Common Phototherapy Mistakes & How to Avoid Them
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dermatology Eponyms – Sign –Lexicon (P)
2XU'HUPDWRORJ\2QOLQH Historical Article Dermatology Eponyms – sign –Lexicon (P)� Part 2 Piotr Brzezin´ ski1,2, Masaru Tanaka3, Husein Husein-ElAhmed4, Marco Castori5, Fatou Barro/Traoré6, Satish Kashiram Punshi7, Anca Chiriac8,9 1Department of Dermatology, 6th Military Support Unit, Ustka, Poland, 2Institute of Biology and Environmental Protection, Department of Cosmetology, Pomeranian Academy, Slupsk, Poland, 3Department of Dermatology, Tokyo Women’s Medical University Medical Center East, Tokyo, Japan, 4Department of Dermatology, San Cecilio University Hospital, Granada, Spain, 5Medical Genetics, Department of Experimental Medicine, Sapienza - University of Rome, San Camillo-Forlanini Hospital, Rome, Italy, 6Department of Dermatology-Venerology, Yalgado Ouédraogo Teaching Hospital Center (CHU-YO), Ouagadougou, Burkina Faso, 7Consultant in Skin Dieseases, VD, Leprosy & Leucoderma, Rajkamal Chowk, Amravati – 444 601, India, 8Department of Dermatology, Nicolina Medical Center, Iasi, Romania, 9Department of Dermato-Physiology, Apollonia University Iasi, Strada Muzicii nr 2, Iasi-700399, Romania Corresponding author: Piotr Brzezin′ski, MD PhD, E-mail: [email protected] ABSTRACT Eponyms are used almost daily in the clinical practice of dermatology. And yet, information about the person behind the eponyms is difficult to find. Indeed, who is? What is this person’s nationality? Is this person alive or dead? How can one find the paper in which this person first described the disease? Eponyms are used to describe not only disease, but also clinical signs, surgical procedures, staining techniques, pharmacological formulations, and even pieces of equipment. In this article we present the symptoms starting with (P) and other. The symptoms and their synonyms, and those who have described this symptom or phenomenon. Key words: Eponyms; Skin diseases; Sign; Phenomenon Port-Light Nose sign or tylosis palmoplantaris is widely related with the onset of squamous cell carcinoma of the esophagus. -

Living with Mast Cell Activation Syndrome
Anne Maitland, MD, PhD Living with Medical Director, Comprehensive Allergy Mast Cell & Asthma Care Activation Asst Professor, Dept of Medicine – Clinical Immunology Syndrome Icahn School of Medicine at Mt Sinai, New York Got MCAS? Mast Cell mediated disorders are common u 1 out of 2 of us are coping with some chronic immune mediated disorder. o ‘allergies’(rhinitis), sinus infections, hives (urticaria),food allergy/intolerance, skin swelling (angioedema), Anaphylaxis Signs and Symptoms eczema (atopic dermatitis and contact dermatitis), asthma issues, and the prototype of immediate hypersensitivity syndromes, anaphylaxis Why the rise in hypersensitivity disorders? Our genes in this environment! The human race has come to dominate its environment so completely that any analysis of the increase or appearance of a disease has to take changes in our lifestyle into account. In the case of allergic disease [hypersensitivity disorders] changes in our environment, diet, water quality, and personal behavior over the last 150 years have played a dominant role in the specificity of these diseases, as well as in prevalence and severity… it is clear that the consequences of hygiene, indoor entertainment, and changes in diet or physical activity have never been predicted. Thomas A. E. Platts-Mills, MD, PhD, FRS, The allergy epidemics: 1870-2010; J Allergy Clin Immunol 2015;136:3-13. Why? Trauma Stress Infection Connective Tissue Chemical Disorder exposure PIDD -manufactured Autoimmune Dz. -mold, Mastocytosis mycotoxins Hypertryptasemia (naturally Atopic Disorders occuring) Mast cell activation syndrome is easily treated, if it's But most patients with recognized MCAD suffer for Patients with mast cell activation syndrome (MCAS) frequently go for years without an accurate diagnosis… Harding, Reuters Health-New York, 2011 years… It is very common for one hypersensitivity condition to progress/morph into another, be provoked by more triggers. -

Immunohistochemical Analysis of S100-Positive Epidermal
An Bras Dermatol. 2020;95(5):627---630 Anais Brasileiros de Dermatologia www.anaisdedermatologia.org.br DERMATOPATHOLOGY Immunohistochemical analysis of S100-positive ଝ,ଝଝ epidermal Langerhans cells in dermatofibroma Mahmoud Rezk Abdelwhaed Hussein Department of Pathology, Assuit University Hospital, Assuit, Egypt Received 3 February 2020; accepted 12 April 2020 Available online 12 July 2020 Abstract Dermatofibroma is a dermal fibrohistiocytic neoplasm. The Langerhans cells are the KEYWORDS immunocompetent cells of the epidermis, and they represent the first defense barrier of the Histiocytoma, benign immune system towards the environment. The objective was to immunohistologically compare fibrous; the densities of S100-positive Langerhans cells in the healthy peritumoral epidermis against Skin neoplasms; those in the epidermis overlying dermatofibroma (20 cases), using antibodies against the S100 S100 Proteins molecule (the immunophenotypic hallmark of Langerhans cells). The control group (normal, healthy skin) included ten healthy age and sex-matched individuals who underwent skin biopsies for benign skin lesions. A significantly high density of Langerhans cells was observed both in the epidermis of the healthy skin (6.00 ± 0.29) and the peritumoral epidermis (6.44 ± 0.41) vs. those in the epidermis overlying the tumor (1.44 ± 0.33, p < 0.05). The quantitative deficit of Langerhans cells in the epidermis overlying dermatofibroma may be a possible factor in its development. © 2020 Sociedade Brasileira de Dermatologia. Published by Elsevier Espana,˜ S.L.U. This is an open access article under the CC BY license (http://creativecommons.org/licenses/by/4.0/). Langerhans cells (LCs) are the exclusive antigen-presenting tions stained with hematoxylin and eosin as ‘‘clear cells’’ cells of the normal human epidermis. -

Storiform Collagenoma: Case Report Colagenoma Estoriforme: Relato De Caso
CASE REPORT Storiform collagenoma: case report Colagenoma estoriforme: relato de caso Guilherme Flosi Stocchero1 ABSTRACT INTRODUCTION Storiform collagenoma is a rare tumor, which originates from the Storiform collagenoma or sclerotic fibroma is a rare proliferation of fibroblasts that show increased production of type-I benign skin tumor that usually affects young adults collagen. It is usually found in the face, neck and extremities, but and middle-age individuals of both sexes. This tumor is it can also appear in the trunk, scalp and, less frequently, in the slightly predominant in women. Storiform collagenoma oral mucosa and the nail bed. It affects both sexes, with a slight female predominance. It may be solitary or multiple, the latter being appears as a small papule or solid fibrous nodule. an important marker for Cowden syndrome. It presents as a painless, It is well-circumscribed, pink, whitish or skin color, solid nodular tumor that is slow-growing. It must be considered in the painless and of slow-growing. This tumor is often differential diagnosis of other well-circumscribed skin lesions, such as found in face and limbs, but it can also appears in dermatofibroma, pleomorphic fibroma, sclerotic lipoma, fibrolipoma, the chest, scalp and, rarely, in oral mucosa and nail giant cell collagenoma, benign fibrous histiocytoma, intradermal Spitz bed. Storiform collagenoma often appears as single nevus and giant cell angiohistiocytoma. tumor, and the occurrence of multiple tumors is an important indication of Cowden syndrome, which is Keywords: Collagen; Hamartoma; Skin neoplasms; Fibroma; Skin; Case a heritage genodermatosis of autosomal dominant reports condition.(1-4) Storiform collagenoma has as differential diagnosis other well-circumscribed skin tumors such RESUMO as dermatofibroma, pleomorphic fibroma, sclerotic O colagenoma estoriforme é um tumor raro originado a partir da lipoma, fibrolipoma, giant cell collagenoma, benign proliferação de fibroblastos com produção aumentada de colágeno tipo I. -
Guide to Policy & Practice Questions
OREGON BOARD OF CHIROPRACTIC EXAMINERS GUIDE TO POLICY & PRACTICE QUESTIONS 530 Center St NE, suite 620 Salem, OR 97301 (503) 378-5816 [email protected] Updated/Adopted: 9/17/2020 TABLE OF CONTENTS SECTION I ............................................................................................................................................................................................... 6 DEVICES, PROCEDURES, AND SUBSTANCES ............................................................................................................................... 6 DEVICES ................................................................................................................................................................ 6 BAX 3000 AND SIMILAR DEVICES................................................................................................................................................ 6 BIOPTRON LIGHT THERAPY ........................................................................................................................................................ 6 CPAP MACHINE, ORDERING ....................................................................................................................................................... 6 CTD MARK I MULTI-TORSION TRACTION DEVICE................................................................................................................... 6 DYNATRON 2000 ........................................................................................................................................................................... -
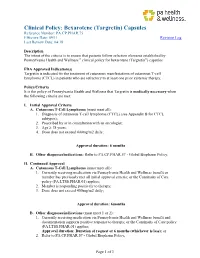
Bexarotene (Targretin) Capsules Reference Number: PA.CP.PHAR.75 Effective Date: 09/11 Revision Log Last Review Date: 04/18
Clinical Policy: Bexarotene (Targretin) Capsules Reference Number: PA.CP.PHAR.75 Effective Date: 09/11 Revision Log Last Review Date: 04/18 Description The intent of the criteria is to ensure that patients follow selection elements established by Pennsylvania Health and Wellness ® clinical policy for bexarotene (Targretin®) capsules FDA Approved Indication(s) Targretin is indicated for the treatment of cutaneous manifestations of cutaneous T-cell lymphoma (CTCL) in patients who are refractory to at least one prior systemic therapy. Policy/Criteria It is the policy of Pennsylvania Health and Wellness that Targretin is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Cutaneous T-Cell Lymphoma (must meet all): 1. Diagnosis of cutaneous T-cell lymphoma (CTCL) (see Appendix B for CTCL subtypes); 2. Prescribed by or in consultation with an oncologist; 3. Age ≥ 18 years; 4. Dose does not exceed 400mg/m2 daily; Approval duration: 6 months B. Other diagnoses/indications: Refer to PA.CP.PHAR.57 - Global Biopharm Policy. II. Continued Approval A. Cutaneous T-Cell Lymphoma (must meet all): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit or member has previously met all initial approval criteria; or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; 2. Member is responding positively to therapy; 3. Dose does not exceed 400mg/m2 daily; Approval duration: 6months B. Other diagnoses/indications (must meet 1 or 2): 1. Currently receiving medication via Pennsylvania Health and Wellness benefit and documentation supports positive response to therapy; or the Continuity of Care policy (PA.LTSS.PHAR.01) applies; Approval duration: Duration of request or 6 months (whichever is less); or 2. -

Clinicopathological Correlation of Acquired Hyperpigmentary Disorders
Symposium Clinicopathological correlation of acquired Dermatopathology hyperpigmentary disorders Anisha B. Patel, Raj Kubba1, Asha Kubba1 Department of Dermatology, ABSTRACT Oregon Health Sciences University, Portland, Oregon, Acquired pigmentary disorders are group of heterogenous entities that share single, most USA, 1Delhi Dermatology Group, Delhi Dermpath significant, clinical feature, that is, dyspigmentation. Asians and Indians, in particular, are mostly Laboratory, New Delhi, India affected. Although the classic morphologies and common treatment options of these conditions have been reviewed in the global dermatology literature, the value of histpathological evaluation Address for correspondence: has not been thoroughly explored. The importance of accurate diagnosis is emphasized here as Dr. Asha Kubba, the underlying diseases have varying etiologies that need to be addressed in order to effectively 10, Aradhana Enclave, treat the dyspigmentation. In this review, we describe and discuss the utility of histology in the R.K. Puram, Sector‑13, diagnostic work of hyperpigmentary disorders, and how, in many cases, it can lead to targeted New Delhi ‑ 110 066, India. E‑mail: and more effective therapy. We focus on the most common acquired pigmentary disorders [email protected] seen in Indian patients as well as a few uncommon diseases with distinctive histological traits. Facial melanoses, including mimickers of melasma, are thoroughly explored. These diseases include lichen planus pigmentosus, discoid lupus erythematosus, drug‑induced melanoses, hyperpigmentation due to exogenous substances, acanthosis nigricans, and macular amyloidosis. Key words: Facial melanoses, histology of hyperpigmentary disorders and melasma, pigmentary disorders INTRODUCTION focus on the most common acquired hyperpigmentary disorders seen in Indian patients as well as a few Acquired pigmentary disorders are found all over the uncommon diseases with distinctive histological traits. -

Dermatologic Manifestations of Hermansky-Pudlak Syndrome in Patients with and Without a 16–Base Pair Duplication in the HPS1 Gene
STUDY Dermatologic Manifestations of Hermansky-Pudlak Syndrome in Patients With and Without a 16–Base Pair Duplication in the HPS1 Gene Jorge Toro, MD; Maria Turner, MD; William A. Gahl, MD, PhD Background: Hermansky-Pudlak syndrome (HPS) con- without the duplication were non–Puerto Rican except sists of oculocutaneous albinism, a platelet storage pool de- 4 from central Puerto Rico. ficiency, and lysosomal accumulation of ceroid lipofuscin. Patients with HPS from northwest Puerto Rico are homozy- Results: Both patients homozygous for the 16-bp du- gous for a 16–base pair (bp) duplication in exon 15 of HPS1, plication and patients without the duplication dis- a gene on chromosome 10q23 known to cause the disorder. played skin color ranging from white to light brown. Pa- tients with the duplication, as well as those lacking the Objective: To determine the dermatologic findings of duplication, had hair color ranging from white to brown patients with HPS. and eye color ranging from blue to brown. New findings in both groups of patients with HPS were melanocytic Design: Survey of inpatients with HPS by physical ex- nevi with dysplastic features, acanthosis nigricans–like amination. lesions in the axilla and neck, and trichomegaly. Eighty percent of patients with the duplication exhibited fea- Setting: National Institutes of Health Clinical Center, tures of solar damage, including multiple freckles, stel- Bethesda, Md (a tertiary referral hospital). late lentigines, actinic keratoses, and, occasionally, basal cell or squamous cell carcinomas. Only 8% of patients Patients: Sixty-five patients aged 3 to 54 years were di- lacking the 16-bp duplication displayed these findings. -

A Genome-Wide Association Study Reveals a Locus for Bilateral Iridal Hypopigmentation in Holstein Friesian Cattle Anne K
Hollmann et al. BMC Genetics (2017) 18:30 DOI 10.1186/s12863-017-0496-4 RESEARCHARTICLE Open Access A genome-wide association study reveals a locus for bilateral iridal hypopigmentation in Holstein Friesian cattle Anne K. Hollmann1, Martina Bleyer2, Andrea Tipold3, Jasmin N. Neßler3, Wilhelm E. Wemheuer1, Ekkehard Schütz1 and Bertram Brenig1* Abstract Background: Eye pigmentation abnormalities in cattle are often related to albinism, Chediak-Higashi or Tietz like syndrome. However, mutations only affecting pigmentation of coat color and eye have also been described. Herein 18 Holstein Friesian cattle affected by bicolored and hypopigmented irises have been investigated. Results: Affected animals did not reveal any ophthalmological or neurological abnormalities besides the specific iris color differences. Coat color of affected cattle did not differ from controls. Histological examination revealed a reduction of melanin pigment in the iridal anterior border layer and stroma in cases as cause of iris hypopigmentation. To analyze the genetics of the iris pigmentation differences, a genome-wide association study was performed using Illumina BovineSNP50 BeadChip genotypes of the 18 cases and 172 randomly chosen control animals. A significant association on bovine chromosome 8 (BTA8) was identified at position 60,990,733 with a -log10(p) = 9.17. Analysis of genotypic and allelic dependences between cases of iridal hypopigmentation and an additional set of 316 randomly selected Holstein Friesian cattle controls showed that allele A at position 60,990,733 on BTA8 (P =4.0e–08, odds ratio = 6.3, 95% confidence interval 3.02–13.17) significantly increased the chance of iridal hypopigmentation. Conclusions: The clinical appearance of the iridal hypopigmentation differed from previously reported cases of pigmentation abnormalities in syndromes like Chediak-Higashi or Tietz and seems to be mainly of cosmetic character. -

RD-Action Matchmaker – Summary of Disease Expertise Recorded Under
Summary of disease expertise recorded via RD-ACTION Matchmaker under each Thematic Grouping and EURORDIS Members’ Thematic Grouping Thematic Reported expertise of those completing the EURORDIS Member perspectives on Grouping matchmaker under each heading Grouping RD Thematically Rare Bone Achondroplasia/Hypochondroplasia Achondroplasia Amelia skeletal dysplasia’s including Achondroplasia/Growth hormone cleidocranial dysostosis, arthrogryposis deficiency/MPS/Turner Brachydactyly chondrodysplasia punctate Fibrous dysplasia of bone Collagenopathy and oncologic disease such as Fibrodysplasia ossificans progressive Li-Fraumeni syndrome Osteogenesis imperfecta Congenital hand and fore-foot conditions Sterno Costo Clavicular Hyperostosis Disorders of Sex Development Duchenne Muscular Dystrophy Ehlers –Danlos syndrome Fibrodysplasia Ossificans Progressiva Growth disorders Hypoparathyroidism Hypophosphatemic rickets & Nutritional Rickets Hypophosphatasia Jeune’s syndrome Limb reduction defects Madelung disease Metabolic Osteoporosis Multiple Hereditary Exostoses Osteogenesis imperfecta Osteoporosis Paediatric Osteoporosis Paget’s disease Phocomelia Pseudohypoparathyroidism Radial dysplasia Skeletal dysplasia Thanatophoric dwarfism Ulna dysplasia Rare Cancer and Adrenocortical tumours Acute monoblastic leukaemia Tumours Carcinoid tumours Brain tumour Craniopharyngioma Colon cancer, familial nonpolyposis Embryonal tumours of CNS Craniopharyngioma Ependymoma Desmoid disease Epithelial thymic tumours in -

Dermatofibrosarcoma Protuberans and Dermatofibroma: Dermal Dendrocytomas? a Ultrastructural Study
Dermatofibrosarcoma Protuberans and Dermatofibroma: Dermal Dendrocytomas? A Ultrastructural Study Hugo Dominguez-Malagon, M.D., Ana Maria Cano-Valdez, M.D. Department of Pathology, Instituto Nacional de Cancerología, Mexico. ABSTRACT population of plump spindled cells devoid of cell processes, these cells contained intracytoplasmic lipid droplets and rare Dermatofibroma (DF) and Dermatofibrosarcoma subplasmalemmal densities but lacked MVB. Protuberans (DFSP) are dermal tumors whose histogenesis has not been well defined to date. The differential diagnosis in most With the ultrastructural characteristics and the constant cases is established in routine H/E sections and may be confirmed expression of CD34 in DFSP, a probable origin in dermal by immunohistochemistry; however there are atypical variants dendrocytes is postulated. The histogenesis of DF remains of DF with less clear histological differences and non-conclusive obscure. immunohistochemical results. In such cases electron microscopy studies may be useful to establish the diagnosis. INTRODUCTION In the present paper the ultrastructural characteristics of 38 The histogenesis or differentiation of cases of DFSP and 10 cases of DF are described in detail, the Dermatofibrosarcoma Protuberans (DFSP) and objective was to identify some features potentially useful for Dermatofibroma (DF) is controversial in the literature. For differential diagnosis, and to identify the possible histogenesis of DFSP diverse origins such as fibroblastic,1 fibro-histiocytic2 both neoplasms. Schwannian,3 myofibroblastic,4 perineurial,5,6 and endoneurial (7) have been postulated. DFSP in all cases was formed by stellate or spindled cells with long, slender, ramified cell processes joined by primitive junctions, Regarding DF, most authors are in agreement of a subplasmalemmal densities were frequently seen in the processes. -

Multi-Organ Teratogenesis Sequels of Bigger Size Particles Colloidal
ytology & f C H o is Prakash, et al., J Cytol Histol 2018, 9:2 l t a o n l o r DOI: 10.4172/2157-7099.1000501 g u y o J Journal of Cytology & Histology ISSN: 2157-7099 Research Article Open Access Multi-Organ Teratogenesis Sequels of Bigger Size Particles Colloidal Silver in Primate Vertebrates Pani Jyoti Prakash*1, Singh Royana2 and Pani Sankarsan3 1Department of Anatomy, Faculty of Medicine, Institute of Medical Science and Research, Karjat, Bhivpuri, India 2Department of Anatomy, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttarpradesh, India 3Deapartment of Surgery, Institute of Medical Science and Research, Karjat, Bhivpuri, India *Corresponding author: Prakash PJ, Department of Anatomy, Faculty of Medicine, Institute of Medical Science and Research, Karjat, Bhivpuri, India, Tel: 8433668356; E-mail: [email protected] Received date: February 21, 2018; Accepted date: March 12, 2018; Published date: March 16, 2018 Copyright: © 2018 Prakash PJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Back ground: In this most recent, update global arena for consumers products most of the daily applications of bigger silver nano particles (20 to 100 nano meter range) are effected as anti-viral and anti-parasitic agents in clinical medicine and diagnosis which is a positive feedback. However, the major negative feedback of bigger size silver nano particles on human, animal and primate vertebrate body is multisystem teratogenicity focuses. Material and methods: This study was designed to investigate teratogenic effects of bigger size nano silver which is poly vinyl pyrollidone coated and sodium borohydride stabilized.