Shillong Urban Agglomerati on comprises of 7(seven) towns viz. Shillong Municipality, Shillong Cantonment and fi ve census towns of Mawlai, Nongthymmai, Pynthorumkhrah, Madanrti ng and Nongmynsong with the administrati on vested in a Municipal Board and a Cantonment Board in case of Shillong municipal and Shillong cantonment areas and Town Dorbars or local traditi onal Dorbars in case of the other towns of the agglomerati on. -

Meghalaya S.No
Meghalaya S.No. District Name of the Establishment Address Major Activity Description Broad NIC Owner Emplo Code Activit ship yment y Code Code Class Interva l 107C.M.C.L STAR CEMENT 17 LUMSHNONG, JAINTIA FMANUFACTURE OF 06 325 4 >=500 INDUSTRIES LTD HILLS 793200 CEMENT 207HILLS CEMENTS 11 MYNKRE, JAINTIA MANUFACTURE OF 06 239 4 >=500 COMPANY INDUSTRIES HILLS 793200 CEMENT LIMITED 307AMRIT CEMENT 17 UMLAPER JAINTIA -MANUFACTURE OF 06 325 4 >=500 INDUSTRIES LTD HILLS 793200 CEMENT 407MCL TOPCEM CEMENT 99 THANGSKAI JAINTIA MANUFACTURE OF 06 239 4 >=500 INDUSTRIES LTD HILLS 793200 CEMENT 506RANGER SECURITY & 74(1) MAWLAI EMPLOYMENT SERVICE 19 781 2 >=500 SERVICE ORGANISATION, MAWAPKHAW, SHILLONG,EKH,MEGHALA YA 793008 606MEECL 4 ELECTRICITY SUPPLIER 07 351 4 >=500 LUMJINGSHAI,POLO,SHILL ONG,EAST LAWMALI KHASI HILLS,MEGHALAYA 793001 706MEGHALAYA ENERGY ELECTRICITY SUPPLY 07 351 4 >=500 CORPORATION LTD. POLO,LUMJINGSHAI,SHILL ONG,EAST KHASI HILLS,MEGHALAYA 793001 806CIVIL HOSPITAL 43 BARIK,EAST KHASI HOSPITAL 21 861 1 >=500 SHILLONG HILLS,MEGHALAYA 793004 906S.S. NET COM 78(1) CLEVE COLONY, INFORMATION AND 15 582 2 200-499 SHILLONG CLEVE COMMUNICATION COLONY EAST KHASI HILLS 793001 10 06 MCCL OFFICE SOHSHIRA 38 BHOLAGANJ C&RD MANUFACTURE OF 06 239 4 200-499 MAWMLUH SHELLA BLOCK EAST KHASI HI CEMENT MAWMLUH LLS DISTRICT MEGHALAYA 793108 11 06 MCCL SALE OFFICE MAWMLUH 793108 SALE OFFICE MCCL 11 466 4 200-499 12 06 DR H.GORDON ROBERTS 91 JAIAW HOSPITAL HEALTH 21 861 2 200-499 HOSPITAL PDENG,SHILLONG,EAST SERVICES KHASI HILLS,MEGHALAYA 793002 13 06 GANESH DAS 47 SHILLONG,EAST KHASI RESIDENTIAL CARE 21 861 1 200-499 HOSPITAL,LAWMALI HILLS MEGHALAYA ACTIVITIES FORWOMEN 793001 AND CHILDREN 14 06 BETHANY HOSPITAL 22(3) NONGRIM HOSPITAL 21 861 2 200-499 HILLS,SHILLONG,EAST KHASI HILLS,MEGHALAYA 793003 15 06 GENERAL POST OFFICE 12 KACHERI ROAD, POSTAL SERVICES 13 531 1 200-499 SHILLONG KACHERI ROAD EAST KHASI HILLS 793001 16 06 EMERGENCY 19(1) AMBULANCE SERVICES. -
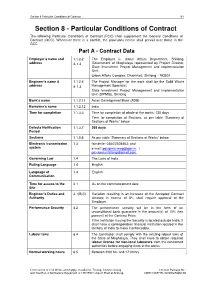
Nerccdiptr- 02Shgswm-08-Section-8
Section 8 Particular Conditions of Contract 8-1 Section 8 - Particular Conditions of Contract The following Particular Conditions of Contract (PCC) shall supplement the General Conditions of Contract (GCC). Whenever there is a conflict, the provisions herein shall prevail over those in the GCC. Part A - Contract Data Employer’s name and 1.1.2.2 The Employer is: Urban Affairs Department, Shillong, address & 1.3 Government of Meghalaya represented by Project Director, State Investment Project Management and Implementation Unit, Urban Affairs Complex, Dhankheti, Shillong - 793001 Engineer’s name & 1.1.2.4 The Project Manager for the work shall be the Solid Waste address & 1.3 Management Specialist State Investment Project Management and Implementation Unit (SIPMIU), Shillong Bank’s name 1.1.2.11 Asian Development Bank (ADB) Borrower’s name 1.1.2.12 India Time for completion 1.1.3.3 Time for completion of whole of the works: 730 days Time for completion of Sections: as per table “Summary of Sections of Works” below Defects Notification 1.1.3.7 365 days Period Sections 1.1.5.6 As per table “Summary of Sections of Works” below Electronic transmission 1.3 facsimile: 0364/2505463; and system e-mail: [email protected]. / [email protected]. Governing Law 1.4 The Laws of India Ruling Language 1.4 English Language of 1.4 English Communication Time for access to the 2.1 As on the commencement date. Site Engineer’s Duties and 3.1(B)(ii) Variation resulting in an increase of the Accepted Contract Authority Amount in excess of 5% shall require approval of the Employer. -

ORDER 1. Entry of Tourists from Outside the State Shall Not Be
GOVERNMENT OF MEGHALAYA HOME (POLITICAL) DEPARTMENT No. POL.75/2020/Pti/100 Dated, Shillong the 28" May, 2021 ORDER Whereas, it is observed that the number of COVID-19 cases in the State continues to rise sharply and hospital bed occupancy is nearing saturation; Therefore, in supersession to all orders issued in respect of Containment Measures in the State, the following shall be enforced in the State w.e.f. 318t May, 2021 until further orders. Entire State: 1. Political, public, social and religious gatherings are not permitted including conferences, meetings and trainings Entry of tourists from outside the State shall not be permitted and all tourist spots shall remain closed. Sports activities are not permitted. Inter-State movement of persons shall be restricted. This shall not apply for transit vehicles of Assam / Tripura / Manipur / Mizoram. 5. International Border Trade shall be regulated by the Deputy Commissioners. East Khasi Hills District: 6. Lockdown shall be extended in East Khasi Hills District till 5:00 AM of 7'" June, 2021. 7. The Deputy Commissioner, East Khasi Hills District shall make suitable arrangements for availability of essential commodities in the localities on need basis. 8. Home Delivery Services are permitted subject to prior permission and regulation by the Deputy Commissioner, East Khasi Hills District. 9. Inter-district movement of persons from and to East Khasi Hills District shall be restricted. 10. All Central Government offices other than those notified by Home (Political) Department vide Notification No. POL.117/2020/Pt.1I/136, dated 28-05-2021 shall remain closed. 11. All State Government offices other than those notified by Personnel & A.R (A) Department vide Notification No. -

Household Population by Religion of Head of Household, Series-14
CENSUS OF INDIA 1981 SERIES-14 PAPER 1 OF 1985 MEGHALAYA (UP TO C.D. BLOCK HOUSEHOLD POPULATION AND TOWN LEVEL) BY RELIGION OF HEAD OF HOUSEHOLD ]. TAYA'NG, OJ the Indian Administrative Service, Director oj Census Operations, Meghalaya. CORRIGENDUM Paper 1 of 1985-MEGHALAYA Sl. Particular:; For Read No. 2 3 J. Preface, Page (iii) Siks Sjkh~ 1st Para, Line 5 ~. Introductory Note Part I the household Part I of the house Para 2, Line 6 hold. 3.' Distribution of the Population of the major religious Communities between rural and urban areas. 1710 1716 Page 2, Statement I, Col. 4 +. Page 3, Statement I Col. No. 14, Line No. I 28.69 +28.69 Col. No. 23, Line No. I 32.65 +32.65 Col. No. 23, Line No.4 L £ J. Page 8, Statement II Orissa Line 14, Col. 17 241,26 241,263 Sikkim Lim' 17, Col. l.1 7,105 7,10!i 6. Page 16, HR-15 Col. 16 (Jow~i Town, 164 164ll ,. Page 21, HR·1!) Col. 17, Rongram (U) 8930 7930 B. Page 3:), Appendix 'N, East Khasi HilLI CoL r; (R 78 75 Col.li lUi 78 Co]. 7 (lJ) 7j g, Page 5P, Appendix 'lJ' Nongpoh C.D. Block (T) Col. No. 5 3 CONTENTS Pages PREFACE iii Introductory Note 1-13 Note on Table HH-15 15 Household Population by Religion of Head of Household 16-27 Note on Appendices and Annexure to Table HH-15 29 Appendices A -Details of Religions having Population of 100 or more shown under 'Other Religions and Per,uas;on,' in Main Table HH-!.). -

The Khasi States and Shillong Municipality
THE KHASI STATES AND SHILLONG MUNICIPALITY: On the day, the Constitution of India came into force; Khasi States became a part of the State of Assam. Prior to this, there were some agreements relating to accession of the Khasi States with the Indian Union to which reference shall be made later. Before this is done, a bird's eye view at the history of these States may not be out of place. Khasis, perhaps, represent one of the earliest waves of migration to India's northeast corner. Historians are not being able to say with authority how early and from where the migration took place. Some trace it even to the days of Mahabharata; but authenticate account is lacking and it is because of this that Major P.R.Giirdon' has regarded the question relating to the origin of the Khasis as a 'very vexed' one. After referring to various opinions about the place from where the Khasis are said to have migrated, Major Gurdon was of the view that the Khasis are an offshoot of the Mon people and must have moved into Assam from east, meaning Burma, and not from west or north. The documented history of the Khasis till the advent of the British consists almost entirely of references to Khasi kings and kingdoms in the 'Buranjis' of Ahom Kings, annals of Koch King Naranarayana and some reference in the chronicles of the Kings of Tippera. The earliest named dynasty is perhaps that of Malyngiang Syiems, who were regarded as supernatural beings and Godkinds. Some historians would place these kings around 1200 A.D., while others would not agree with this. -

Part IA, Series-16, Meghalaya
For Official Use CENSUS OF INDIA 1991 SERIES 16 MEGHALAYA PART I-A ADMINISTRATION REPORT (ENUMERATION) TAPAN SENAPATI Director of Census Operations, Meghalaya CONTENTS Page PREFACE (v) Chapter Introduction 1 Chapter II Preparatory Steps 2 Chapter III Preparation for the Census 6 Chapter IV Building up of the Organisation 17 Chapter '. V Touring and Training Programmes 19 Chapter VI Census Schedules and Instruction-Translation, Printing and Distribution 21 Chapter VII Procurement of Maps 22 Chapter VIlI Preparation of Rural and Urban Frame 44 Chapter IX Enumeration Agency 28 Chapter X Houselisting Operations 30 Chapter XI Enumeration 33 Chapter XII Directives issued by the Central/State Govemments 38 Chapter XIII General 39 Chapter XIV Post-Enumeration Check 43 Chapter XV Condusion and Acknowledgement 44 APPENDICES Appendix - Otculars issued by the Registrar General, India 45 Appendix - II Circulars issued by the Director of Census Operations, Meghalaya 83 Appendix - III Important letters from the State Government of Megtlalaya 172 Appendix - IV Census Schedules - 1991 Census 186 (iii) PREfACE It has been a tradition that 'after each decennial census of the population an .. Administration Report - E.numeration" is written by each and every Director of Census Operations who has conducted the Census to record therein his functions, duties and experiences in the course of the census operations in order to act as a guide to his suc«~ssor in the next decennial census. With the passage of time and due to the continuous rise in the population. the number of districts. Dev. Blocks, drdes, etc., ha~ risen by many folds. This increase has made the conduct of the census operations more complicated and strenuous demanding huge manpower at every level. -

Chapter Six Nepali Migration and Settlement Into Northeast India In
Chapter Six Nepali Migration and Settlement into Northeast India in Colonial and Postcolonial Phase Nepali migration to Northeast India has taken place from nineteenth century mainly from Nepal and also to some extent from other parts of India. Scope of employment in the British colonial army paved the way to migration of Nepalis to India including Northeastern parts of it. For the expeditions against the tribes of Northeast Nepalis were used. Gorkhas were awarded for their service and loyalty to British army. The British tried to take care of the Gorkha soldiers, encouraged them to settle in the region and allotted land to them. After the First World War a huge number of Gorkha ex-servicemen were settled in the Northeast region, especially in Manipur. 1 British encouragement to Nepali settlement in the Northeast was not always limited to retired Gorkha soldiers but also to others. Beside military employment, Nepali migration had taken place in other sectors of service in colonial period. Nepalis worked as porters, labourers in plantation, construction and mining sectors, in oil refineries, saw mills, sugarcane cultivation, and many other sectors in Northeast India. Nepalis were also involved in large scale lumbering and clearing of forest. Plenty of land available in the hills and valleys of northeast also encouraged Nepali migrant in the profession of graziers. The British were benefited with the labour of Nepali migrants and Nepalis were easily fitted in the colonial arrangement. Cultivable rice plots were also allotted to the Nepalis. Nepalis, who migrated, settled in the foothill between Assam and Arunachal Pradesh. They also settled in the vast forest fringes and in the river banks of Assam, even in Naga Hills, Manipur, Meghalaya, Sikkim and every parts of Northeast India. -

Shillong Solid Waste Management Subproject Components
Initial Environmental Examination (Updated) February 2015 IND: North-Eastern Region Capital Cities Development Investment Program (Tranche 2) – Shillong, Meghalaya Subproject Prepared by the State Investment Program Management and Implementation Unit (SIPMIU), Urban Development Department for the Asian Development Bank. This is an updated version of the revised IEE posted in January 2013 available on http://www.adb.org/sites/default/files/ project-document/77248/35290-033-ind-iee-11.pdf CURRENCY EQUIVALENTS (as of 29 June 2011) Currency unit ± rupee (INR) INR1.00 = $0.0222 $1.00 = INR 45.040 ABBREVIATIONS ADB ² Asian Development Bank CBO ² Community Building Organization CLC ² City Level Committees CPHEEO ² Central Public Health and Environmental Engineering Organization CTE ² Consent to Establish CTO ² Consent to Operate DSMC ² Design Supervision Management Consultant EAC ² Expert Appraisal Committee EIA ² Environmental Impact Assessment EMP ² Environmental Management Plan GSPA ² Greater Shillong Planning Area GRC ² Grievance Redress Committee H&S ² Health and Safety IEE ² Initial Environmental Examination IPCC ² Investment Program Coordination Cell lpcd ² liters per capita per day MFF ² Multitranche Financing Facility MOEF ² Ministry of Environment and Forests MSW ² Municipal Solid Waste NAAQS ² National Ambient Air Quality Standards NEA ² National-Level Executing Agency NER ² North Eastern Region NERCCDIP ² North Eastern Region Capital Cities Development Investment Program NGO ² Nongovernmental Organization NSC ² National Level Steering -

Chapter – Vii Transport
CHAPTER – VII TRANSPORT 7.1 ROADS & BRIDGES 7.1.1 Road communication is the only mode of transport in the state of Meghalaya. Good road network is therefore vital for the socio-economic development of the State. The total road length of the state as on March, 2012 is 9437 Km with a road density of 42.08 Km /100 sq. Km. Out of the total road length of 9437.00 Km, 6124.00 Kms is blacktopped and 3313.00 Kms is gravelled. During 2012-13, 140.00 Km of road is anticipated to be completed. Thus the total road length at the end of the year i.e. up-to 31-03-2013 is anticipated to be 9577.00 Kms out of which 6495.00 Kms will be blacktopped and the remaining 3082.00 Km is kutcha. Thus, the road density will increase to 42.70 Km /100 sq Km. 7.1.2. The Department is having 980 nos of on-going General schemes including RIDF up-to 31-03-2012 comprising 7th, 8th, Rolling Plan, 9th, 10th & 11th Plan schemes with a total Bank of Sanction of `24933.00 (L). Maximum stress has been given to complete as many of the above schemes as practicable within the Plan Outlay. During the year 2012-13, the anticipated expenditure for implementation of these schemes is ` 9691.00 (L) and about 39 nos of schemes will be completed. Thus, the total no. of ongoing schemes at the end of 2012- 13 and the beginning of 2013-14 is expected to be around 967 with a total bank of sanction of `16959.00 (L) including 26 new schemes sanctioned during 2012-13 amounting to `1717.00(L). -

District Census Handbook, East Khasi Hills, Part XIII a & B, Series-14
CENSUS OF INDIA 1981 SERIES 1'4. MEGHALAYA PARTS XIII A & B DISTRICT CENSUS HANDBOOK VILLAGE & TOWN DIRECTORY VILLAGE & TOWNWISE PRIMARY CENSUS ABSTRACT EAST KHASI HILLS DISTRICT J. TAYENG OF THE INDIAN ADMINISTRATIVE SERVICE. Director of Cenius Operations MEGHALAYA CONTENTS Pa~. FOREWORD I-II PREFACE I-IV MAPS ... Important Statistics Census Concepts ... I-!' History of the District and the District Census Handbooks 1-7 Major Social and Cultural Events of East Khasi Hiils Distr~ct ,-j Brief Description of Places of Religious, Historical Or Archaeological Importance 1. Places of Tourist ~nterest ••. 11-12 ~p.aly.sis of Tables 13 Fly leaf to Table-l 15 Table-l Population, Number of villages and Towns, 198.1, 16 .Fly leaf to Table-2 17 Table-2 Decadal change in distribution of Population "' .. 18 ;'able-3 Dis1ribution of Villages by Popul~tjon It Table-4 Distribution of villages by density 20 Table-5 Proportion of Scheduled Castes Populatibn to total Population in the villages 21 Table-6 Proportion of ~~p.eduled Tribes Population-to total PopUlation in the villages !I .Table-7 Proportion of Scheduled Caste~j'Tribes Population in Towns J \~3 TabJe- 8 Literacy Rates ·by Population'Ranges by villages ~4 'Table-9 Literacy Rate~ for Towns !5 Fly leaf to Table-IO 26 Tabie-IO Percentage of literate workers, non-workers, scheduled castes/tribes PopUla 21-29 tion in the district. Fly leaf to Table-ll ... J Table-ll Distribution of villages according to the_,av<\ilability of different ame?,ities Table -12 Prop'Qrtion of rural Population served by different amenities Table-13 Distribution of villages not having certain amenities, arranged by distance ranges from places wJ:ere tbese are available.