Improving Health and Wellbeing in Bedfordshire, Luton and Milton Keynes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of Bedfordshire Application Form
International StudentApplication Form Please return the completed form to:International Admissions University of Bedfordshire University Square, Luton, Bedfordshire LU1 3JU United Kingdom T: +44 (0)1582 489326 F: +44 (0)1582 743469 5JFSSponsor Licence Number DA8AR2CH7 [email protected] Please read the notes at the back before completing this form. It is important that you write neatly using BLOCK CAPITALS in black ink or typescript. If available, you must include a copy of the personal details page from your passport (the page that contains the passport number and your photo). Incomplete application forms submitted without ALL the supporting documents may delay the issuing of your offer. 1 Personal Details Title (Mr/Mrs/Miss/Ms etc) Male Female Date of birth* (dd/mm/yyyy) First name(s) Family name(s) Previous family name (if changed) Passport number and country of issue Correspondence address Permanent/Home address (if different) Postcode Postcode Telephone (including international code) Telephone (including international code) Mobile (including international code) Mobile (including international code) Current email Skype ID Do you have any criminal convictions? Yes No Have you received any other penalty in relation to a criminal offence; for example a caution, reprimand, warning, or similar penalties in the UK or any other country? Yes No 2 Fee Status and iration History Country of birth Present nationality Country of Domicile Are you currently a resident in the UK? Yes No Have you ever been refused a Visa to any country? Yes No Have you studied in the UK previously? If es o Have you been denied entry to the UK before? Yes o yes, provide details below. -

County Unitary/District Project Name Project Applicant
Item 1 - Declarations of Interest County Unitary/District Project Name Project Applicant LOCAL GROWTH FUND £265m Buckinghamshire County Council The Exchange, Aylesbury (formerly known as Waterside North) AVDC Buckinghamshire County Council Digital Manufacturing Centre KWSP Bedford Borough Council Bedford Western Bypass Bedford Borough Council Bedford Borough Council Advanced Engineering Centre, Bedford College Bedford College Bedford Borough Council I-WORX Bedford Borough Council Bedford Borough Council Transporting Bedford 2020 Bedford Borough Council Bedford Borough Council Mark Rutherford School Trust STEM Training Centre Mark Rutherford School Trust Bedford Borough Council Hydroponics Growpura Ltd Central Bedfordshire Council Cranfield University Forensic Sciences Institute Cranfield University Central Bedfordshire Council /Milton Keynes Council MK: U - educational acceleration in digital skills Cranfield University Central Bedfordshire Council Dunstable High Street Central Bedfordshire Council Central Bedfordshire Council Smarter Routes to Employment Central Bedfordshire Council Central Bedfordshire Council Engineering and Construction Skills Leighton Buzzard Central Bedfordshire Council Central Bedfordshire Council Woodside Link Central Bedfordshire Council Central Bedfordshire Council A421 dualling Central Bedfordshire Council Central Bedfordshire Council MUEAVI Cranfield University Central Bedfordshire Council Millbrook Innovation Centre Millbrook Proving Ground Ltd Central Bedfordshire Council Millbrook Tyre Testing and Handling -

Successful Bids to the Police Innovation Fund 2016 to 2017
SUCCESSFUL BIDS TO THE POLICE INNOVATION FUND 2016/17 Bid 2016/17 Lead Force Other partners Bid Name / Details No. Award National Centre for Cyberstalking Research (NCCR) – University of Bedfordshire Cyberharassment: University of Liverpool Bedfordshire Platform for Evidence Nottingham Trent University £461,684.00 47 Gathering, Assessing Police Victim Support Risk & Managing Hampshire Stalking Policing Consultancy Clinic Paladin Greater Manchester Police Dyfed-Powys PCC Cambridgeshire Constabulary University of Cambridge BeNCH Community Rehabilitation Company Crown Prosecution Service Evidence-based Local authorities Cambridgeshire approach to deferred Health system £250,000.00 36 prosecution linked to Constabulary Criminal Justice Board devolution in West Midlands Police Cambridgeshire. Hampshire Constabulary Hertfordshire Constabulary Leicestershire Police Staffordshire Police West Yorkshire Police Ministry of Justice/NOMS Warwickshire Police Cheshire Integrated Force West Mercia Police £303,000.00 122 Communications Constabulary West Mercia Fire and Rescue Solution Cheshire Fire and Rescue Fire and Rescue Services Cheshire (FRS) through the Chief Fire National Air Service for 140 £120,100.00 Constabulary Officers’ Association (CFOA) emergency services Association of Ambulance (Category 1 and 2) Chief Executives (AACE) City of London Metropolitan Police Service False identity data £525,000.00 62 Warwickshire Police Police capture and sharing Barclays Bank Metropolitan Police Service Serious Fraud Office Public/private Crown Prosecution -

Plaque Schemes Across England
PLAQUE SCHEMES ACROSS ENGLAND Plaque schemes are listed below according to region and county, apart from thematic schemes which have a national remit. The list includes: the name of the erecting body (with a hyperlink to a website where possible); a note of whether the scheme is active, dormant, proposed or complete; and a link to an email contact where available. While not all organisations give details of their plaques on their websites, the information included on the register should enable you to contact those responsible for a particular scheme. In a few cases, plaques are described as ‘orphaned’, which indicates that they are no longer actively managed or maintained by the organisation that erected them. English Heritage is not responsible for the content of external internet sites. BEDFORDSHIRE Bedford Borough ACTIVE Council Various historical schemes BEDFORDSHIRE Biggleswade COMPLETED Contact EAST History Society 1997-2004 BEDFORDSHIRE Dunstable COMPLETED Contact Town Council CAMBRIDGESHIRE Cambridge Blue ACTIVE Contact Plaques Scheme since 2001 CAMBRIDGESHIRE Eatons ACTIVE Contact Community Association 1 PLAQUE SCHEMES ACROSS ENGLAND CAMBRIDGESHIRE Great Shelford ACTIVE Contact Oral History Group CAMBRIDGESHIRE Littleport Society AD HOC One-off plaque erected in 2011, more hoped for. CAMBRIDGESHIRE Peterborough ACTIVE Contact Civic Society since the 1960s CAMBRIDGESHIRE St Ives ACTIVE Contact EAST Civic Society since 2008 CAMBRIDGESHIRE St Neots Local ACTIVE Contact History Society ESSEX (Basildon) PROPOSED Contact Foundation -

Christopher Hollyman, Sr. of Isle of Wight, Virginia and His Children
Christopher Hollyman, Sr. of Isle of Wight, Virginia and His Children Anne Christopher Hollyman Mary Birth: ? Birth: 1618 Birth: abt 1637 Death: Isle of Wight, Virginia Bedford, Bedfordshire, England Isle of Wight, Virginia Death: Aft 10 Aug 1691 Death: abt 1704 Isle of Wight, Virginia Isle of Wight, Virginia John Hollyman * Mary Hollyman James Atkinson Birth: abt 1657 Birth: abt 1670 Birth: 1660 Isle of Wight, Virginia Isle of Wight, Virginia Isle of Wight, Virginia * Indirect evidence Death: Abt 1723 Death: 23 Dec 1723 of his existence Isle of Wight, Virginia Isle of Wight, Virginia Susannah Vasser Christopher Hollyman Birth: 1659 Birth: 1658-1660 In 1650, Christopher Hollyman, Sr., Isle of Wight, Virginia Isle of Wight, Virginia immigrated from England to Jamestown, Death: aft Jun 1755 Death: 1729-1731 Isle of Wight, Virginia Isle of Wight, Virginia Virginia.HefirstmarriedAnneinabout 1655, and after her death, he married his second wife, Mary, around 1668. Elizabeth Thomas Hollyman Christopher had 5 known sons and 2 daughters. There is some evidence Birth: ? Birth: 1660-1662 Death: 1736-1737 Isle of Wight, Virginia pointing to a 6th son, John Hollyman, Isle of Wight, Virginia Death: 1732-1734 but no solid proof has been found, yet. Isle of Wight, Virginia His sons carried the family name forward, sometimes spelling it Holliman, Marie “Mary” Chambers William Hollyman Holleman, Holloman, Holyman, and other variations depending on the literacy level of Birth: 1659 Birth: 1662-1664 the county court clerk at the time. Isle of Wight, -
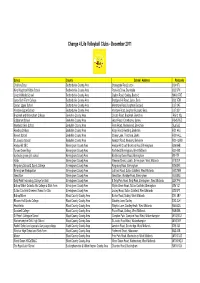
Website List Dec 11
Change 4 Life Volleyball Clubs - December 2011 School County School Address Postcode Challney Boys Bedfordshire County Area Stoneygate Road, Luton LU4 9TJ King Houghton Middle School Bedfordshire County Area Parkside Drive, Dunstable LU5 5PX Lincroft Middle School Bedfordshire County Area Station Road, Oakley, Bedford MK43 7RE Luton Sixth Form College Bedfordshire County Area Bradgers Hill Road, Luton, Beds LU2 7EW Cedars Upper School Bedfordshire County Area Mentmore Road, Leighton Buzzard LU7 2AE Vandyke Upper School Bedfordshire County Area Vandyke Road, Leighton Buzzard, Beds LU7 3DY Bracknell and Wokingham College Berkshire County Area Chruch Road, Bracknell, Berkshire RG12 1DJ Edgbarrow School Berkshire County Area Grant Road, Crowthorne, Surrey RG45 7HZ Newlands Girls School Berkshire County Area Farm Road, Maidenhead, Berkshire SL6 5JB Reading College Berkshire County Area Kings Road, Reading, Berkshire RG1 4HJ Kennet School Berkshire County Area Stoney Lane, Thatcham, Berks RG19 4LL St Josephs School Berkshire County Area Newport Road, Newbury, Berkshire RG14 2AW Hodge Hill SEC Birmingham County Area Hodge Hill Court, Bromford Road, Birmingham B36 8HB Turves Green Boys Birmingham County Area Northfield, Birmingham, West Midlands B31 4BS bordesley green girls school Birmingham County Area Bordesley Green Road, Birmingham B9 4TR Holte Birmingham County Area Wheeler Street, Lozells, Birmingham, West Midlands B19 2EP Kingsbury School & Sports College Birmingham County Area Kingsbury Road, Birmingham B24 8RE Birmingham Metropolitan -

Bedfordshire People Past and Present
Bedfordshire People Past and Present 1 Bedfordshire People Past and Present This is just a selection of some of the notable people associated with Bedfordshire. Bedfordshire Borough and Central Bedfordshire libraries offer a wealth of resources, for more detailed information see the Virtual Library: www.bedford.gov.uk or www.centralbedfordshire.gov.uk Click on Libraries Click on Local and Family History Click on People The Local Studies section at Bedford Central Library also holds an archive of newspaper cuttings, biography files, an obituary index, local periodicals and books, including A Bedfordshire Bibliography by L.R. Conisbee, which has a large biography section. 2 Bedfordshire People Past Offa (? -796 BC) King Offa, regarded as one of the most powerful kings in early Anglo-Saxon England, ruled for 39 years from 757 to his death in 796. It is traditionally believed that he was buried in Bedford, somewhere near Batts Ford. Falkes De Breaute (1180-1225) A French soldier and adventurer, Falkes's loyalty to King John was rewarded with a number of titles. The king also gave him Bedford Castle, which Falkes held until 1224 when it was besieged and demolished by King Henry III. Falkes escaped and fled to the continent but died on route from food poisoning. Queen Eleanor (1244-1290) The sad death of Queen Eleanor links her to Dunstable. She died in Lincolnshire and King Edward 1st – her husband – wanted her to be buried in Westminster, thus the body was taken back to London and passed through Dunstable. The king ordered memorial crosses to be erected at every place the funeral cortege stopped overnight. -

1 New Methodologies for the Estimation of Urbanisation in England C.1670 and C.17611,2 Romola Davenport3, Max Satchell, Oliver D
New methodologies for the estimation of urbanisation in England c.1670 and c.17611,2 Romola Davenport3, Max Satchell, Oliver Dunn, Gill Newton and Leigh Shaw-Taylor4 The United Nations estimates that the proportion of the world’s population living in urban areas exceeded the population in rural areas by 2008 (United Nations, 2007). In Britain conventional estimates of the urban population of England and Wales and of Scotland indicate that this benchmark was reached by the mid-nineteenth century, the first national populations to achieve this level. This precocious urbanisation was in marked contrast to most of continental Europe, where urbanisation levels stagnated across the eighteenth and early nineteenth centuries (Bairoch & Goertz, 1986; de Vries, 1984; Wrigley, 2014). It is also especially remarkable because the British Isles, like the other fringes of Europe, lagged behind the continental average before the late seventeenth century. De Vries estimated that only 5.8 % of the population of England and Wales lived in towns of 10,000 or more in 1600, compared with 7.6 % for western Europe as a whole. By 1700 the comparable figures were 13.2 % and 9.2 %, and by 1800 a fifth of the population of England and Wales lived in such towns, compared with a tenth of the European population (de Vries, p. 39,64). The British experience of urbanisation is often used as the standard exemplar or comparator for modern patterns of urbanisation elsewhere. We have a relatively clear picture of developments in nineteenth century Britain as a consequence of the instigation of decennial censuses from 1801. -
Luton and South Bedfordshire Local Development Framework
Luton and South Bedfordshire Local Development Framework Sustainability Appraisal Draft Scoping Report May 2007 Luton and South Bedfordshire Local Development Framework Sustainability Appraisal Scoping Report Contents Amendment Record This report has been issued and amended as follows: Issue Revision Description Date Signed 01 00 Draft SA Scoping Report 24/1/07 JPW 02 01 Draft SA Scoping Report 6/02/07 JPW 03 02 Final SA Scoping Report 14/3/07 JPW 04 03 Final SA Scoping Report 25/4/0 JPW Contents 1 INTRODUCTION 1 1.1 Background 1 1.2 Luton and South Bedfordshire Local Development Framework 2 1.3 Background to SEA and SA 3 1.4 Health Impacts 5 1.5 Health and Sustainable Development 5 1.6 Equality Impacts 5 1.7 Purpose of this Scoping Report 6 1.8 Structure of this Report 7 2 Stage A1- Identifying other relevant plans, programmes and sustainability objectives 9 2.1 Background 9 2.2 Purpose 9 2.3 Economic Factors 13 2.4 Social Factors 14 2.5 Water 15 2.6 Biodiversity 15 2.7 Air Quality 16 2.8 Soil 16 2.9 Climatic Factors 16 2.10 Population 17 2.11 Human Health 17 2.12 Material Assets 19 2.13 Cultural Heritage 19 2.14 Landscape and Townscape 19 3 Stage A2- Collecting Baseline Information 21 3.1 Background 21 3.2 Collection Methodology 22 3.3 Baseline Analysis 22 3.4 Economic Factors 22 3.5 Social Factors 26 3.6 Water 31 3.7 Biodiversity 33 3.8 Air Quality 39 3.9 Soil 43 3.10 Climatic Factors 44 3.11 Population 45 3.12 Human Health 48 3.13 Material Assets 53 3.14 Cultural Heritage 55 3.15 Landscape 55 3.16 Townscape 57 4 Stage A3- Identifying -
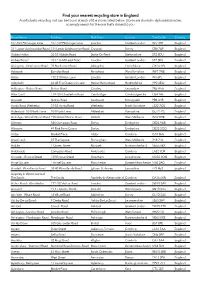
Find Your Nearest Recycling Store in England a Soft Plastic Recycling Unit Can Be Found at Each of the Stores Listed Below
Find your nearest recycling store in England A soft plastic recycling unit can be found at each of the stores listed below. Stores are shared in alphabetical order, so simply search for the one that’s closest to you. Store Name Address Post Town County Post Code Country 107-109 Pitshanger Lane 107-109 Pitshanger Lane London Greater London W5 1RH England 311 Lower Addiscombe Road 311 Lower Addiscombe Road Croydon Surrey CR0 7AF England Abbey Hulton 53-55 Abbots Road Stoke-On-Trent Staffordshire ST2 8DU England Abbey Wood 103-116 McLeod Road London Greater London SE2 0BS England Abingdon - Northcourt Road 39 Northcourt Road Abingdon Oxfordshire OX14 1PJ England Ackworth Barnsley Road Pontefract West Yorkshire WF7 7NB England Acton 192-210 Horn Lane London Greater London W3 6PL England Adeyfield 46-48 The Queens Square Hemel Hempstead Hertfordshire HP2 4EW England Adlington - Bolton Road Bolton Road Chorley Lancashire PR6 9NA England Ailsa Court 179-185 Chesterton Road Cambridge Cambridgeshire CB4 1AF England Ainsdale Station Road Southport Merseyside PR8 3HR England Ainsty Road Wetherby 51-55 Ainsty Road Wetherby North Yorkshire LS22 7QS England Aldershot - 264 North Lane 264 North Lane Aldershot Hampshire GU12 4TJ England Aldridge - Walsall Wood Road 198 Walsall Wood Road Walsall West Midlands WS9 8HB England Allenton 840 Osmaston Road Derby Derbyshire DE24 9AB England Allestree 49 Park Farm Centre Derby Derbyshire DE22 2QQ England Alston Market Place Alston Cumbria CA9 3HS England Alvechurch 25 The Square Birmingham West Midlands B48 7LA England Amble 1 Queen Street Morpeth Northumberland NE65 0BX England Ambleside Compston Road Ambleside Cumbria LA22 9DR England Ancaster - Ermine Street 139 Ermine Street Grantham Lincolnshire NG32 3QN England Angel Square 1 Angel Square Manchester Greater Manchester M60 0AG England Ansdell - Woodlands Road 38-40 Woodlands Road Lytham St. -

Bedfordshire Historical Record Society
1 Bedfordshire Historical Record Society Bedfordshire and the Lincolnshire Parish Clergy A lecture presented to Bedfordshire Historical Record Society on 23 September 2016 by Dr Nicholas Bennett Kirkby with Muckby-cum-Sparrowby-cum-Spinx Is down a long lane in the county of Lincs, And often on Wednesdays, well-harnessed and spruce, I would drive into Wiss over Winderby Sluice. A whacking great sunset bathed level and drain From Kirkby with Muckby to Beckby-on-Bain, And I saw, as I journeyed, my marketing done, Old Caistorby tower take the last of the sun. The opening lines of A Lincolnshire Tale, John Betjeman’s well-loved poem, capture that familiar landscape, thickly populated with parish churches, their towers and spires rising from the villages and towns of the county. In 1914, on the eve of the First World War, there were some 700 Anglican parish churches and parochial chapels in the diocese. During the past hundred years, some of these have been declared ‘redundant’, or even destroyed, but the great majority remain as witnesses to the central role of the Christian faith in the history of Lincolnshire communities. The fabric of these buildings, nave and chancel, font, pulpit and reading desk, stained glass and monuments, all tell of the long history of their parishes. But what of the clergy who served them? Go inside one of these churches, savour the familiar smell of hassocks and hymn books, and you will often see beside the door a framed list of past incumbents. They serve to remind us that in order to understand the history of the towns and villages in which these churches stand, we must go beyond the buildings themselves and explore the lives of those who used them. -

CTSA Contacts UK List
CTSA Contacts UK List Region Email Address Avon and Somerset [email protected] Bedfordshire Beds&HertsCT&[email protected] British Transport Police [email protected] Cambridgeshire [email protected] Central Scotland [email protected] Cheshire [email protected] City Of London [email protected] Cleveland [email protected] Cumbria [email protected] Derbyshire [email protected] Devon and Cornwall [email protected] Dorset [email protected] Dumfries and Galloway [email protected] Durham [email protected] Dyfed Powys [email protected] Essex [email protected] Fife [email protected] Gloucestershire [email protected] Grampian [email protected] Greater Manchester [email protected] Hampshire [email protected] Heddlu Gwent [email protected] Humberside [email protected] Kent [email protected] Lancashire [email protected] Leicestershire [email protected] Lincolnshire [email protected] Lothian and Borders [email protected] Merseyside [email protected] Metropolitan [email protected] Ministry of Defence [email protected] NaCTSO [email protected] Norfolk [email protected] North Wales [email protected] North Yorkshire [email protected] Northamptonshire [email protected]