Vascular Pathology in the Aged Human Brain
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
General Pathologic Anatomy
МІНІСТЕРСТВО ОХОРОНИ ЗДОРОВ'Я УКРАЇНИ Харківський національний медичний університет GENERAL PATHOLOGIC ANATOMY Manual for practical classes in pathomorphology for English-speaking teachers ЗАГАЛЬНА ПАТОЛОГІЧНА АНАТОМІЯ Методичні розробки до занять з патоморфології для англомовних викладачів медичних закладів Затверджено вченою радою ХНМУ. Протокол № 15 від 15.06.2017. Харків ХНМУ 2017 1 General pathologic anatomy : мanual for practical classes in patho- morphology for English-speaking teachers / comp. I. V. Sorokina, V. D. Markovskiy, I. V. Korneyko et al. – Kharkov : KNMU, 2017. – 64 p. Compilers I. V. Sorokina V. D. Markovskiy I. V. Korneyko G. I. Gubina-Vakulik V. V. Gargin O. N. Pliten M. S. Myroshnychenko S. N. Potapov T. V. Bocharova D. I. Galata O.V. Kaluzhina Загальна патологічна анатомія : метод. розроб. до занять з пато- морфології для англомовних викладачів мед. закладів / упоряд. І. В. Сорокіна, В. Д. Марковський, І. В. Корнейко та ін. – Харків : ХНМУ, 2017. – 64 с. Упорядники I. В. Сорокіна В. Д. Марковський І. В. Корнейко Г. І. Губіна-Вакулик В. В. Гаргін О. М. Плітень М. С. Мирошниченко С. М. Потапов Т. В. Бочарова Д. І. Галата О. В. Калужина 2 Foreword Pathomorphology, one of the most important medical subjects is aimed at teaching students understanding material basis and mechanisms of the development of main pathological processes and diseases. This manual published as separate booklets is devoted to general pathological processes as well as separate nosological forms. It is intended to the English-medium students of the medical and dentistry faculties. It can be used as additional material used for individual work in class. It can also be used to master the relevant terminology and its unified teaching. -
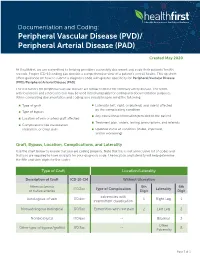
Documentationand Coding Tips: Peripheral Vascular Disease
Documentation and Coding: Peripheral Vascular Disease (PVD)/ Peripheral Arterial Disease (PAD) Created May 2020 At Healthfirst, we are committed to helping providers accurately document and code their patients’ health records. Proper ICD-10 coding can provide a comprehensive view of a patient’s overall health. This tip sheet offers guidance on how to submit a diagnosis code with greater specificity for Peripheral Vascular Disease (PVD)/Peripheral Arterial Disease (PAD). The risk factors for peripheral vascular disease are similar to those for coronary artery disease. The terms arteriosclerosis and atherosclerosis may be used interchangeably for coding and documentation purposes. When completing documentation and coding, you should keep in mind the following: Type of graft Laterality (left, right, or bilateral) and side(s) affected by the complicating condition Type of bypass Any educational information provided to the patient Location of vein or artery graft affected Treatment plan, orders, testing, prescriptions, and referrals Complications like claudication, ulceration, or chest pain Updated status of condition (stable, improved, and/or worsening) Graft, Bypass, Location, Complications, and Laterality Use the chart below to ensure that you are coding properly. Note that this is not an inclusive list of codes and that you are required to have six digits for your diagnosis code. The location and laterality will help determine the fifth and sixth digits for the codes. Type of Graft Location/Laterality Description of Graft ICD-10-CM Without -

Peripheral Artery Disease (Pad)
PERIPHERAL ARTERY DISEASE (PAD) Provider’s guide to diagnose and code PAD Peripheral Artery Disease (ICD-10 code I73.9) is estimated The American Cardiology and American Heart Association to affect 12 to 20% of Americans age 65 and older with as 2013 revised guidelines recommend the following many as 75% of that group being asymptomatic (Rogers et al, interpretation for noncompression values for ABI 2011). Of note, for the purposes of this clinical flyer the term (Anderson, 2013). peripheral vascular disease (PVD) is used synonymously with PAD. Table 2: Interpretation of ABI Values Who and how to screen for PAD Value Interpretation The updated 2013 American College of Cardiology and > 1.30 Non-compressible American Heart Association guidelines for the management of 1.00 – 1.29 Normal patients with PAD, recommends screening patients at risk for lower extremity PAD (Anderson et al, 2013). 0.91 – 0.99 Borderline The guidelines recommend reviewing vascular signs and 0.41 - 0.90 Mild to moderate PAD symptoms (e.g., walking impairment, claudication, ischemic 0.00 – 0.40 Severe PAD rest pain and/or presence of non-healing wounds) and physical examination (e.g., evaluation of pulses and inspection The diagnostic accuracy of the ABI can be hindered under the of lower extremities). The Trans-Atlantic Inter-Society following conditions: (Ruff, 2003) Consensus Document on Management of PAD and U.S. Preventative Task Force on screening for PAD identify similar › Patient anxiety and/or discomfort screening criteria that address patient’s age, smoking history, › Poor positioning of patient or restless patient co-morbid conditions and physical exam findings (Moyer, 2013 & Norgren et al, 2007). -

Pathogenetic Mechanisms in Vascular Dementia
lnt J Clin Lab Res 24: 15-22, 1994 Springer-Verlag 1994 Pathogenetie mechanisms in vascular dementia Lueilla Parnetti 1, Daniela Mari 2, Patrizia Mecocci 1, and Umberto Senin 1 1 Sezione di Gerontologia e Geriatria, Dipartimento di Medicina Clinica, Patologia e Farmacologia, Universitfi degli Studi di Perugia, Via Eugubina 42, 1-06122 Perugia, Italy 2 Istituto di Medicina Interna, UniversitY. degli Studi di Milano, Milan, Italy Summary. Vascular dementia accounts for approximately figures reach and surpass prevalence rates for DAT [62]. 20% of all cases of dementia and for about 50% in VD is the commonest cause of dementia in Japan, being subjects over 80 years. Thromboembolism with multiple responsible for up to 50% of all clinical cases and for cerebral infarcts was considered to be almost the only 54%-65% of all autopsy-confirmed dementias world- pathogenetic pathway of vascular dementia, with multi- wide [88]. While degenerative dementias are currently un- infarct dementia as its clinical manifestation. However, treatable, there is, in contrast, a definite potential for the there is a great heterogeneity of vascular dementia syn- prevention and treatment of cerebrovascular diseases. dromes and pathological subtypes, as documented by the The varied clinical presentations and the multiple number of pathogenetic mechanisms now known to un- causes of dementia syndrome make clinical diagnosis derlie the clinical picture. They include thromboem- quite difficult. In 1984, a Work Group on the Diagnosis bolism and extracerebral and cerebral factors. Among of Alzheimer's Disease established by the National Insti- the extracerebral factors are ischemic hypoxic dementia tute of Neurological and Communicative Disorders and (i.e., dementia due to hypoperfusion), vasculitis, hyper- Stroke and the Alzheimer's Disease and Related Disor- viscosity and abnormalities of hemostasis. -

Intracerebral Hemorrhage
Circulation Journal ORIGINAL ARTICLE Circ J 2019; 83: 441 – 446 doi: 10.1253/circj.CJ-18-0938 Stroke Safety of Anticoagulant Therapy Including Direct Oral Anticoagulants in Patients With Acute Spontaneous Intracerebral Hemorrhage Yuki Sakamoto, MD; Chikako Nito, MD, PhD; Yasuhiro Nishiyama, MD, PhD; Satoshi Suda, MD, PhD; Noriko Matsumoto, MD, PhD; Junya Aoki, MD, PhD; Takashi Shimoyama, MD, PhD; Takuya Kanamaru, MD, PhD; Kentaro Suzuki, MD; Takuya Nishimura, MD; Masahiro Mishina, MD, PhD; Kazumi Kimura, MD, PhD Background: Because the efficacy and safety of anticoagulant therapy in patients with acute intracerebral hemorrhage (ICH) are not fully known, present study aimed to elucidate the current status and the safety of anticoagulant therapy, mainly direct oral anticoagulants (DOACs), for acute ICH and anticoagulant-indicated patients. Methods and Results: From September 2014 through March 2017, consecutive patients with acute (<7 days from onset), sponta- neous ICH were retrospectively enrolled from a prospective registry. Whether to start anticoagulation was at the attending physicians’ discretion, and thromboembolic or hemorrhagic events during hospitalization were analyzed. A total of 236 patients (80 women [34%]; median age 69 [interquartile range 61–79] years; National Institutes of Health stroke scale score 7 [3–16]) were enrolled. Of them, 47 patients (20%) had an indication for anticoagulant therapy (33 had atrial fibrillation, 14 developed deep vein thrombosis), and 41 of 47 patients (87%) were actually treated with anticoagulant therapy (DOACs were used in 34 patients) after a median of 7 days from ICH onset. There was neither hematoma expansion nor excessive hemorrhagic complications during hospitalization after starting anticoagulant therapy. -

Intracranial Angioplasty & Stenting
Position Statement Intracranial Angioplasty & Stenting for Cerebral Atherosclerosis: A Position Statement of the American Society of Interventional and Therapeutic Neuroradiology, Society of Interventional Radiology, and the American Society of Neuroradiology Stroke is the third leading cause of death and the 20) with the definitive National Institutes of Health leading cause of adult disability in North America, (NIH) study demonstrating a first year ischemic Europe, and Asia (1, 2). Intracranial cerebral athero- stroke rate in the pertinent vascular territory of at sclerosis accounts for approximately 8–10% of all least 11% (17). ischemic strokes with a higher reported incidence in the Asian, African, and Hispanic descent populations (3–5). Risk factors include insulin-dependent diabe- Review of Studies tes mellitus, hypercholesterolemia, hypertension, and Surgical Revascularization—EC/IC Bypass Trial cigarette smoking (6–8). In the United States, it is (Extracranial to Intracranial): In 1985, the EC/IC By- estimated that 40,000–60,000 new strokes per year pass Study Group published the results of a trial that are due to intracranial cerebral atherosclerosis. attempted to prove benefit for a surgical approach to treating intracranial atherosclerotic stenoses or occlu- Intracranial Atherosclerosis sion (18). This extracranial to intracranial arterial bypass trial was a prospective, multicenter, interna- Etiology tional study involving 1377 patients and attempted to Four mechanisms for ischemic stroke secondary to show that patients with an intracranial atherosclerotic intracranial atherosclerosis have been proposed: (1) stenosis or occlusion could benefit by an EC/IC by- hypoperfusion; (2) thrombosis at the site of stenosis pass. This trial failed for all subgroups, and in partic- due to plaque rupture, intraplaque hemorrhage, or ular for those with middle cerebral artery stenosis. -

Origin of the Microangiopathic Changes in Diabetes
ORIGIN OF THE MICROANGIOPATHIC CHANGES IN DIABETES A. H. BARNETT Birmingham SUMMARY its glycosidally linked disaccharide units. Such alterations The mechanism of development of microangiopathy is lead to abnormal packing of the peptide chains producing incompletely understood, but relates to a number of excessive leakiness of the membrane. The exact mech ultrastructural, biochemical and haemostatic processes. anisms of thickening and leakiness of basement mem These include capillary basement membrane thickening, brane and their relevance to diabetic complications are not non-enzymatic glycosylation, possibly increased free rad entirely clear, but appear to involve several biochemical ical activity, increased flux through the polyol pathway mechanisms. and haemostatic abnormalities. The central feature Non-enzymatic Glycosylation appears to be hyperglycaemia, which is causally related to the above processes and culminates in tissue ischaemia. In the presence of persistent hyperglycaemia glucose This article will briefly describe these processes and will chemically attaches to proteins non-enzymatically to form discuss possible pathogenic interactions which may lead a stable product (keto amine or Amadori product) of which to the development of the pathological lesion. glycosylated haemoglobin is the best-known example. In long-lived tissue proteins such as collagen the ketoamine Microangiopathy is a specific disorder of the small blood then undergoes a series of reactions resulting in the vessels which causes much morbidity and mortality in dia development of advanced glycosylation end products betic patients. Diabetic retinopathy is the commonest (AGE) (Fig. 1).5 AGE are resistant to degradation and con cause of blindness in the working population of the United tinue to accumulate indefinitely on long-lived proteins. -
Anti-Thrombotics in Stroke When to Start and When to Stop
Anti-Thrombotics In Stroke when to start and when to stop Ania Busza MD PhD Assistant Professor of Neurology University of Rochester School of Medicine and Dentistry No Relevent Disclosures • Research funding from NIH/NICHD (K12 award) • Materials provided for research from MC10, Inc This person was He has afib but was Outlinedischarged 1 week discharged only on ago with a subdural. aspirin – when Should they be back My patient is should I restart his on aspirin? currently on warfarin anticoagulation ? but wants to get pregnant. Is that Common questions that arise post-Stroke safe? Why is everyone The report says talking about putting “likely amyloid TIA patients on angiopathy” – what BOTH aspirin and do I do about their plavix for a few antithrombotics? weeks? Outline ? • Physiology – types of clots and the logic behind the different choices for antithrombotic therapy • Timing: When should antithrombotics be started… – after an ischemic stroke? ? ? – after a hemorrhagic stroke? • Safety: What to consider in selecting antithrombotic therapy – in pregnancy – in patients with cerebral amyloid angiopathy ? • DAPT: When is duo-antiplatelet treatment indicated? Physiology of Clots thrombosis - an obstruction of blood flow due to a localized occlusive process within one more more blood vessels. Physiology of Clots RED THROMBI WHITE THROMBI RED THROMBI • Erythrocytes + Fibrin • tend to develop in low flow situations: – dilated cardiac atria / afib – regions of ventricular hypokinesia (ventricular aneurysms, low EF, or MI) – leg/pelvic veins -

The Increasing Impact of Cerebral Amyloid Angiopathy: Essential New
JNNP Online First, published on August 26, 2017 as 10.1136/jnnp-2016-314697 Cerebrovascular disease J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp-2016-314697 on 26 August 2017. Downloaded from REVIEW The increasing impact of cerebral amyloid angiopathy: essential new insights for clinical practice Gargi Banerjee,1 Roxana Carare,2 Charlotte Cordonnier,3 Steven M Greenberg,4 Julie A Schneider,5 Eric E Smith,6 Mark van Buchem,7 Jeroen van der Grond,7 Marcel M Verbeek,8,9 David J Werring1 For numbered affiliations see ABSTRact Furthermore, CAA gained new relevance with the end of article. Cerebral amyloid angiopathy (CAA) has never been advent of anti-Aβ immunotherapies for the treat- more relevant. The last 5 years have seen a rapid ment of Alzheimer’s disease (AD), as a sizeable Correspondence to increase in publications and research in the field, with proportion of those treated went on to develop Dr David J Werring, The National Hospital for Neurology and the development of new biomarkers for the disease, imaging features of CAA-related inflammation as 5 Neurosurgery, UCL Institute thanks to advances in MRI, amyloid positron emission an unintended consequence. This, together with of Neurology, Queen Square, tomography and cerebrospinal fluid biomarker analysis. advances in our understanding of the impact of London WC1N 3BG, UK; d. The inadvertent development of CAA-like pathology CAA on cognition, in the context of ICH, ageing werring@ ucl. ac. uk in patients treated with amyloid-beta immunotherapy and AD, has broadened the clinical spectrum Received 1 March 2017 for Alzheimer’s disease has highlighted the importance of disease to which the contribution of CAA is Revised 26 April 2017 of establishing how and why CAA develops; without recognised. -

Diagnostic and Therapeutic Approach of Carotid and Cerebrovascular Plaque on the Basis of Vessel Imaging
Review J Lipid Atheroscler 2017 June;6(1):15-21 https://doi.org/10.12997/jla.2017.6.1.15 JLA pISSN 2287-2892 • eISSN 2288-2561 Diagnostic and Therapeutic Approach of Carotid and Cerebrovascular Plaque on the Basis of Vessel Imaging Dong Hyun Lee, Jong-Ho Park Department of Stroke Neurology, Seonam University Myongji Hospital, Goyang-si, Korea Atherosclerosis, characterized by chronic systemic inflammation with plaque formation, is one of the major causes of cerebrovascular disease. Recent advances in imaging technologies can help further understand the overall process and biology of plaque formation and rupture. Thus, these imaging techniques could aid clinicians to make better decision for risk stratification, therapeutic planning, and prediction of future cerebrovascular event. Ultrasonography, magnetic resonance imaging, and positron emission tomography are the rapidly-evolving imaging modalities dealing with assessment of atherosclerotic plaque. By advances in imaging technology for evaluating plaque, we can characterize the vulnerability of plaque in-vivo, understand the composition and activity of plaque, assess therapeutic response to treatment, and ultimately predict the overall risk of future cerebrovascular episodes. In this review, we will introduce current understanding of various advanced imaging modalities and clinical application of these imaging technologies. (J Lipid Atheroscler 2017 June;6(1):15-21) Key Words: Atherosclerosis, Plaque, Imaging, Carotid artery disease, Cerebrovascular disease INTRODUCTION vascular episodes, and reliably monitor the therapeutic response to medication. Atherosclerosis is a chronic systemic inflammatory Recent advances in imaging technologies can help disease with an insidious process caused by multiple further understand the overall process in atherosclerosis pathological changes triggering lipoprotein dysregulation including molecular biology of plaque formation and and immunocyte activation within the arterial system.1 rupture. -

From Brain to Heart: Possible Role of Amyloid-Β in Ischemic Heart Disease and Ischemia-Reperfusion Injury
International Journal of Molecular Sciences Review From Brain to Heart: Possible Role of Amyloid-β in Ischemic Heart Disease and Ischemia-Reperfusion Injury Giulia Gagno 1, Federico Ferro 1, Alessandra Lucia Fluca 1, Milijana Janjusevic 1, Maddalena Rossi 1, Gianfranco Sinagra 1, Antonio Paolo Beltrami 2 , Rita Moretti 3 and Aneta Aleksova 1,* 1 Cardiothoracovascular Department, Azienda Sanitaria Universitaria Giuliano Isontina (ASUGI) and University of Trieste, 34100 Trieste, Italy; [email protected] (G.G.); ff[email protected] (F.F.); alessandrafl[email protected] (A.L.F.); [email protected] (M.J.); [email protected] (M.R.); [email protected] (G.S.) 2 Department of Medicine (DAME), University of Udine, 33100 Udine, Italy; [email protected] 3 Department of Internal Medicine and Neurology, Neurological Clinic, 34100 Trieste, Italy; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +39-340-550-7762 Received: 3 December 2020; Accepted: 14 December 2020; Published: 17 December 2020 Abstract: Ischemic heart disease (IHD) is among the leading causes of death in developed countries. Its pathological origin is traced back to coronary atherosclerosis, a lipid-driven immuno-inflammatory disease of the arteries that leads to multifocal plaque development. The primary clinical manifestation of IHD is acute myocardial infarction (AMI),) whose prognosis is ameliorated with optimal timing of revascularization. Paradoxically, myocardium re-perfusion can be detrimental because of ischemia-reperfusion injury (IRI), an oxidative-driven process that damages other organs. Amyloid-β (Aβ) plays a physiological role in the central nervous system (CNS). Alterations in its synthesis, concentration and clearance have been connected to several pathologies, such as Alzheimer’s disease (AD) and cerebral amyloid angiopathy (CAA). -

Search for Reliable Circulating Biomarkers to Predict Carotid Plaque Vulnerability
International Journal of Molecular Sciences Review Search for Reliable Circulating Biomarkers to Predict Carotid Plaque Vulnerability Núria Puig 1,2, Elena Jiménez-Xarrié 3,*, Pol Camps-Renom 3,* and Sonia Benitez 2,* 1 Department of Biochemistry and Molecular Biology, Faculty of Medicine, Building M, Autonomous University of Barcelona (UAB), 08193 Cerdanyola del Vallès, Barcelona, Spain; [email protected] 2 Cardiovascular Biochemistry, Biomedical Research Institute Sant Pau (IIB-Sant Pau), 08041 Barcelona, Spain 3 Stroke Unit, Department of Neurology, Hospital de la Santa Creu i Sant Pau (IIB-Sant Pau), 08041 Barcelona, Spain * Correspondence: [email protected] (E.J.-X.); [email protected] (P.C.-R.); [email protected] (S.B.); Tel.: +34-93-553-7595 (S.B.) Received: 2 October 2020; Accepted: 1 November 2020; Published: 3 November 2020 Abstract: Atherosclerosis is responsible for 20% of ischemic strokes, and the plaques from the internal carotid artery the most frequently involved. Lipoproteins play a key role in carotid atherosclerosis since lipid accumulation contributes to plaque progression and chronic inflammation, both factors leading to plaque vulnerability. Carotid revascularization to prevent future vascular events is reasonable in some patients with high-grade carotid stenosis. However, the degree of stenosis alone is not sufficient to decide upon the best clinical management in some situations. In this context, it is essential to further characterize plaque vulnerability, according to specific characteristics (lipid-rich core, fibrous cap thinning, intraplaque hemorrhage). Although these features can be partly detected by imaging techniques, identifying carotid plaque vulnerability is still challenging. Therefore, the study of circulating biomarkers could provide adjunctive criteria to predict the risk of atherothrombotic stroke.