The Functional Anatomy of the Cranial Nerves
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Anatomy-Nerve Tracking
INJECTABLES ANATOMY www.aestheticmed.co.uk Nerve tracking Dr Sotirios Foutsizoglou on the anatomy of the facial nerve he anatomy of the human face has received enormous attention during the last few years, as a plethora of anti- ageing procedures, both surgical and non-surgical, are being performed with increasing frequency. The success of each of those procedures is greatly dependent on Tthe sound knowledge of the underlying facial anatomy and the understanding of the age-related changes occurring in the facial skeleton, ligaments, muscles, facial fat compartments, and skin. The facial nerve is the most important motor nerve of the face as it is the sole motor supply to all the muscles of facial expression and other muscles derived from the mesenchyme in the embryonic second pharyngeal arch.1 The danger zone for facial nerve injury has been well described. Confidence when approaching the nerve and its branches comes from an understanding of its three dimensional course relative to the layered facial soft tissue and being aware of surface anatomy landmarks and measurements as will be discussed in this article. Aesthetic medicine is not static, it is ever evolving and new exciting knowledge emerges every day unmasking the relationship of the ageing process and the macroscopic and microscopic (intrinsic) age-related changes. Sound anatomical knowledge, taking into consideration the natural balance between the different facial structures and facial layers, is fundamental to understanding these changes which will subsequently help us develop more effective, natural, long-standing and most importantly, safer rejuvenating treatments and procedures. The soft tissue of the face is arranged in five layers: 1) Skin; 2) Subcutaneous fat layer; 3) Superficial musculoaponeurotic system (SMAS); 4) Areolar tissue or loose connective tissue (most clearly seen in the scalp and forehead); 5) Deep fascia formed by the periosteum of facial bones and the fascial covering of the muscles of mastication (lateral face). -

MR Imaging of Primary Trochlear Nerve Neoplasms
707 MR Imaging of Primary Trochlear Nerve Neoplasms Lindell R. Gentry 1 We present the clinical, anatomic, and MR imaging findings in six patients with seven Rahul C. Mehta 1 primary trochlear nerve neoplasms, as well as the MR and clinical criteria that serve to Richard E. Appen2 establish the diagnosis of these rare cranial nerve neoplasms. Three patients had a Joel M. Weinstein2 history of neurofibromatosis and five patients had clinical evidence of a trochlear nerve palsy. Six of seven neoplasms produced localized, fusiform enlargement of the proximal cisternal segments of the trochlear nerves. The lesions that were visible on noncontrast MR scans (T1-, T2-, and proton density-weighted) had signal intensities that were virtually identical to normal brain parenchyma. All lesions showed intense, homogeneous enhancement on contrast-enhanced scans. Contrast-enhanced imaging was necessary for the detection of five of seven lesions and greatly increased the value of the MR study in all six patients. AJNR 12:707-713, July/August 1991; AJR 157: September 1991 Primary neoplasms arising from pure motor cranial nerves such as the trochlear nerve are rare. To our knowledge just nine primary trochlear nerve neoplasms have been reported in the literature [1-7), only one of which was imaged with MR [1). Over the last 6 years, since we began to use MR as the primary imaging method for evaluating patients with cranial nerve palsies , we have noticed a striking increase in the number of primary trochlear nerve neoplasms over those encountered during the CT era. We believe this is due to a much greater sensitivity of MR in detecting these typically small lesions. -

87.MANISH KUMAR DOI.Cdr
Volume - 10 | Issue - 12 | December - 2020 | PRINT ISSN No. 2249 - 555X | DOI : 10.36106/ijar Review Article Dentistry THE MANDIBULAR NERVE, ITS COURSE, ANATOMICAL VARIATIONS AND PTERYGOMANDIBULAR SPACE. - A SYSTEMATIC REVIEW. Assistant Professor, Department Of Dentistry, Government Medical College & Dr. Manish Kumar Hospital, Ratlam (M.P). Dr. Kapil Associate Professor, Department Of Dentistry, Ananta Institute Of Medical Sciences Karwasra* And Research Centre, Rajsamand, Rajasthan. *Corresponding Author Dr. Amit Senior Resident, Department Of Dentistry, Sardar Patel Medical College & Associated Chhaparwal Hospital, Bikaner, (Rajasthan). ABSTRACT Knowledge of mandibular nerve and its branches is important when performing dental and surgical procedures of mandible. So, this systematic review article revealed all details of mandibular nerve course and also important anatomical variations. Mandibular nerve during its course go through the pterygomandibular space and this space is important for inferior alveolar nerve block anaesthesia, so all details of pterygomandibular structure are also included in this review. KEYWORDS : Mandibular Nerve, Pterygomandibular Space, Inferior Alveolar Nerve, Trigeminal Nerve, Trigeminal Ganglion. INTRODUCTION and this site is generally used for buccal nerve block 5. The trigeminal nerve (TN) exits the brain on the lateral surface of pons, entering the trigeminal ganglion (TGG) after few millimeters, Deep temporal nerves usually are two nerves, anterior and posterior. followed by an extensive series of divisions1. Mandibular nerve (MN) They pass between the skull and the LPt, and enter the deep surface of is the largest of the three divisions of trigeminal nerve. MN also temporalis2. contains motor or efferent bers to innervate the muscles that are attached to mandible. Most of these bers travel directly to their target The nerve to LPt enters the deep surface of the muscle and may arise tissues. -
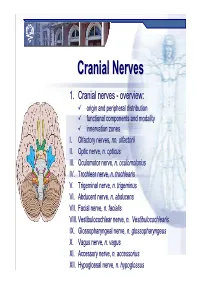
Cranial Nervesnerves
CranialCranial NervesNerves 1. Cranial nerves - overview: origin and peripheral distribution functional components and modality innervation zones I. Olfactory nerves, nn. olfactorii II. Optic nerve, n. opticus III. Oculomotor nerve, n. oculomotorius IV. Trochlear nerve, n. trochlearis V. Trigeminal nerve, n. trigeminus VI. Abducent nerve, n. abducens VII. Facial nerve, n. facialis VIII. Vestibulocochlear nerve, n. Vestibulocochlearis IX. Glossopharyngeal nerve, n. glossopharyngeus X. Vagus nerve, n. vagus XI. Accessory nerve, n. accessorius XII. Hypoglossal nerve, n. hypoglossus Cranial nerves CranialCranial nervesnerves 0. N. terminalis I. N. olfactorius II. N. opticus III. N. oculomotorius IV. N. trochlearis V. N. trigeminus VI. N. abducens VII. N. facialis VIII. N. vestibulocochlearis IX. N. glossopharyngeus X. N. vagus XI. N. accessorius XII. N. hypoglossus Prof. Dr. Nikolai Lazarov 2 Cranial nerves FunctionalFunctional classificationclassification purely sensory (afferent ): n. olfactorius n. opticus n. vestibulocochlearis purely motor (efferent): n. oculomotorius n. trochlearis n. abducens n. accessorius n. hypoglossus mixed (sensory&motor ): n. trigeminus n. facialis n. glossopharyngeus n. vagus autonomic (parasympathetic( ): n. oculomotorius n. facialis n. glossopharyngeus n. vagus Prof. Dr. Nikolai Lazarov 3 Cranial nerves AnatomicAnatomic relationshipsrelationships Location within the brainstem: ventrally: n. olfactorius n. opticus n. oculomotorius n. abducens n. hypoglossus laterally: n. trigeminus -

Use of Calcium-Binding Proteins to Map Inputs in Vestibular Nuclei of the Gerbil
THE JOURNAL OF COMPARATIVE NEUROLOGY 386:317–327 (1997) Use of Calcium-Binding Proteins to Map Inputs in Vestibular Nuclei of the Gerbil GOLDA ANNE KEVETTER* AND ROBERT B. LEONARD Departments of Otolaryngology, Anatomy and Neurosciences, and Physiology and Biophysics, University of Texas Medical Branch, Galveston, Texas 77555 ABSTRACT We wished to determine whether calbindin and/or calretinin are appropriate markers for vestibular afferents, a population of neurons in the vestibular nuclear complex, or cerebellar Purkinje inputs. To accomplish this goal, immunocytochemical staining was observed in gerbils after lesions of the vestibular nerve central to the ganglion, the cerebellum, or both. Eleven to fourteen days after recovery, the brain was processed for immunocytochemical identification of calretinin and calbindin. After lesion of the vestibular nerve, no calretinin staining was seen in any of the vestibular nuclei except for a population of intrinsic neurons, which showed no obvious change in number or staining pattern. Calbindin staining was reduced in all nuclei except the dorsal part of the lateral vestibular nuclei. The density of staining of each marker, measured in the magnocellular medial vestibular nucleus, was signifi- cantly reduced. After the cerebellar lesion, no differences in calretinin staining were noted. However, calbindin staining was greatly reduced in all nuclei. The density of staining, measured in the caudal medial vestibular nucleus, was significantly lower. After a combined lesion of the cerebellum and vestibular nerve, the distribution and density of calretinin staining resembled that after vestibular nerve section alone, whereas calbindin staining was no longer seen. This study demonstrates that calretinin and calbindin are effective markers for the identification of vestibular afferents. -

Cranial Nerves 1, 5, 7-12
Cranial Nerve I Olfactory Nerve Nerve fiber modality: Special sensory afferent Cranial Nerves 1, 5, 7-12 Function: Olfaction Remarkable features: – Peripheral processes act as sensory receptors (the other special sensory nerves have separate Warren L Felton III, MD receptors) Professor and Associate Chair of Clinical – Primary afferent neurons undergo continuous Activities, Department of Neurology replacement throughout life Associate Professor of Ophthalmology – Primary afferent neurons synapse with secondary neurons in the olfactory bulb without synapsing Chair, Division of Neuro-Ophthalmology first in the thalamus (as do all other sensory VCU School of Medicine neurons) – Pathways to cortical areas are entirely ipsilateral 1 2 Crania Nerve I Cranial Nerve I Clinical Testing Pathology Anosmia, hyposmia: loss of or impaired Frequently overlooked in neurologic olfaction examination – 1% of population, 50% of population >60 years Aromatic stimulus placed under each – Note: patients with bilateral anosmia often report nostril with the other nostril occluded, eg impaired taste (ageusia, hypogeusia), though coffee, cloves, or soap taste is normal when tested Note that noxious stimuli such as Dysosmia: disordered olfaction ammonia are not used due to concomitant – Parosmia: distorted olfaction stimulation of CN V – Olfactory hallucination: presence of perceived odor in the absence of odor Quantitative clinical tests are available: • Aura preceding complex partial seizures of eg, University of Pennsylvania Smell temporal lobe origin -

Trigeminal Cave and Ganglion: an Anatomical Review
Int. J. Morphol., 31(4):1444-1448, 2013. Trigeminal Cave and Ganglion: An Anatomical Review Cavo y Ganglio Trigeminal: Una Revisión Anatómica N. O. Ajayi*; L. Lazarus* & K. S. Satyapal* AJAYI, N. O.; LAZARUS, L. & SATYAPAL, K. S. Trigeminal cave and ganglion: an anatomical review. Int. J. Morphol., 31(4):1444- 1448, 2013. SUMMARY: The trigeminal cave (TC) is a special channel of dura mater, which extends from the posterior cranial fossa into the posteromedial portion of the middle cranial fossa at the skull base. The TC contains the motor and sensory roots of the trigeminal nerve, the trigeminal ganglion (TG) as well as the trigeminal cistern. This study aimed to review the anatomy of the TC and TG and determine some parameters of the TC. The study comprised two subsets: A) Cadaveric dissection on 30 sagitally sectioned formalin fixed heads and B) Volume injection. We found the dura associated with TC arranged in three distinct layers. TC had relations with internal carotid artery, the cavernous sinus, the superior petrosal sinus, the apex of petrous temporal bone and the endosteal dura of middle cranial fossa. The mean volume of TC was 0.14 ml. The mean length and breadth of TG were 18.3 mm and 7.9 mm, respectively, mean width and height of trigeminal porus were 7.9 mm and 4.1 mm, respectively, and mean length of terminal branches from TG to point of exit within skull was variable. An understanding of the precise formation of the TC, TG, TN and their relations is important in order to perform successful surgical procedures and localized neural block in the region of the TC. -

Surgical Treatment of Bronchial Asthma by Resection of the Laryngeal Nerve
Surgical treatment of bronchial asthma by resection of the laryngeal nerve Ubaidullo Kurbon, Hamza Dodariyon, Abdumalik Davlatov, Sitora Janobilova, Amu Therwath, Massoud Mirshahi To cite this version: Ubaidullo Kurbon, Hamza Dodariyon, Abdumalik Davlatov, Sitora Janobilova, Amu Therwath, et al.. Surgical treatment of bronchial asthma by resection of the laryngeal nerve. BMC Surgery, BioMed Central, 2015, 15 (1), pp.109. 10.1186/s12893-015-0093-2. inserm-01264486 HAL Id: inserm-01264486 https://www.hal.inserm.fr/inserm-01264486 Submitted on 29 Jan 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Kurbon et al. BMC Surgery (2015) 15:109 DOI 10.1186/s12893-015-0093-2 TECHNICAL ADVANCE Open Access Surgical treatment of bronchial asthma by resection of the laryngeal nerve Ubaidullo Kurbon1, Hamza Dodariyon1, Abdumalik Davlatov1, Sitora Janobilova1, Amu Therwath2 and Massoud Mirshahi1,2* Abstract Background: Management of asthma in chronically affected patients is a serious health problem. Our aim was to show that surgical treatment of chronic bronchial asthma by unilateral resection of the internal branch of the superior laryngeal nerve (ib-SLN) is an adequateand lasting remedial response. Patients and methods: In a retrospective study, 41 (26 male and 15 female) patients with bronchial chronic asthma were treated surgically during the period between 2005 and 2013. -

Cranial Nerve VIII
Cranial Nerve VIII Color Code Important (The Vestibulo-Cochlear Nerve) Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the students should be able to: ✓ List the nuclei related to vestibular and cochlear nerves in the brain stem. ✓ Describe the type and site of each nucleus. ✓ Describe the vestibular pathways and its main connections. ✓ Describe the auditory pathway and its main connections. Due to the difference of arrangement of the lecture between the girls and boys slides we will stick to the girls slides then summarize the pathway according to the boys slides. Ponto-medullary Sulcus (cerebello- pontine angle) Recall: both cranial nerves 8 and 7 emerge from the ventral surface of the brainstem at the ponto- medullary sulcus (cerebello-pontine angle) Brain – Ventral Surface Vestibulo-Cochlear (VIII) 8th Cranial Nerve o Type: Special sensory (SSA) o Conveys impulses from inner ear to nervous system. o Components: • Vestibular part: conveys impulses associated with body posture ,balance and coordination of head & eye movements. • Cochlear part: conveys impulses associated with hearing. o Vestibular & cochlear parts leave the ventral surface* of brain stem through the pontomedullary sulcus ‘at cerebellopontine angle*’ (lateral to facial nerve), run laterally in posterior cranial fossa and enter the internal acoustic meatus along with 7th (facial) nerve. *see the previous slide Auditory Pathway Only on the girls’ slides 04:14 Characteristics: o It is a multisynaptic pathway o There are several locations between medulla and the thalamus where axons may synapse and not all the fibers behave in the same manner. -

Volume 1: the Upper Extremity
Volume 1: The Upper Extremity 1.1 The Shoulder 01.00 - 38.20 (37.20) 1.1.1 Introduction to shoulder section 0.01.00 0.01.28 0.28 1.1.2 Bones, joints, and ligaments 1 Clavicle, scapula 0.01.29 0.05.40 4.11 1.1.3 Bones, joints, and ligaments 2 Movements of scapula 0.05.41 0.06.37 0.56 1.1.4 Bones, joints, and ligaments 3 Proximal humerus 0.06.38 0.08.19 1.41 Shoulder joint (glenohumeral joint) Movements of shoulder joint 1.1.5 Review of bones, joints, and ligaments 0.08.20 0.09.41 1.21 1.1.6 Introduction to muscles 0.09.42 0.10.03 0.21 1.1.7 Muscles 1 Long tendons of biceps, triceps 0.10.04 0.13.52 3.48 Rotator cuff muscles Subscapularis Supraspinatus Infraspinatus Teres minor Teres major Coracobrachialis 1.1.8 Muscles 2 Serratus anterior 0.13.53 0.17.49 3.56 Levator scapulae Rhomboid minor and major Trapezius Pectoralis minor Subclavius, omohyoid 1.1.9 Muscles 3 Pectoralis major 0.17.50 0.20.35 2.45 Latissimus dorsi Deltoid 1.1.10 Review of muscles 0.20.36 0.21.51 1.15 1.1.11 Vessels and nerves: key structures First rib 0.22.09 0.24.38 2.29 Cervical vertebrae Scalene muscles 1.1.12 Blood vessels 1 Veins of the shoulder region 0.24.39 0.27.47 3.08 1.1.13 Blood vessels 2 Arteries of the shoulder region 0.27.48 0.30.22 2.34 1.1.14 Nerves The brachial plexus and its branches 0.30.23 0.35.55 5.32 1.1.15 Review of vessels and nerves 0.35.56 0.38.20 2.24 1.2. -

Imaging Features Differentiating Vestibular Ganglion From
Click HERE for more articles at Annals, Academy of Medicine, Singapore homepage Differentiating Ganglion from Schwannoma—Yi-Wei Wu et al 65 Original Article Imaging Features Differentiating Vestibular Ganglion from Intracanalicular Schwannoma on Single-Sequence Non-Contrast Magnetic Resonance Imaging Study 1 1 1 2 Yi-Wei Wu, MD, MMed, FRCR, Amit Karandikar, MBBS, FRCR, FAMS, Julian PN Goh, MBBS, FRCR, Tiong Yong Tan, MBBS, FRCR, FAMS Abstract Introduction: This study aimed to identify imaging features on single-sequence non- contrast magnetic resonance imaging (MRI) that differentiate the vestibular ganglion from small intracanalicular schwannomas. Materials and Methods: Ninety patients (42 men and 48 women; age: 24‒87 years old) with 102 internal auditory canal (IAC) nodules (59 vestibular ganglia and 43 intracanalicular schwannoma) who underwent both single- sequence T2-weighted (T2W) non-contrast enhanced MRI studies and contrast-enhanced T1-weighted (T1W) MRI studies between May 2012 and April 2017 were evaluated. The length, width, distance to the IAC fundus and length/width ratios for all lesions were obtained and compared among groups. Diagnostic performance and cutoff values of the parameters were evaluated with receiver operating characteristics curve analysis. Area under the curve (AUC) value was calculated. Results: Vestibular ganglia have significantly smaller lengths and widths compared to intracanalicular vestibular schwannomas (1.7 ± 0.4 mm and 1.0 ± 0.2 mm versus 5.6 ± 3.0 mm and 3.7 ± 1.5 mm). They are more fusiform in shape compared to vestibular schwannomas (length/width ratio: 1.8 ± 0.4 versus 1.5 ± 0.4). The lesion width demonstrated the highest diagnostic performance (AUC: 0.998).