Radiology Notes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Update on Diagnosis and Treatment of Idiopathic Pulmonary Fibrosis
J Bras Pneumol. 2015;41(5):454-466 http://dx.doi.org/10.1590/S1806-37132015000000152 REVIEW ARTICLE Update on diagnosis and treatment of idiopathic pulmonary fibrosis José Baddini-Martinez1, Bruno Guedes Baldi2, Cláudia Henrique da Costa3, Sérgio Jezler4, Mariana Silva Lima5, Rogério Rufino3,6 1. Divisão de Pneumologia, Departamento de Clínica Médica, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo, Ribeirão Preto, Brasil. 2. Divisão de Pneumologia, Instituto do Coração, Hospital das Clínicas, ABSTRACT Faculdade de Medicina, Universidade de São Paulo, São Paulo, Brasil. Idiopathic pulmonary fibrosis is a type of chronic fibrosing interstitial pneumonia, of 3. Disciplina de Pneumologia e Tisiologia, unknown etiology, which is associated with a progressive decrease in pulmonary Faculdade de Ciências Médicas, function and with high mortality rates. Interest in and knowledge of this disorder have Universidade do Estado do Rio de grown substantially in recent years. In this review article, we broadly discuss distinct Janeiro, Rio de Janeiro, Brasil. aspects related to the diagnosis and treatment of idiopathic pulmonary fibrosis. We 4. Ambulatório de Pneumologia, Hospital list the current diagnostic criteria and describe the therapeutic approaches currently Ana Nery, Salvador, Brasil. available, symptomatic treatments, the action of new drugs that are effective in slowing 5. Ambulatório de Doenças Pulmonares Intersticiais, Hospital do Servidor the decline in pulmonary function, and indications for lung transplantation. Público Estadual de São Paulo, São Keywords: Idiopathic pulmonary fibrosis/diagnosis; Idiopathic pulmonary fibrosis/therapy; Paulo, Brasil. Idiopathic pulmonary fibrosis/rehabilitation. 6. Programa de Pós-Graduação em Ciências Médicas, Universidade do Estado do Rio de Janeiro, Rio de Janeiro, Brasil. -

Chest and Abdominal Radiograph 101
Chest and Abdominal Radiograph 101 Ketsia Pierre MD, MSCI July 16, 2010 Objectives • Chest radiograph – Approach to interpreting chest films – Lines/tubes – Pneumothorax/pneumomediastinum/pneumopericar dium – Pleural effusion – Pulmonary edema • Abdominal radiograph – Tubes – Bowel gas pattern • Ileus • Bowel obstruction – Pneumoperitoneum First things first • Turn off stray lights, optimize room lighting • Patient Data – Correct patient – Patient history – Look at old films • Routine Technique: AP/PA, exposure, rotation, supine or erect Approach to Reading a Chest Film • Identify tubes and lines • Airway: trachea midline or deviated, caliber change, bronchial cut off • Cardiac silhouette: Normal/enlarged • Mediastinum • Lungs: volumes, abnormal opacity or lucency • Pulmonary vessels • Hila: masses, lymphadenopathy • Pleura: effusion, thickening, calcification • Bones/soft tissues (four corners) Anatomy of a PA Chest Film TUBES Endotracheal Tubes Ideal location for ETT Is 5 +/‐ 2 cm from carina ‐Normal ETT excursion with flexion and extension of neck 2 cm. ETT at carina Right mainstem Intubation ‐Right mainstem intubation with left basilar atelectasis. ETT too high Other tubes to consider DHT down right mainstem DHT down left mainstem NGT with tip at GE junction CENTRAL LINES Central Venous Line Ideal location for tip of central venous line is within superior vena cava. ‐ Risk of thrombosis decreased in central veins. ‐ Catheter position within atrium increases risk of perforation Acceptable central line positions • Zone A –distal SVC/superior atriocaval junction. • Zone B – proximal SVC • Zone C –left brachiocephalic vein. Right subclavian central venous catheter directed cephalad into IJ Where is this tip? Hemiazygous Or this one? Right vertebral artery Pulmonary Arterial Catheter Ideal location for tip of PA catheter within mediastinal shadow. -

Mantke, Peitz, Surgical Ultrasound -- Index
419 Index A esophageal 218 Anorchidism 376 gallbladder 165 Aorta 364–366 A-mode imaging 97 gastric 220 abdominal aneurysm (AAA) AAA (abdominal aortic aneurysm) metastasis 142 20–21, 364, 366 20–21, 364, 366 pancreatic 149, 225 dissection 364, 366 Abdominal wall Adenofibroma, breast 263 perforation 366 abscess 300–301 Adenoma pseudoaneurysm 364 diagnostic evaluation 297 adrenal 214 Aortic rupture 20 hematoma 73, 300, 305 colorectal 231, 232 Aplasia, muscular 272 rectus sheath 297–300 duodenal papilla 229, 231 Appendicitis 1–4 hernia 300, 302–304 gallbladder 165 consequences for surgical indications for sonography 297 hepatic 54, 58, 141 treatment 2 seroma 298, 300, 305 multiple 141 sonographic criteria 1 trauma 297–300 parathyroid 213 Archiving 418 Abortion, tubal 30 renal 241 Arteriosclerosis 346, 348 Abscess thyroid 202–203 carotid artery 335, 337, 338 abdominal wall 300–301 Adenomyomatosis 8, 164, 165 plaque 337, 338, 345, 367, 370 causes 301 Adrenal glands 214–216 Arteriovenous (AV) malformation amebic 138 adenoma 214 139, 293, 326–329 breast 264 carcinoma 214 Artery chest wall 173, 178 cyst 214 carotid 334–339 diverticular 120, 123 hematoma 214 aneurysm 338 drainage 85–88, 93 hemorrhage 214 arteriosclerosis 335 hepatic 6, 138, 398 hyperplasia 214 plaque characteristics inflammatory bowel disease limpoma/myelipoma 214 337, 338, 345 116, 119 metastases 214 bifurcation 334, 337 intramural 5 sonographic criteria 214 bulb 339 lung 183, 186, 190 tuberculosis 214 dissection 338, 339, 346 pancreatic 11 Advanced dynamic flow (ADF) sonographic -

The Supine Pneumothorax
Annals of the Royal College of Surgeons of England (1987) vol. 69 The supine pneumothorax DAVID A P COOKE FRCS Surgical Registrar, Department ofSurgery, St Thomas' Hospital JULIE C COOKE FRCR* Radiological Senior Registrar, Department ofDiagnostic Radiology, Brompton Hospital, London Key words: PNEUMOTHORAX; COMPUTI ED TOMOGRAPHY; TRAUMA Summary TABLE I Causes of a pneumothorax The consequences of an undiagnosed pneumothorax can be life- threatening, particularly in patients with trauma to the head or Broncho-pulmonay pathology Traumatic injuy and in those mechanical ventilation. Yet multiple requiring Asthma it is these patients, whose films will be assessed initially by the Bronchial adenoma surgeon, who are more likely to have a chest X-ray taken in the Bronchial carcinoma Penetrating trauma supine position. The features of supine pneumothoraces are de- Emphysema Blunt trauma scribed and discussed together with radiological techniques used to Fibrosing alveolitis Inhaled foreign body confirm the diagnosis, including computed tomography (CT) Idiopathic which may be ofparticular importance in patients with associated Marfan's syndrome fatrogenic cranial trauma. Pulmonary abscess Pulmonary dysplasia CVP line insertion Introduction Pulmonary infarct Jet ventilation Pulmonary metastases Liver biopsy In a seriously ill patient or the victim of multiple trauma Pulmonoalveolar proteinosis Lung biopsy the clinical symptoms and signs of a pneumothorax may Radiation pneumonitis Oesophageal instrumentation be overshadowed by other problems. Usually in these Sarcoid PEEP ventilation circumstances a chest X-ray will be taken at the bedside Staphylococcal septicaemia Pleural aspiration with the patient supine and the appearances of a Tuberculosis Pleural biopsy pneumothorax will be different from those seen when the Tuberose sclerosis patient is upright. -

Toxicological Profile for Jp-5, Jp-8, and Jet a Fuels
TOXICOLOGICAL PROFILE FOR JP-5, JP-8, AND JET A FUELS U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Agency for Toxic Substances and Disease Registry March 2017 JP-5, JP-8, AND JET A FUELS ii DISCLAIMER Use of trade names is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry, the Public Health Service, or the U.S. Department of Health and Human Services. JP-5, JP-8, AND JET A FUELS iii UPDATE STATEMENT A Toxicological Profile for JP-5, JP-8, and Jet A Fuels, Draft for Public Comment was released in February 2016. This edition supersedes any previously released draft or final profile. Toxicological profiles are revised and republished as necessary. For information regarding the update status of previously released profiles, contact ATSDR at: Agency for Toxic Substances and Disease Registry Division of Toxicology and Human Health Sciences Environmental Toxicology Branch 1600 Clifton Road NE Mailstop F-57 Atlanta, Georgia 30329-4027 JP-5, JP-8, AND JET A FUELS iv This page is intentionally blank. JP-5, JP-8, AND JET A FUELS v FOREWORD This toxicological profile is prepared in accordance with guidelines* developed by the Agency for Toxic Substances and Disease Registry (ATSDR) and the Environmental Protection Agency (EPA). The original guidelines were published in the Federal Register on April 17, 1987. Each profile will be revised and republished as necessary. The ATSDR toxicological profile succinctly characterizes the toxicologic and adverse health effects information for these toxic substances described therein. Each peer-reviewed profile identifies and reviews the key literature that describes a substance's toxicologic properties. -

CHEST RADIOLOGY: Goals and Objectives
Harlem Hospital Center Department of Radiology Residency Training Program CHEST RADIOLOGY: Goals and Objectives ROTATION 1 (Radiology Years 1): Resident responsibilities: • ED chest CTs • Inpatient and outpatient plain films including the portable intensive care unit radiographs • Consultations with referring clinicians MEDICAL KNOWLEDGE: • Residents must demonstrate knowledge about established and evolving biomedical, clinical, and cognitive sciences and the application of this knowledge to patient care. At the end of the rotation, the resident should be able to: • Identify normal radiographic and CT anatomy of the chest • Identify and describe common variants of normal, including aging changes. • Demonstrate a basic knowledge of radiographic interpretation of atelectasis, pulmonary infection, congestive heart failure, pleural effusion and common neoplastic diseases of the chest • Identify the common radiologic manifestation of thoracic trauma, including widened mediastinum, signs of aortic laceration, pulmonary contusion/laceration, esophageal and diaphragmatic rupture. • Know the expected postoperative appearance in patients s/p thoracic surgery and the expected location of the life support and monitoring devices on chest radiographs of critically ill patients (intensive care radiology); be able to recognize malpositioned devices. • Identify cardiac enlargement and know the radiographic appearance of the dilated right vs. left atria and right vs. left ventricles, and pulmonary vascular congestion • Recognize common life-threatening -

Deep Sulcus Sign Developed in Patient with Multiple Fibrous Bands Between the Parietal and Visceral Pleura
eISSN: 2508-8033 Brief Image in Trauma pISSN: 2508-5298 Deep Sulcus Sign Developed in Patient with Multiple Fibrous Bands between the Parietal and Visceral Pleura Chan Yong Park1, Kwang Hee Yeo1, Sung Jin Park1, Ho Hyun Kim1, Chan Kyu Lee1, Seon Hee Kim1, Hyun Min Cho1, Seok Ran Yeom2 1Department of Trauma Surgery, Pusan National University Hospital, Busan, Korea 2Department of Emergency Medicine, Pusan National University Hospital, Busan, Korea A deepening of the costophrenic angle occurs in cases with a deep sulcus sign. We report a case of deep sulcus sign in a 47-year-old man who fell from the fifth floor. Supine chest radiography showed a right-sided pneumothorax with deep sulcus sign. Chest computed tomography (CT) demonstrated a large pneumothorax with multiple fibrous bands between the parietal and visceral pleura of the upper lobe of the right lung. (Trauma Image Proced 2017(1):7-9) Key Words: Pneumothorax; X-Rays; Diagnosis; Tomography, X-Ray computed CASE A 47-year-old man presented to the emergency department after falling from a fifth floor height. His vital signs were systolic blood pressure 60 mmHg, pulse rate 111 beats/min, respiration rate 31 breaths/min, body temperature, 36.4℃, and oxygen saturation 96%. The injury severity score was 29, revised trauma score 5.15, trauma and injury severity score 74.8%. His arterial blood gas analysis was pH 7.35, pCO2 29 mmHg, pO2 75 mmHg, hemoglobin 16.7, SaO2 94%, lactic acid 11.8 mmol/L, and base excess -8.0. Supine chest radiography showed a right-sided pneumothorax with a deep sulcus Fig. -

Kyomuhangi-CHS-Masters.Pdf
MAKERERE UNIVERSITY COLLEGE OF HEALTH SCIENCES DEPARTMENT OF RADIOLOGY ACCURACY OF CHEST ULTRASOUND IN DIAGNOSING PNEUMONIA IN PEDIATRIC PATIENTS AT MULAGO NATIONAL REFERRAL HOSPITAL, KAMPALA, UGANDA. PRINCIPAL INVESTIGATOR: DR KYOMUHANGI AGNES, MBChB, MUK SUPERVISORS: 1. DR BUGEZA SAM MBChB(MUK), MMED (Rad). 2. DR EREM GEOFFREY MBChB(MUST), MMED(Rad) 3. DR MWOROZI EDISON ARWANIRE MBChB(MUK), MMED (SENIOR CONSULTANT, Pead). A DISSERTATION SUBMITTED TO SCHOOL OF GRADUATE STUDIES IN PARTIAL FULLFILLMENT OF THE REQUIREMENT FOR AWARD OF THE DEGREE OF MASTERSAggie OF MEDICINE IN RADIOLOGY AT MAKERERE UNIVERSITY. [Date] AUGUST 2019 i DECLARATION I Kyomuhangi Agnes, hereby declare that the work presented in this dissertation has not been presented for any other degree in this university. Signed…………………………………. …………………………………. DR. KYOMUHANGI AGNES Date This dissertation has been submitted for examination with approval of the following supervisors; Signed…………………………………. …………………………………. DR. BUGEZA SAMUEL Date MBChB, MMed Rad Specialist Radiologist / lecturer, College of Health Sciences, Makerere University. Signed……………………………….... ………………………………….. DR. EREM GEOFFREY Date MBChB, MMed Rad Specialist Radiologist / lecturer, College of Health Sciences, Makerere University. Signed…………………………………. ……………………………………. DR. MWOROZI EDISON ARWANIRE Date MBChB, MMed Pead Consultant Pediatrician Mulago National Referral Hospital / Senior lecturer, College of Health Sciences, Makerere University. ii DEDICATION To my family, for being a constant source of inspiration, I am eternally grateful for their love, unwavering encouragement and all round support during the course of my masters programme. iii ACKNOWLEDGEMENTS The development and completion of this course/work was first of all made possible, by the Almighty God who has been faithful providing me with grace, mercy and strength. The funding to do this study was made possible by Uganda Cancer Institute (UCI-AfDB) scholarship which sponsored me throughout my masters programme and this study. -

Diagnosis of Pneumothorax in Critically Ill Adults Postgrad Med J: First Published As 10.1136/Pmj.76.897.399 on 1 July 2000
Postgrad Med J 2000;76:399–404 399 Diagnosis of pneumothorax in critically ill adults Postgrad Med J: first published as 10.1136/pmj.76.897.399 on 1 July 2000. Downloaded from James J Rankine, Antony N Thomas, Dorothee Fluechter Abstract The diagnosis of pneumothorax is estab- Box 1: Mechanisms of air entry lished from the patients’ history, physical causing pneumothorax examination and, where possible, by ra- x Chest wall damage: diological investigations. Adult respira- Trauma and surgery tory distress syndrome, pneumonia, and trauma are important predictors of pneu- x Lung surface damage: mothorax, as are various practical proce- Trauma—for example, rib fractures dures including mechanical ventilation, Iatrogenic—for example, attempted central line insertion, and surgical proce- central line insertion dures in the thorax, head, and neck and Rupture of lung cysts abdomen. Examination should include an inspection of the ventilator observations x Alveolar air leak: and chest drainage systems as well as the Barotrauma patient’s cardiovascular and respiratory Blast injury systems. x Via diaphragmatic foramina from Radiological diagnosis is normally con- peritoneal and retroperitoneal structures fined to plain frontal radiographs in the critically ill patient, although lateral im- x Via the head and neck ages and computed tomography are also important. Situations are described where an abnormal lucency or an apparent lung will then recoil away from the chest wall and a edge may be confused with a pneumotho- pneumothorax will be produced.1 rax. These may arise from outside the Air can enter the pleural space in a variety of thoracic cavity or from lung abnormali- diVerent ways that are summarised in box 1. -

Signs in Chest Imaging
Diagn Interv Radiol 2011; 17:18–29 CHEST IMAGING © Turkish Society of Radiology 2011 PICTORIAL ESSAY Signs in chest imaging Oktay Algın, Gökhan Gökalp, Uğur Topal ABSTRACT adiological practice includes classification of illnesses with similar A radiological sign can sometimes resemble a particular object characteristics through recognizable signs. Knowledge of and abil- or pattern and is often highly suggestive of a group of similar pathologies. Awareness of such similarities can shorten the dif- R ity to recognize these signs can aid the physician in shortening ferential diagnosis list. Many such signs have been described the differential diagnosis list and deciding on the ultimate diagnosis for for X-ray and computed tomography (CT) images. In this ar- ticle, we present the most frequently encountered plain film a patient. In this report, 23 important and frequently seen radiological and CT signs in chest imaging. These signs include for plain signs are presented and described using chest X-rays, computed tomog- films the air bronchogram sign, silhouette sign, deep sulcus raphy (CT) images, illustrations and photographs. sign, Continuous diaphragm sign, air crescent (“meniscus”) sign, Golden S sign, cervicothoracic sign, Luftsichel sign, scim- itar sign, doughnut sign, Hampton hump sign, Westermark Plain films sign, and juxtaphrenic peak sign, and for CT the gloved finger Air bronchogram sign sign, CT halo sign, signet ring sign, comet tail sign, CT an- giogram sign, crazy paving pattern, tree-in-bud sign, feeding Bronchi, which are not normally seen, become visible as a result of vessel sign, split pleura sign, and reversed halo sign. opacification of the lung parenchyma. -

Nursing Care in Pediatric Respiratory Disease Nursing Care in Pediatric Respiratory Disease
Nursing Care in Pediatric Respiratory Disease Nursing Care in Pediatric Respiratory Disease Edited by Concettina (Tina) Tolomeo, DNP, APRN, FNP-BC, AE-C Nurse Practitioner Director, Program Development Yale University School of Medicine Department of Pediatrics Section of Respiratory Medicine New Haven, CT A John Wiley & Sons, Inc., Publication This edition first published 2012 © 2012 by John Wiley & Sons, Inc. Wiley-Blackwell is an imprint of John Wiley & Sons, formed by the merger of Wiley’s global Scientific, Technical and Medical business with Blackwell Publishing. Registered office: John Wiley & Sons Inc., The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offices: 2121 State Avenue, Ames, Iowa 50014-8300, USA The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 9600 Garsington Road, Oxford, OX4 2DQ, UK For details of our global editorial offices, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell. Authorization to photocopy items for internal or personal use, or the internal or personal use of specific clients, is granted by Blackwell Publishing, provided that the base fee is paid directly to the Copyright Clearance Center, 222 Rosewood Drive, Danvers, MA 01923. For those organizations that have been granted a photocopy license by CCC, a separate system of payments has been arranged. The fee codes for users of the Transactional Reporting Service are ISBN-13: 978-0-8138-1768-2/2012. Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their respective owners. -
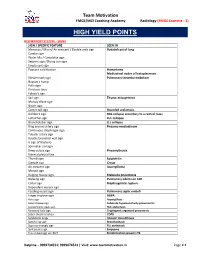
High Yield Points
Team Motivation FMGE/MCI Coaching Academy Radiology (FMGE Essentia - 3) HIGH YIELD POINTS RESPIRATORY SYSTEM – SIGNS SIGN / SPECIFIC FEATURE SEEN IN Meniscus / Moon/ Air crescent / Double arch sign Hydatid cyst of lung Cumbo sign Water lilly / Camalotte sign Serpent sign / Rising sun sign Empty cyst sign Popcorn calcification Hamartoma Mediastinal nodes of histoplasmosis Westermark sign Pulmonary thrombo-embolism Hapton’s hump Palla sign Fleishner lines Felson’s sign Sail sign Thymic enlargement Mulvay Wave sign Notch sign Comet tail sign Rounded atelectasis Golden S sign RUL collapse secondary to a central mass Luftsichel sign LUL collapse Broncholobar sign LLL collapse Ring around artery sign Pneumo-mediastinum Continuous diaphragm sign Tubular artery sign Double bronchial wall sign V sign of Naclerio Spinnaker sail sign Deep sulcus sign Pneumothorax Visceral pleural line Thumb sign Epiglottitis Steeple sign Croup Air crescent sign Aspergilloma Monod sign Bulging fissure sign Klebsiella pneumonia Batwing sign Pulmonary edema on CXR Collar sign Diaphragmatic rupture Dependant viscera sign Feeding vessel sign Pulmonary septic emboli Finger in glove sign ABPA Halo sign Aspergillosis Head cheese sign Subacute hypersensitivity pneumonitis Juxtaphrenic peak sign RUL atelectasis Reversed halo sign Cryptogenic organized pneumonia Saber sheath trachea COPD Sandstorm lungs Alveolar microlithiasis Signet ring sign Bronchiectasis Superior triangle sign RLL atelectasis Split pleura sign Empyema Tree in bud sign on HRCT Endobronchial spread in TB