On Human Anatomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Larynx Anatomy
LARYNX ANATOMY Elena Rizzo Riera R1 ORL HUSE INTRODUCTION v Odd and median organ v Infrahyoid region v Phonation, swallowing and breathing v Triangular pyramid v Postero- superior base àpharynx and hyoid bone v Bottom point àupper orifice of the trachea INTRODUCTION C4-C6 Tongue – trachea In women it is somewhat higher than in men. Male Female Length 44mm 36mm Transverse diameter 43mm 41mm Anteroposterior diameter 36mm 26mm SKELETAL STRUCTURE Framework: 11 cartilages linked by joints and fibroelastic structures 3 odd-and median cartilages: the thyroid, cricoid and epiglottis cartilages. 4 pair cartilages: corniculate cartilages of Santorini, the cuneiform cartilages of Wrisberg, the posterior sesamoid cartilages and arytenoid cartilages. Intrinsic and extrinsic muscles THYROID CARTILAGE Shield shaped cartilage Right and left vertical laminaà laryngeal prominence (Adam’s apple) M:90º F: 120º Children: intrathyroid cartilage THYROID CARTILAGE Outer surface à oblique line Inner surface Superior border à superior thyroid notch Inferior border à inferior thyroid notch Superior horns à lateral thyrohyoid ligaments Inferior horns à cricothyroid articulation THYROID CARTILAGE The oblique line gives attachement to the following muscles: ¡ Thyrohyoid muscle ¡ Sternothyroid muscle ¡ Inferior constrictor muscle Ligaments attached to the thyroid cartilage ¡ Thyroepiglottic lig ¡ Vestibular lig ¡ Vocal lig CRICOID CARTILAGE Complete signet ring Anterior arch and posterior lamina Ridge and depressions Cricothyroid articulation -

Diseases of Salivary Glands: Review
ISSN: 1812–1217 Diseases of Salivary Glands: Review Alhan D Al-Moula Department of Dental Basic Science BDS, MSc (Assist Lect) College of Dentistry, University of Mosul اخلﻻضة امخجوًف امفموي تُئة رطبة، حتخوي ػىل طبلة ركِلة من امسائل ثدغى انوؼاب ثغطي امسطوح ادلاخوَة و متﻷ امفراغات تني ااطَة امفموًة و اﻷس نان. انوؼاب سائل مؼلد، ًنذج من امغدد انوؼاتَة، اذلي ًوؼة دورا" ىاما" يف اﶈافظة ػىل سﻻمة امفم. املرىض اذلٍن ؼًاهون من هلص يف اﻷفراز انوؼايب حكون دلهيم مشبلك يف اﻷلك، امخحدث، و امبوع و ًطبحون غرضة مﻷههتاابت يف اﻷغش َة ااطَة و امنخر املندرش يف اﻷس نان. ًوخد ثﻻثة أزواج من امغدد انوؼاتَة ام ئرُسة – امغدة امنكفِة، امغدة حتت امفكِة، و حتت انوساهَة، موضؼيا ٍكون خارج امخجوًف امفموي، يف حمفظة و ميخد هظاهما املنَوي مَفرغ افرازاهتا. وًوخد أًضا" امؼدًد من امغدد انوؼاتَة امطغرية ، انوساهَة، اتحنكِة، ادلىوزيًة، انوساهَة احلنكِة وما كبل امرخوًة، ٍكون موضؼيا مﻷسفل و مضن امغشاء ااطي، غري حماطة مبحفظة مع هجاز كنَوي كطري. افرازات امغدد انوؼاتَة ام ئرُسة مُست مدشاهبة. امغدة امفكِة ثفرز مؼاب مطيل غين ابﻷمِﻻز، وامغدة حتت امفكِة ثنذج مؼاب غين اباط، أما امغدة حتت انوساهَة ثنذج مؼااب" مزخا". ثبؼا" ميذه اﻷخذﻻفات، انوؼاب املوحود يق امفم ٌشار امَو مكزجي. ح كرَة املزجي انوؼايب مُس ثس َطا" واملادة اﻷضافِة اموػة من لك املفرزات انوؼاتَة، اكمؼدًد من امربوثُنات ثنذلل ثرسػة وثوخطق هبدروكس َل اﻷتُذاًت مﻷس نان و سطوح ااطَة امفموًة. ثبدأ أمراض امغدد انوؼاتَة ػادة تخغريات اندرة يف املفرزات و ام كرتَة، وىذه امخغريات ثؤثر اثهواي" من خﻻل جشلك انووحية اجلرثومِة و املوح، اميت تدورىا ثؤدي اىل خنور مذفش َة وأمراض وس َج دامعة. ىذه اﻷمراض ميكن أن ثطبح شدًدة تؼد املؼاجلة امشؼاغَة ﻷن امؼدًد من احلاﻻت اجليازًة )مثل امسكري، امخوَف اهكُيس( ثؤثر يف اجلراين انوؼايب، و ٌش خيك املرض من حفاف يف امفم. -

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -
Anatomical Overview
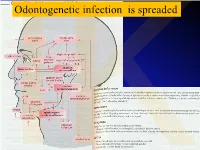
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Infraclavicular Topography of the Brachial Plexus Fascicles in Different Upper Limb Positions
Int. J. Morphol., 34(3):1063-1068, 2016. Infraclavicular Topography of the Brachial Plexus Fascicles in Different Upper Limb Positions Topografía Infraclavicular de los Fascículos del Plexo Braquial en Diferentes Posiciones del Miembro Superior Daniel Alves dos Santos*; Amilton Iatecola*; Cesar Adriano Dias Vecina*; Eduardo Jose Caldeira**; Ricardo Noboro Isayama**; Erivelto Luis Chacon**; Marianna Carla Alves**; Evanisi Teresa Palomari***; Maria Jose Salete Viotto**** & Marcelo Rodrigues da Cunha*,** ALVES DOS SANTOS, D.; IATECOLA, A.; DIAS VECINA, C. A.; CALDEIRA, E. J.; NOBORO ISAYAMA, R.; CHACON, E. L.; ALVES, M. C.; PALOMARI, E. T.; SALETE VIOTTO, M. J. & RODRIGUES DA CUNHA, M. Infraclavicular topography of the brachial plexus fascicles in different upper limb positions. Int. J. Morphol., 34 (3):1063-1068, 2016. SUMMARY: Brachial plexus neuropathies are common complaints among patients seen at orthopedic clinics. The causes range from traumatic to occupational factors and symptoms include paresthesia, paresis, and functional disability of the upper limb. Treatment can be surgical or conservative, but detailed knowledge of the brachial plexus is required in both cases to avoid iatrogenic injuries and to facilitate anesthetic block, preventing possible vascular punctures. Therefore, the objective of this study was to evaluate the topography of the infraclavicular brachial plexus fascicles in different upper limb positions adopted during some clinical procedures. A formalin- preserved, adult, male cadaver was used. The infraclavicular and axillary regions were dissected and the distance of the brachial plexus fascicles from adjacent bone structures was measured. No anatomical variation in the formation of the brachial plexus was observed. The metric relationships between the brachial plexus and adjacent bone prominences differed depending on the degree of shoulder abduction. -

Pocket Atlas of Human Anatomy 4Th Edition
I Pocket Atlas of Human Anatomy 4th edition Feneis, Pocket Atlas of Human Anatomy © 2000 Thieme All rights reserved. Usage subject to terms and conditions of license. III Pocket Atlas of Human Anatomy Based on the International Nomenclature Heinz Feneis Wolfgang Dauber Professor Professor Formerly Institute of Anatomy Institute of Anatomy University of Tübingen University of Tübingen Tübingen, Germany Tübingen, Germany Fourth edition, fully revised 800 illustrations by Gerhard Spitzer Thieme Stuttgart · New York 2000 Feneis, Pocket Atlas of Human Anatomy © 2000 Thieme All rights reserved. Usage subject to terms and conditions of license. IV Library of Congress Cataloging-in-Publication Data is available from the publisher. 1st German edition 1967 2nd Japanese edition 1983 7th German edition 1993 2nd German edition 1970 1st Dutch edition 1984 2nd Dutch edition 1993 1st Italian edition 1970 2nd Swedish edition 1984 2nd Greek edition 1994 3rd German edition 1972 2nd English edition 1985 3rd English edition 1994 1st Polish edition 1973 2nd Polish edition 1986 3rd Spanish edition 1994 4th German edition 1974 1st French edition 1986 3rd Danish edition 1995 1st Spanish edition 1974 2nd Polish edition 1986 1st Russian edition 1996 1st Japanese edition 1974 6th German edition 1988 2nd Czech edition 1996 1st Portuguese edition 1976 2nd Italian edition 1989 3rd Swedish edition 1996 1st English edition 1976 2nd Spanish edition 1989 2nd Turkish edition 1997 1st Danish edition 1977 1st Turkish edition 1990 8th German edition 1998 1st Swedish edition 1979 1st Greek edition 1991 1st Indonesian edition 1998 1st Czech edition 1981 1st Chinese edition 1991 1st Basque edition 1998 5th German edition 1982 1st Icelandic edition 1992 3rd Dutch edtion 1999 2nd Danish edition 1983 3rd Polish edition 1992 4th Spanish edition 2000 This book is an authorized and revised translation of the 8th German edition published and copy- righted 1998 by Georg Thieme Verlag, Stuttgart, Germany. -

Unusual Organization of the Ansa Cervicalis: a Case Report
CASE REPORT ISSN- 0102-9010 UNUSUAL ORGANIZATION OF THE ANSA CERVICALIS: A CASE REPORT Ranjana Verma1, Srijit Das2 and Rajesh Suri3 Department of Anatomy, Maulana Azad Medical College, New Delhi-110002, India. ABSTRACT The superior root of the ansa cervicalis is formed by C1 fibers carried by the hypoglossal nerve, whereas the inferior root is contributed by C2 and C3 nerves. We report a rare finding in a 40-year-old male cadaver in which the vagus nerve fused with the hypoglossal nerve immediately after its exit from the skull on the left side. The vagus nerve supplied branches to the sternohyoid, sternothyroid and superior belly of the omohyoid muscles and also contributed to the formation of the superior root of the ansa cervicalis. In this arrangement, paralysis of the infrahyoid muscles may result following lesion of the vagus nerve anywhere in the neck. The cervical location of the vagus nerve was anterior to the common carotid artery within the carotid sheath. This case report may be of clinical interest to surgeons who perform laryngeal reinnervation and neurologists who diagnose nerve disorders. Key words: Ansa cervicalis, hypoglossal nerve, vagus nerve, variations INTRODUCTION cadaver. The right side was normal. The neck region The ansa cervicalis is a nerve loop formed was dissected and the neural structures in the carotid by the union of superior and inferior roots. The and muscular triangle regions were exposed, with superior root is a branch of the hypoglossal nerve particular attention given to the organization of the containing C1 fibers, whereas the inferior root is ansa cervicalis. -

Communication Between the Mylohyoid and Lingual Nerves: Clinical Implications
Int. J. Morphol., Case Report 25(3):561-564, 2007. Communication Between the Mylohyoid and Lingual Nerves: Clinical Implications Comunicación entre los Nervios Milohioideo y Lingual: Implicancias Clínicas *Valéria Paula Sassoli Fazan; **Omar Andrade Rodrigues Filho & ***Fernando Matamala FAZAN, V. P. S.; RODRIGUES FILHO, O. A. & MATAMALA, F. Communication between the mylohyoid and lingual nerves: Clinical implications. Int. J. Morphol., 25(3):561-564, 2007. SUMMARY: The mylohyoid muscle plays an important role in chewing, swallowing, respiration and phonation, being the mylohyoid nerve also closely related to these important functions. It has been postulated that the mylohyoid nerve might have a role in the sensory innervation of the chin and the lower incisor teeth while the role of the mylohyoid nerve in the mandibular posterior tooth sensation is still a controversial issue. Although variations in the course of the mylohyoid nerve in relation to the mandible are frequently found on the dissecting room, they have not been satisfactorily described in the anatomical or surgical literature. It is well known that variations on the branching pattern of the mandibular nerve frequently account for the failure to obtain adequate local anesthesia in routine oral and dental procedures and also for the unexpected injury to branches of the nerves during surgery. Also, anatomical variations might be responsible for unexpected and unexplained symptoms after a certain surgical procedure. We describe the presence of a communicating branch between the mylohyoid and lingual nerves in an adult male cadaver, and discuss its clinical/surgical implications as well as its possible role on the sensory innervation of the tongue. -

Variation of the Infrahyoid Muscle: Duplicated Omohyoid and Appearance of the Levator Glandulae Thyroideae Muscles
DOI 10.3349/ymj.2010.51.6.984 Case Report pISSN: 0513-5796, eISSN: 1976-2437 Yonsei Med J 51(6):984-986, 2010 Variation of the Infrahyoid Muscle: Duplicated Omohyoid and Appearance of the Levator Glandulae Thyroideae Muscles Deog-Im Kim,1 Ho-Jeong Kim,2 Jae-Young Park,2 and Kyu-Seok Lee2 1Department of Anatomy, Catholic Institution for Applied Anatomy, College of Medicine, The Catholic University of Korea, Seoul; 2Department of Anatomy, Kwandong University College of Medicine, Gangneung, Korea. Received: November 21, 2008 The embryologic origin of the omohyoid muscle is different from that of the other Revised: March 23, 2009 neck muscles. A number of variations such as the absence of muscle, variable sites Accepted: March 27, 2009 of origin and insertion, and multiple bellies have been reported. However, varia- Corresponding author: Dr. Kyu-Seok Lee, tions in the inferior belly of the omohyoid muscle are rare. There have been no Department of Anatomy, Kwandong University reports of the combined occurrence of the omohyoid muscle variation with the College of Medicine, 522 Naegok-dong, appearance of the levator glandulase thyroideae muscle. Routine dissection of a 51- Gangneung 210-701, Korea. year-old female cadaver revealed a duplicated omohyoid muscle and the appea- Tel: 82-33-649-7473, Fax: 82-33-641-1074 rance of the levator glandulae thyroideae muscle. In this case, the two inferior E-mail: [email protected] bellies of the omohyoid muscle were found to originate inferiorly from the superior border of the scapula. One of the inferior bellies generally continued to the superior ∙The authors have no financial conflicts of belly with the tendinous intersection. -
MSS 1. a Patient Presented to a Traumatologist with a Trauma Of
MSS 1. A patient presented to a traumatologist with a trauma of shoulder. What wall of axillary cavity contains foramen trilaterum and foramen quadrilaterum? a) anterior b) posterior c) lateral d) medial e) intermediate 2. A patient presented to a traumatologist with a trauma of leg, which he had sustained at a sport competition. Upon examination, damage of posterior muscle, that is attached to calcaneus by its tendon, was found. This muscle is: a) triceps surae b) tibialis posterior c) popliteus d) fibularis longus e) fibularis brevis 3. In the course of a cesarean section, an incision was made in the pubic area and vagina of rectus abdominis muscle was cut. What does anterior wall of the vagina of rectus abdominis muscle consist of? A. aponeurosis of m. transversus abdominis, m. obliquus internus abdominis. B. aponeurosis of m. transversus abdominis, m. pyramidalis. C. aponeurosis of m. obliquus internus abdominis, m. obliquus externus abdominis. D. aponeurosis of m. transversus abdominis, m. obliquus externus abdominis. E. aponeurosis of m. transversus abdominis, m. obliquus internus abdominis 4. A 30 year-old woman complained of pain in the lower part of her forearm. Traumatologist found that her radio-carpal joint was damaged. This joint is: A. complex, ellipsoid B.simple, ellipsoid C.complex, cylindrical D.simple, cylindrical E.complex condylar 5. A woman was brought by an ambulance to the emergency department with a trauma of the cervical part of her vertebral column. Radiologist diagnosed a fracture of a nonbifid spinous processes of one of her cervical vertebrae. Spinous process of what cervical vertebra is fractured? A.VI. -

The Digastric Muscle's Anterior Accessory Belly: Case Report
Med Oral Patol Oral Cir Bucal 2007;12:E341-3. The digastric muscle’s anterior accessory belly Med Oral Patol Oral Cir Bucal 2007;12:E341-3. The digastric muscle’s anterior accessory belly The digastric muscle’s anterior accessory belly: Case report Genny Reyes 1, Camilo Contreras 2, Luis Miguel Ramírez 3, Luis Ernesto Ballesteros 4 (1) Medicine Student. First Semester. Universidad Industrial de Santander (UIS), Bucaramanga (2) Medicine Student. Third Semester. Universidad Industrial de Santander (UIS), Bucaramanga (3) Doctor of Prosthetic Dentistry and Temporomandibular Disorders from Universidad Javeriana, Santa fe de Bogota, Colombia. Associate Professor of Morphology, Department of Basic Sciences at the Universidad Industrial de Santander (UIS), Bucaramanga (4) Medical Doctor. Degree in Basic Sciences, Universidad del Valle, Cali, Colombia. Director of the Basic Sciences Department at Universidad Industrial de Santander (UIS), Bucaramanga, Colombia Correspondence: Dr. Luis Miguel Ramirez Aristeguieta E-mail: [email protected] Reyes G, Contreras C, Ramirez LM, Ballesteros LE. The digastric Received: 23-05-2006 muscle’s anterior accessory belly: Case report. Med Oral Patol Oral Cir Accepted: 10-04-2007 Bucal 2007;12:E341-3. © Medicina Oral S. L. C.I.F. B 96689336 - ISSN 1698-6946 Indexed in: -Index Medicus / MEDLINE / PubMed -EMBASE, Excerpta Medica -SCOPUS -Indice Médico Español -IBECS ABStract Digastric muscle is characterized by presenting occasional variations. The suprahyoid region of an 83 year-old male cadaver was dissected and an anatomic variation of the digastric muscle was observed in its anterior belly. It consisted of an accessory bilateral anterior belly originating in the intermediate tendon and inserted into the mylohyoid raphe. -

Fig. 2-32 Facial Muscles. Fig. 2-33 Trigeminal Nerve (CN V)
Fig. 2-32 Facial Muscles. Fig. 2-33 Trigeminal Nerve (CN V) leaving the Skull. 51 thetic agent at the infraorbital foramen or in the infraor- posterior to its head and anterior to the auricle. It then bital canal (e.g., for treatment of wounds of the upper crosses over the root of the zygomatic process of the lip and cheek or for repairing the maxillary incisor teeth). temporal bone, deep to the superficial temporal artery. The site of emergence of this nerve can easily be deter- As its name suggests, it supplies parts of the auricle, mined by exerting pressure on the maxilla in the region external acoustic meatus, tympanic membrane (ear- of the infraorbital foramen and nerve. Pressure on the drum), and skin in the temporal region. The inferior al- nerve causes considerable pain. Care is exercised when veolar nerve is the large terminal branch of the posterior performing an infraorbital nerve block because compan- division of CN V3; the lingual nerve is the other terminal ion infraorbital vessels leave the infraorbital foramen with branch. It enters the mandibular canal through the man- the nerve. Careful aspiration of the syringe during injec- dibular foramen. In the canal it gives off branches that tion prevents inadvertent injection of the anesthetic fluid supply the mandibular (lower) teeth. Opposite the mental into a blood vessel. The orbit is located just superior to foramen, the inferior alveolar nerve divides into its ter- the injection site. A careless injection could result in minal incisive and mental branches. The incisive nerve the passage of anesthetic fluid into the orbit, causing supplies the incisor teeth, the adjacent gingiva, and temporary paralysis of the extraocular muscles.