Cerebral Atherosclerosis Contributes to Alzheimer's Dementia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Defining Functional Interactions During Biogenesis of Epithelial Junctions
ARTICLE Received 11 Dec 2015 | Accepted 13 Oct 2016 | Published 6 Dec 2016 | Updated 5 Jan 2017 DOI: 10.1038/ncomms13542 OPEN Defining functional interactions during biogenesis of epithelial junctions J.C. Erasmus1,*, S. Bruche1,*,w, L. Pizarro1,2,*, N. Maimari1,3,*, T. Poggioli1,w, C. Tomlinson4,J.Lees5, I. Zalivina1,w, A. Wheeler1,w, A. Alberts6, A. Russo2 & V.M.M. Braga1 In spite of extensive recent progress, a comprehensive understanding of how actin cytoskeleton remodelling supports stable junctions remains to be established. Here we design a platform that integrates actin functions with optimized phenotypic clustering and identify new cytoskeletal proteins, their functional hierarchy and pathways that modulate E-cadherin adhesion. Depletion of EEF1A, an actin bundling protein, increases E-cadherin levels at junctions without a corresponding reinforcement of cell–cell contacts. This unexpected result reflects a more dynamic and mobile junctional actin in EEF1A-depleted cells. A partner for EEF1A in cadherin contact maintenance is the formin DIAPH2, which interacts with EEF1A. In contrast, depletion of either the endocytic regulator TRIP10 or the Rho GTPase activator VAV2 reduces E-cadherin levels at junctions. TRIP10 binds to and requires VAV2 function for its junctional localization. Overall, we present new conceptual insights on junction stabilization, which integrate known and novel pathways with impact for epithelial morphogenesis, homeostasis and diseases. 1 National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. 2 Computing Department, Imperial College London, London SW7 2AZ, UK. 3 Bioengineering Department, Faculty of Engineering, Imperial College London, London SW7 2AZ, UK. 4 Department of Surgery & Cancer, Faculty of Medicine, Imperial College London, London SW7 2AZ, UK. -

Absence of NEFL in Patient-Specific Neurons in Early-Onset Charcot-Marie-Tooth Neuropathy Markus T
ARTICLE OPEN ACCESS Absence of NEFL in patient-specific neurons in early-onset Charcot-Marie-Tooth neuropathy Markus T. Sainio, MSc, Emil Ylikallio, MD, PhD, Laura M¨aenp¨a¨a, MSc, Jenni Lahtela, PhD, Pirkko Mattila, PhD, Correspondence Mari Auranen, MD, PhD, Johanna Palmio, MD, PhD, and Henna Tyynismaa, PhD Dr. Tyynismaa [email protected] Neurol Genet 2018;4:e244. doi:10.1212/NXG.0000000000000244 Abstract Objective We used patient-specific neuronal cultures to characterize the molecular genetic mechanism of recessive nonsense mutations in neurofilament light (NEFL) underlying early-onset Charcot- Marie-Tooth (CMT) disease. Methods Motor neurons were differentiated from induced pluripotent stem cells of a patient with early- onset CMT carrying a novel homozygous nonsense mutation in NEFL. Quantitative PCR, protein analytics, immunocytochemistry, electron microscopy, and single-cell transcriptomics were used to investigate patient and control neurons. Results We show that the recessive nonsense mutation causes a nearly total loss of NEFL messenger RNA (mRNA), leading to the complete absence of NEFL protein in patient’s cultured neurons. Yet the cultured neurons were able to differentiate and form neuronal networks and neuro- filaments. Single-neuron gene expression fingerprinting pinpointed NEFL as the most down- regulated gene in the patient neurons and provided data of intermediate filament transcript abundancy and dynamics in cultured neurons. Blocking of nonsense-mediated decay partially rescued the loss of NEFL mRNA. Conclusions The strict neuronal specificity of neurofilament has hindered the mechanistic studies of re- cessive NEFL nonsense mutations. Here, we show that such mutation leads to the absence of NEFL, causing childhood-onset neuropathy through a loss-of-function mechanism. -

Serum Albumin OS=Homo Sapiens
Protein Name Cluster of Glial fibrillary acidic protein OS=Homo sapiens GN=GFAP PE=1 SV=1 (P14136) Serum albumin OS=Homo sapiens GN=ALB PE=1 SV=2 Cluster of Isoform 3 of Plectin OS=Homo sapiens GN=PLEC (Q15149-3) Cluster of Hemoglobin subunit beta OS=Homo sapiens GN=HBB PE=1 SV=2 (P68871) Vimentin OS=Homo sapiens GN=VIM PE=1 SV=4 Cluster of Tubulin beta-3 chain OS=Homo sapiens GN=TUBB3 PE=1 SV=2 (Q13509) Cluster of Actin, cytoplasmic 1 OS=Homo sapiens GN=ACTB PE=1 SV=1 (P60709) Cluster of Tubulin alpha-1B chain OS=Homo sapiens GN=TUBA1B PE=1 SV=1 (P68363) Cluster of Isoform 2 of Spectrin alpha chain, non-erythrocytic 1 OS=Homo sapiens GN=SPTAN1 (Q13813-2) Hemoglobin subunit alpha OS=Homo sapiens GN=HBA1 PE=1 SV=2 Cluster of Spectrin beta chain, non-erythrocytic 1 OS=Homo sapiens GN=SPTBN1 PE=1 SV=2 (Q01082) Cluster of Pyruvate kinase isozymes M1/M2 OS=Homo sapiens GN=PKM PE=1 SV=4 (P14618) Glyceraldehyde-3-phosphate dehydrogenase OS=Homo sapiens GN=GAPDH PE=1 SV=3 Clathrin heavy chain 1 OS=Homo sapiens GN=CLTC PE=1 SV=5 Filamin-A OS=Homo sapiens GN=FLNA PE=1 SV=4 Cytoplasmic dynein 1 heavy chain 1 OS=Homo sapiens GN=DYNC1H1 PE=1 SV=5 Cluster of ATPase, Na+/K+ transporting, alpha 2 (+) polypeptide OS=Homo sapiens GN=ATP1A2 PE=3 SV=1 (B1AKY9) Fibrinogen beta chain OS=Homo sapiens GN=FGB PE=1 SV=2 Fibrinogen alpha chain OS=Homo sapiens GN=FGA PE=1 SV=2 Dihydropyrimidinase-related protein 2 OS=Homo sapiens GN=DPYSL2 PE=1 SV=1 Cluster of Alpha-actinin-1 OS=Homo sapiens GN=ACTN1 PE=1 SV=2 (P12814) 60 kDa heat shock protein, mitochondrial OS=Homo -

Pathogenetic Mechanisms in Vascular Dementia
lnt J Clin Lab Res 24: 15-22, 1994 Springer-Verlag 1994 Pathogenetie mechanisms in vascular dementia Lueilla Parnetti 1, Daniela Mari 2, Patrizia Mecocci 1, and Umberto Senin 1 1 Sezione di Gerontologia e Geriatria, Dipartimento di Medicina Clinica, Patologia e Farmacologia, Universitfi degli Studi di Perugia, Via Eugubina 42, 1-06122 Perugia, Italy 2 Istituto di Medicina Interna, UniversitY. degli Studi di Milano, Milan, Italy Summary. Vascular dementia accounts for approximately figures reach and surpass prevalence rates for DAT [62]. 20% of all cases of dementia and for about 50% in VD is the commonest cause of dementia in Japan, being subjects over 80 years. Thromboembolism with multiple responsible for up to 50% of all clinical cases and for cerebral infarcts was considered to be almost the only 54%-65% of all autopsy-confirmed dementias world- pathogenetic pathway of vascular dementia, with multi- wide [88]. While degenerative dementias are currently un- infarct dementia as its clinical manifestation. However, treatable, there is, in contrast, a definite potential for the there is a great heterogeneity of vascular dementia syn- prevention and treatment of cerebrovascular diseases. dromes and pathological subtypes, as documented by the The varied clinical presentations and the multiple number of pathogenetic mechanisms now known to un- causes of dementia syndrome make clinical diagnosis derlie the clinical picture. They include thromboem- quite difficult. In 1984, a Work Group on the Diagnosis bolism and extracerebral and cerebral factors. Among of Alzheimer's Disease established by the National Insti- the extracerebral factors are ischemic hypoxic dementia tute of Neurological and Communicative Disorders and (i.e., dementia due to hypoperfusion), vasculitis, hyper- Stroke and the Alzheimer's Disease and Related Disor- viscosity and abnormalities of hemostasis. -

Spatial Distribution of Leading Pacemaker Sites in the Normal, Intact Rat Sinoa
Supplementary Material Supplementary Figure 1: Spatial distribution of leading pacemaker sites in the normal, intact rat sinoatrial 5 nodes (SAN) plotted along a normalized y-axis between the superior vena cava (SVC) and inferior vena 6 cava (IVC) and a scaled x-axis in millimeters (n = 8). Colors correspond to treatment condition (black: 7 baseline, blue: 100 µM Acetylcholine (ACh), red: 500 nM Isoproterenol (ISO)). 1 Supplementary Figure 2: Spatial distribution of leading pacemaker sites before and after surgical 3 separation of the rat SAN (n = 5). Top: Intact SAN preparations with leading pacemaker sites plotted during 4 baseline conditions. Bottom: Surgically cut SAN preparations with leading pacemaker sites plotted during 5 baseline conditions (black) and exposure to pharmacological stimulation (blue: 100 µM ACh, red: 500 nM 6 ISO). 2 a &DUGLDFIoQChDQQHOV .FQM FOXVWHU &DFQDG &DFQDK *MD &DFQJ .FQLS .FQG .FQK .FQM &DFQDF &DFQE .FQM í $WSD .FQD .FQM í .FQN &DVT 5\U .FQM &DFQJ &DFQDG ,WSU 6FQD &DFQDG .FQQ &DFQDJ &DFQDG .FQD .FQT 6FQD 3OQ 6FQD +FQ *MD ,WSU 6FQE +FQ *MG .FQN .FQQ .FQN .FQD .FQE .FQQ +FQ &DFQDD &DFQE &DOP .FQM .FQD .FQN .FQG .FQN &DOP 6FQD .FQD 6FQE 6FQD 6FQD ,WSU +FQ 6FQD 5\U 6FQD 6FQE 6FQD .FQQ .FQH 6FQD &DFQE 6FQE .FQM FOXVWHU V6$1 L6$1 5$ /$ 3 b &DUGLDFReFHSWRUV $GUDF FOXVWHU $GUDD &DY &KUQE &KUP &KJD 0\O 3GHG &KUQD $GUE $GUDG &KUQE 5JV í 9LS $GUDE 7SP í 5JV 7QQF 3GHE 0\K $GUE *QDL $QN $GUDD $QN $QN &KUP $GUDE $NDS $WSE 5DPS &KUP 0\O &KUQD 6UF &KUQH $GUE &KUQD FOXVWHU V6$1 L6$1 5$ /$ 4 c 1HXURQDOPURWHLQV -

Supplemental Text and Figures
Supplemental Materials and Methods Experimental bone metastasis assay Primary PCa cells were sorted by GFP marker from mTmG+ tumors, and 105 cells in 20μL PBS were injected using Hamilton syringe into the tibia of 6-week old NSG mice. Mice were monitored biweekly for moribund signs for euthanasia and organ harvest. Noninvasive mouse and ex vivo imaging MRI imaging with Bruker ICON and fluorescence imaging of fresh organs with metastasis enumeration were recently described (Lu et al. 2017). Primary prostate cell sphere formation assay Isolate of primary cells from prostate, culture and counting of prostatospheres on Matrigel were performed as described (Lukacs et al. 2010). For organoid culture assay, we followed a published matrigel embedding method (Chua et al. 2014). RNA-Seq and differential gene expression Total RNA was isolated from prostate tumors using Direct-zol RNA MiniPrep Kit (Zymo Research) and processed for stranded total RNA-Seq using Illumina HiSeq 4000 at Sequencing and Microarray Facility at MD Anderson Cancer Center. The differential expression analysis was performed using the DESeq2 package of R. P-values obtained after multiple binomial tests were adjusted using BH method. Significant genes are defined by using a cut-off of 0.05 on the BH corrected p-value and an absolute log2 fold change value of at least 1.5. Histology and western blot H&E stain, immunohistochemical (IHC) and western blot were performed as previously described (Ding et al. 2011; Wang et al. 2016). Primary antibodies for IHC include Ki67 (Fisher, RM-9106-S1), cleaved caspase 3 (Cell Signaling Technology aka CST, 9661), cyclin D1 (Fisher, clone SP4), TGFBR2 (Abcam, ab61213), BMPR2 (Abcam, ab130206), AR (EMD Millipore, 06-680), phospho- Akt (CST, 4060), GFP (CST, 2956), E-Cadherin (CST, 14472). -

Intracranial Angioplasty & Stenting
Position Statement Intracranial Angioplasty & Stenting for Cerebral Atherosclerosis: A Position Statement of the American Society of Interventional and Therapeutic Neuroradiology, Society of Interventional Radiology, and the American Society of Neuroradiology Stroke is the third leading cause of death and the 20) with the definitive National Institutes of Health leading cause of adult disability in North America, (NIH) study demonstrating a first year ischemic Europe, and Asia (1, 2). Intracranial cerebral athero- stroke rate in the pertinent vascular territory of at sclerosis accounts for approximately 8–10% of all least 11% (17). ischemic strokes with a higher reported incidence in the Asian, African, and Hispanic descent populations (3–5). Risk factors include insulin-dependent diabe- Review of Studies tes mellitus, hypercholesterolemia, hypertension, and Surgical Revascularization—EC/IC Bypass Trial cigarette smoking (6–8). In the United States, it is (Extracranial to Intracranial): In 1985, the EC/IC By- estimated that 40,000–60,000 new strokes per year pass Study Group published the results of a trial that are due to intracranial cerebral atherosclerosis. attempted to prove benefit for a surgical approach to treating intracranial atherosclerotic stenoses or occlu- Intracranial Atherosclerosis sion (18). This extracranial to intracranial arterial bypass trial was a prospective, multicenter, interna- Etiology tional study involving 1377 patients and attempted to Four mechanisms for ischemic stroke secondary to show that patients with an intracranial atherosclerotic intracranial atherosclerosis have been proposed: (1) stenosis or occlusion could benefit by an EC/IC by- hypoperfusion; (2) thrombosis at the site of stenosis pass. This trial failed for all subgroups, and in partic- due to plaque rupture, intraplaque hemorrhage, or ular for those with middle cerebral artery stenosis. -

Homer1 Promotes Dendritic Spine Growth Through Ankyrin-G and Its Loss Reshapes the Synaptic Proteome
Molecular Psychiatry (2021) 26:1775–1789 https://doi.org/10.1038/s41380-020-00991-1 ARTICLE Homer1 promotes dendritic spine growth through ankyrin-G and its loss reshapes the synaptic proteome 1 1 2 1,5 2 Sehyoun Yoon ● Nicolas H. Piguel ● Natalia Khalatyan ● Leonardo E. Dionisio ● Jeffrey N. Savas ● Peter Penzes 1,3,4 Received: 22 February 2020 / Revised: 24 November 2020 / Accepted: 7 December 2020 / Published online: 4 January 2021 © The Author(s), under exclusive licence to Springer Nature Limited part of Springer Nature 2021. This article is published with open access Abstract Homer1 is a synaptic scaffold protein that regulates glutamatergic synapses and spine morphogenesis. HOMER1 knockout (KO) mice show behavioral abnormalities related to psychiatric disorders, and HOMER1 has been associated with psychiatric disorders such as addiction, autism disorder (ASD), schizophrenia (SZ), and depression. However, the mechanisms by which it promotes spine stability and its global function in maintaining the synaptic proteome has not yet been fully investigated. Here, we used computational approaches to identify global functions for proteins containing the Homer1-interacting PPXXF motif within the postsynaptic compartment. Ankyrin-G was one of the most topologically important nodes in the postsynaptic peripheral 1234567890();,: 1234567890();,: membrane subnetwork, and we show that one of the PPXXF motifs, present in the postsynaptically-enriched 190 kDa isoform of ankyrin-G (ankyrin-G 190), is recognized by the EVH1 domain of Homer1. We use proximity ligation combined with super- resolution microscopy to map the interaction of ankyrin-G and Homer1 to distinct nanodomains within the spine head and correlate them with spine head size. -

Neurofilament Medium Polypeptide (NFM) Protein Concentration Is
Neurofilament medium polypeptide (NFM) protein concentration is increased in CSF and serum samples from patients with brain injury MARTÍNEZ-MORILLO, Eduardo, CHILDS, Charmaine <http://orcid.org/0000- 0002-1558-5633>, GARCÍA, Belén Prieto, ÁLVAREZ MENÉNDEZ, Francisco V., ROMASCHIN, Alexander D., CERVELLIN, Gianfranco, LIPPI, Giuseppe and DIAMANDIS, Eleftherios P. Available from Sheffield Hallam University Research Archive (SHURA) at: http://shura.shu.ac.uk/9484/ This document is the author deposited version. You are advised to consult the publisher's version if you wish to cite from it. Published version MARTÍNEZ-MORILLO, Eduardo, CHILDS, Charmaine, GARCÍA, Belén Prieto, ÁLVAREZ MENÉNDEZ, Francisco V., ROMASCHIN, Alexander D., CERVELLIN, Gianfranco, LIPPI, Giuseppe and DIAMANDIS, Eleftherios P. (2015). Neurofilament medium polypeptide (NFM) protein concentration is increased in CSF and serum samples from patients with brain injury. Clinical Chemistry and Laboratory Medicine, 53 (10), 1575-1584. Copyright and re-use policy See http://shura.shu.ac.uk/information.html Sheffield Hallam University Research Archive http://shura.shu.ac.uk Clin Chem Lab Med 2015; aop Eduardo Mart í nez-Morillo , Charmaine Childs , Bel é n Prieto Garc í a , Francisco V. Á lvarez Men é ndez , Alexander D. Romaschin , Gianfranco Cervellin , Giuseppe Lippi and Eleftherios P. Diamandis * Neurofilament medium polypeptide (NFM) protein concentration is increased in CSF and serum samples from patients with brain injury DOI 10.1515/cclm-2014-0908 Methods: An ELISA from Elabscience was used. The selec- Received September 14 , 2014 ; accepted January 6 , 2015 tivity was evaluated using size-exclusion chromatography and mass spectrometry. Intra- and inter-batch coefficients of variation (CV) were also studied. -
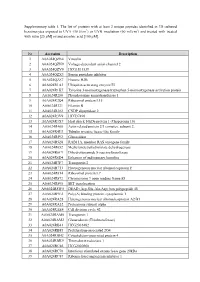
Supplementary Table 1. the List of Proteins with at Least 2 Unique
Supplementary table 1. The list of proteins with at least 2 unique peptides identified in 3D cultured keratinocytes exposed to UVA (30 J/cm2) or UVB irradiation (60 mJ/cm2) and treated with treated with rutin [25 µM] or/and ascorbic acid [100 µM]. Nr Accession Description 1 A0A024QZN4 Vinculin 2 A0A024QZN9 Voltage-dependent anion channel 2 3 A0A024QZV0 HCG1811539 4 A0A024QZX3 Serpin peptidase inhibitor 5 A0A024QZZ7 Histone H2B 6 A0A024R1A3 Ubiquitin-activating enzyme E1 7 A0A024R1K7 Tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein 8 A0A024R280 Phosphoserine aminotransferase 1 9 A0A024R2Q4 Ribosomal protein L15 10 A0A024R321 Filamin B 11 A0A024R382 CNDP dipeptidase 2 12 A0A024R3V9 HCG37498 13 A0A024R3X7 Heat shock 10kDa protein 1 (Chaperonin 10) 14 A0A024R408 Actin related protein 2/3 complex, subunit 2, 15 A0A024R4U3 Tubulin tyrosine ligase-like family 16 A0A024R592 Glucosidase 17 A0A024R5Z8 RAB11A, member RAS oncogene family 18 A0A024R652 Methylenetetrahydrofolate dehydrogenase 19 A0A024R6C9 Dihydrolipoamide S-succinyltransferase 20 A0A024R6D4 Enhancer of rudimentary homolog 21 A0A024R7F7 Transportin 2 22 A0A024R7T3 Heterogeneous nuclear ribonucleoprotein F 23 A0A024R814 Ribosomal protein L7 24 A0A024R872 Chromosome 9 open reading frame 88 25 A0A024R895 SET translocation 26 A0A024R8W0 DEAD (Asp-Glu-Ala-Asp) box polypeptide 48 27 A0A024R9E2 Poly(A) binding protein, cytoplasmic 1 28 A0A024RA28 Heterogeneous nuclear ribonucleoprotein A2/B1 29 A0A024RA52 Proteasome subunit alpha 30 A0A024RAE4 Cell division cycle 42 31 -

New Partners Identified by Mass Spectrometry Assay Reveal Functions of NCAM2 in Neural Cytoskeleton Organization
International Journal of Molecular Sciences Article New Partners Identified by Mass Spectrometry Assay Reveal Functions of NCAM2 in Neural Cytoskeleton Organization Antoni Parcerisas 1,2,3,*,† , Alba Ortega-Gascó 1,2,† , Marc Hernaiz-Llorens 1,2 , Maria Antonia Odena 4, Fausto Ulloa 1,2, Eliandre de Oliveira 4, Miquel Bosch 3 , Lluís Pujadas 1,2 and Eduardo Soriano 1,2,* 1 Department of Cell Biology, Physiology and Immunology, University of Barcelona and Institute of Neurosciences, 08028 Barcelona, Spain; [email protected] (A.O.-G.); [email protected] (M.H.-L.); [email protected] (F.U.); [email protected] (L.P.) 2 Centro de Investigación Biomédica en Red sobre Enfermedades Neurodegenerativas (CIBERNED), 28031 Madrid, Spain 3 Department of Basic Sciences, Universitat Internacional de Catalunya, 08195 Sant Cugat del Vallès, Spain; [email protected] 4 Plataforma de Proteòmica, Parc Científic de Barcelona (PCB), 08028 Barcelona, Spain; [email protected] (M.A.O.); [email protected] (E.d.O.) * Correspondence: [email protected] (A.P.); [email protected] (E.S.) † A.P. and A.O.-G. contributed equally. Abstract: Neuronal cell adhesion molecule 2 (NCAM2) is a membrane protein with an important role in the morphological development of neurons. In the cortex and the hippocampus, NCAM2 is essential for proper neuronal differentiation, dendritic and axonal outgrowth and synapse forma- tion. However, little is known about NCAM2 functional mechanisms and its interactive partners Citation: Parcerisas, A.; during brain development. Here we used mass spectrometry to study the molecular interactome Ortega-Gascó, A.; Hernaiz-Llorens, of NCAM2 in the second postnatal week of the mouse cerebral cortex. -

Diagnostic and Therapeutic Approach of Carotid and Cerebrovascular Plaque on the Basis of Vessel Imaging
Review J Lipid Atheroscler 2017 June;6(1):15-21 https://doi.org/10.12997/jla.2017.6.1.15 JLA pISSN 2287-2892 • eISSN 2288-2561 Diagnostic and Therapeutic Approach of Carotid and Cerebrovascular Plaque on the Basis of Vessel Imaging Dong Hyun Lee, Jong-Ho Park Department of Stroke Neurology, Seonam University Myongji Hospital, Goyang-si, Korea Atherosclerosis, characterized by chronic systemic inflammation with plaque formation, is one of the major causes of cerebrovascular disease. Recent advances in imaging technologies can help further understand the overall process and biology of plaque formation and rupture. Thus, these imaging techniques could aid clinicians to make better decision for risk stratification, therapeutic planning, and prediction of future cerebrovascular event. Ultrasonography, magnetic resonance imaging, and positron emission tomography are the rapidly-evolving imaging modalities dealing with assessment of atherosclerotic plaque. By advances in imaging technology for evaluating plaque, we can characterize the vulnerability of plaque in-vivo, understand the composition and activity of plaque, assess therapeutic response to treatment, and ultimately predict the overall risk of future cerebrovascular episodes. In this review, we will introduce current understanding of various advanced imaging modalities and clinical application of these imaging technologies. (J Lipid Atheroscler 2017 June;6(1):15-21) Key Words: Atherosclerosis, Plaque, Imaging, Carotid artery disease, Cerebrovascular disease INTRODUCTION vascular episodes, and reliably monitor the therapeutic response to medication. Atherosclerosis is a chronic systemic inflammatory Recent advances in imaging technologies can help disease with an insidious process caused by multiple further understand the overall process in atherosclerosis pathological changes triggering lipoprotein dysregulation including molecular biology of plaque formation and and immunocyte activation within the arterial system.1 rupture.