Post-Covid-19 Practice Recovery Toolkit
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Torrance Herald
I DOUBLE-RING NUPTIALS Donna Brimer Becomes 3ride of Wilmington Man Tall tapers cast a soft glow upon the altar of First Meth odist Church last. Saturday when Rev- Clarence E. Miller of ficiated at the nuptials o£ Donna Lou Brimer and Albert E. Whelchel. Preceding the'lovely bride, daughter of Mr. and Mrs. D. F. Brimer of 427 W. Ocean St., to* he altar were her sister, Mrs. 'illiam Leo, to serve as b o G. L. Dlsmuke (Joanne Brimer), an. Michael Fiosol, a cousin of matron of honor, and brides 10 bride, carried tho double maids Barbara Fiesol, cousin of ngs. Ushers were Wick t tho bride, and Betty Whelchel, ch, Robert Burnotlc, Frank Tut- lister of the groom. Margie Lou e and Raymond Hurt., Lilos, a cousin of the bride, was Fay Sims and Carol Branca, flower girl. assmates of the bride, lit the The wedding gown was fash- 3. Baskets of white stock iOaod of white satin with a nd gladioli were placed by the stand-up collar and long pointed Itar. sleeves edged In seed pearls. Miss Brimer wore a veil of Mrs. Brimer was attired In a French Illusion edged in. tatting oor-length dress of royal blui and carried a white prayer book 'ith pink accessories for the cc with a white orchid and stream oniony, while tho bridegroom's ers of satin lother wore a gown of ri entwined with Ce 'ith white accessories). cil Bruncr roses. Following a" reception at i Each member of the bridal en /. Ocean St., the now Mr. -

For Flavor at Its Crisp, Fresh Best
THE EVENING STAR gation to Russia on cultural B-12 Wellington, 0. C., Thunder, September 17, 1959 exchange, with Mrs. John- Our Annual ston. in sequined apricot lace, TOOTH STAINS READERS CLEARING HOUSE - and Mr. Donald David, phair- tosacco corni man of the Ford Foundation. KING-SIZI Door Q33 •» rstommnndscA L. M In addition to Ambassador Want* to Cloan Shower Groores WEE WOMEN by dentists l« remove \*/ dalas * a— Ci_: n 1.1. BIDDING Few Sly Remarks Menshikov, the other Rus- Mn. M. O. H: Annandale living ifwvw ivwin* vivin*i*w iPvifi Lk*L kfiiskl X-.| ~. J._X..I ' slang present were Messrs. V. Over a year ago we had glass sliding shower doors in- ivwa vriyni, iwwi wwrvuwnvi. over Soap water run down doors P. Yelutin, A. Zhukov, stalled the bathtub. and the O. V. grooves or that the doors operate on. and K4pZ£Z49U79t Passed at Dinner Yemelyanov, Tikho- into the slot SALE 8. N. A. although there are openings for this water to run out into the It iVete In Praymi Contianed Fran Pace B-7 lon in a short red silk dinner nov. A. M. Markov. A. A. Sol- tub, a part of it stays at the bottom of the groove to form a wife, who was in a long green dress. datov, O. T. Bhulski, V. 8. black scum. THE gown with matching chiffon AMERICAN AMBASSA- Lebedev, O. A. Troyanovskl, \ I have found that a sponge although absorbent, is too to get into thk tiny stole: Secretary of Commerce DOR TO THE USSR and Mrs. -

The Nobby Shop
Fashion Article S THE PRAYER CORNER Jor Economical Transportation kly A BEGINNING AND AN ENDING BY LUCILE BUCHANAN Well, otio year has flown into 11- of Bazar other. The bi-ginningof « War Fashion Editor Harper'* lias come," ¦ I But are not those divisions of . matters . 'more' New York, January 2; Paris back, and a swathed hip-line. The time purely arbitrary in feature of this frock are of clocks, chronometers ami sun 6 talks about greater feminity outstanding dials? "Time," Aristotle tells us, "is } Thi clothes, and then makes evening two flat and stiff tailored bows, one of successive M that »re decidedly tailored, at the left hip and the other at the! the perceived number been gowns is the the left shoulder. With this costume movements,"- and this century i liaa cnvefully ik This, of course, way of the .lust as '.Ik node contradicts itself, are worn a long chain of diamonds the product last, checked and vcco.i- >{¦ constantly new will e the successive is what makes the pursuit of with a diamond pendant, and many century .'lri<-. tiitione<ul where | N^hicli it is. The shoes are a movement to the present. the exciting business diamond bracelets, roll iiVt'o each other, hir. Hjnshion are, of course, many flut- darker shade of pinky-beige edged the years for necessary ^frhereand floating and even bouf- with silver lame, and fastened with divisions of time are useful . and each month ^^HpngHnic tulle gowns worn this winter, in small diamond clasps, at the top of practical purposes, j to the little chiffon k-ag that the instep, where the sandal strap, is, in a real sense, both a beginning WW^nlrast for . -
![The Costumer's Q]!Arterly](https://docslib.b-cdn.net/cover/0965/the-costumers-q-arterly-730965.webp)
The Costumer's Q]!Arterly
The costumer's Q]!arterly Vol. 11, No. 1 ]an/Feb/ Mar 1998 In This Issue How to Build A 1790's Gown Bridal Gowns of the 1920's cutting a 1913 Noifolk Ensemble A Military Man our Fashionable Mothers ustng La Mode Bagatelle Patterns GBACG Requests the Pleasure of Your comyany caring for Teitiles A Familj Affair Good night, sweet prince, And flights of angels sing thee to thy rest! Costumer's Quarterly Jan/Feb/Mar 1998 In Loving Remembrance Gary Lin Anderson 1943- 1998 At 3:00pm yesterday my father, Gary Lin Anderson They say that when a king dies, a comet streaks the skies passed from this world. He went peacefully, without to announce it to the world. What is a more fitting trib struggle as his body slowed down and then came to a ute to the passing of a techno wizard, than the satellite stop. I am reassured by many members of my family that currently tumbles in our sky? that he was never in any pain, nor did he have his per ception of the world dimmed by any drugs. He left this This was the conclusion of a valiant nine-month battle world as he lived his life, gently and patiently. He died with the deadly, rare form of brain cancer, glioblastoma in his home surrounded by his friends, family, his books multiforma. He beat all the odds by staying with us as and memories as he had wished. The paramedics long as he did, giving both family and friends a chance attempted to resuscitated him, but it was his will to go at to say good-bye. -

SUNDAY Elusive Images Photo Contest
Lady Eagles REMINISCE beat Comets SUNDAY Elusive Images photo contest ..........Page A-8 Jan. 27, 2008 ...................................Page A-3 INSIDE Mendocino County’s World briefly The Ukiah local newspaper .......Page A-2 Monday: Cloudy with rain; H 46º L 33º Tuesday: Cloudy and cold; H 42º L 34º $1 tax included DAILY JOURNAL ukiahdailyjournal.com 42 pages, Volume 149 Number 293 email: [email protected] Ukiah’s Melissa Chaty reaches final 8 Storm lull won’t MISS AMERICA PAGEANT last long New system expected to bring several days of rain The Daily Journal Ukiahans got a brief respite Saturday from the storms that lashed the county all week, but another system was expected to move into the county Saturday night, bring- ing more rain. The Miss America Pageant According to reports from the National was at the Planet Holly- Weather Service, an area of low pressure off wood Resort & Casino on the Mendocino Coast was expected to send the Las Vegas Strip. rain east across the county Saturday evening. The rain is expected to continue into Monday when cold temperatures are predict- Competing ed to drop the snow level to 1,500 feet. Rain is expected until at least Wednesday. Heavy rainfall overnight Friday con- for Miss tributed to several slides that briefly covered parts of Highway 253 and Highway 128. According to the NWS, more than three America: inches of rain fell in the county Friday night. On Saturday morning, the NWS issued a flood alert for the Navarro River. the week As of 7:15 a.m. Saturday, the river was at 17.3 feet, according to the NWS. -

Sized Women's Fashions, 1910-1924 Carmen Nicole Keist Iowa State University
Iowa State University Capstones, Theses and Graduate Theses and Dissertations Dissertations 2012 "The new costumes of odd sizes:" Plus sized women's fashions, 1910-1924 Carmen Nicole Keist Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/etd Part of the Art and Materials Conservation Commons, Fashion Design Commons, History Commons, and the Home Economics Commons Recommended Citation Keist, Carmen Nicole, ""The new costumes of odd sizes:" Plus sized women's fashions, 1910-1924" (2012). Graduate Theses and Dissertations. 12363. https://lib.dr.iastate.edu/etd/12363 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. “The new costumes of odd sizes:” Plus sized women’s fashions, 1910-1929 by Carmen Nicole Keist A dissertation submitted to the graduate faculty in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY Major: Apparel, Merchandising, and Design Program of Study Committee: Sara. B. Marcketti, Major Professor Amy S. Bix Mary Lynn Damhorst Charles M. Dobbs Linda S. Niehm Iowa State University Ames, Iowa 2012 Copyright © Carmen Nicole Keist, 2012. All rights reserved. ii TABLE OF CONTENTS LIST OF TABLES iv LIST OF FIGURES v ACKNOWLEDGEMENTS vi CHAPTER -

WESTFIELD LEADER I
WESTFIELD LEADER r«£ LEADING AND MOST WIDELY CIRCULATED WEEKLY NEWSP, PER IN UNION COUNTY Published SIXTY-SECOND YEAR—No. 17 WESTFIELD, NEW JERSEY, JANUARY 3, 1952 Every Thursday M Page*—* Silver Star Talk on Government 1952 March Of Dimes To Feature Meeting Awarded Pvt. Mayor Appoints Two New Sidney C. Moody of Plainfield, •riue Opens In County generall manager of Calcl o CChemh i John Brooks cal Division of the American Cya-'Uy l DlOOfl UOHOrS namid Co., Round Brook, willl add- I The 1952 March of Dimes dress the Westfield Women's Re- Councilmanic Committees pened In Union County yester-r Cite Westfielder publican Club Tuesday afternoon Local Red Cross jay with the avowed objective of at the home of Mrs. Harold C. iting the fight against polio on, For Gallantry Towttley of 1011 Harding street Quota 500 Pints "pay as you go basis" after four In Korean Action on "Government and Taxes on In Seven Months Names George Civil Defense, fcuccessive years in which the Na- Business." A business meeting at tional; Foundation for Infantile Pvt. John Brooks, 509 Central 1:30 p.m. -will precede his talk Preparations are being made by iralysis has gone .into debt fight- scheduled for 3 p.m. Cox Honorary Parking, Traffic ing the only epidemic disease still avenue, has been awarded the Sil- the Westfield >- Mountainside Red * «i m pn the increase in America. ver Star, the nation's third highest Mr. Moody, vice president of the Cross chapter for the recruitment 11 .lhraPV I 1 combat decoration, for gallantry in American Cyanamid Co., is state 4 "During the last four years," of blood donors for the mobile unit *•"•*» "* J * Groups Named Edward L. -

The Complete Costume Dictionary
The Complete Costume Dictionary Elizabeth J. Lewandowski The Scarecrow Press, Inc. Lanham • Toronto • Plymouth, UK 2011 Published by Scarecrow Press, Inc. A wholly owned subsidiary of The Rowman & Littlefield Publishing Group, Inc. 4501 Forbes Boulevard, Suite 200, Lanham, Maryland 20706 http://www.scarecrowpress.com Estover Road, Plymouth PL6 7PY, United Kingdom Copyright © 2011 by Elizabeth J. Lewandowski Unless otherwise noted, all illustrations created by Elizabeth and Dan Lewandowski. All rights reserved. No part of this book may be reproduced in any form or by any electronic or mechanical means, including information storage and retrieval systems, without written permission from the publisher, except by a reviewer who may quote passages in a review. British Library Cataloguing in Publication Information Available Library of Congress Cataloging-in-Publication Data Lewandowski, Elizabeth J., 1960– The complete costume dictionary / Elizabeth J. Lewandowski ; illustrations by Dan Lewandowski. p. cm. Includes bibliographical references. ISBN 978-0-8108-4004-1 (cloth : alk. paper) — ISBN 978-0-8108-7785-6 (ebook) 1. Clothing and dress—Dictionaries. I. Title. GT507.L49 2011 391.003—dc22 2010051944 ϱ ™ The paper used in this publication meets the minimum requirements of American National Standard for Information Sciences—Permanence of Paper for Printed Library Materials, ANSI/NISO Z39.48-1992. Printed in the United States of America For Dan. Without him, I would be a lesser person. It is the fate of those who toil at the lower employments of life, to be rather driven by the fear of evil, than attracted by the prospect of good; to be exposed to censure, without hope of praise; to be disgraced by miscarriage or punished for neglect, where success would have been without applause and diligence without reward. -

December 10, 1943
HAPPY NEW YEAR Z 776 E tablished 1922 8 Madison College, Harrisonburg, Virginia, Friday, Deceinber 10, 1943 Vol. XX. No. 18 Bound Letters Announcement Stratford Presents "Brief Music" Are Presented BOARDING STUDENTS Every boarding student will With Harris And Suttle Directing To Professors receive a pink registration card when she checks in at the Dean Comedy Takes Seven Girls Through Bull Sessions, Volume Includes Letters of Women's office after the holi- Love Life Discussions, Bridge Games, And Suicide From Officials, College days. This card admits her to » Presidents, Educators classes for the Winter Quarter, The Stratford Dramatic club presents as its first performance of the beginning Tuesday, January 4, current season a sentimental comedy, Brief Music tonight at 8:00 p. m. In A large number of friends of Miss 1944, and should be shown to the Wilson Hall auditorium. i Elizabeth P. Cleveland and Dr. John the instructor in each class on The play is directed by Miss Ainslie Harris and Marie Suttle, Stratford W. Wayland sent them letters of con- Tuesday, January 4, and Wed- president, as her assistant. gratulation and appreciation on the nesday, January 5. Involves Seven Girls occasion of last Friday, when they Every boarding student re- Emmet Lauery's comedy which takes seven girls through bull sessions, were honored at the college. These turning on Tuesday, January 4, love life discussions, bridge games, and an attempt by one of the girls to letters were compiled in a book ap- and thereafter, must call at the commit suicide in three years of college life. -

Watertown Readers
Property of the'... « Watertown Historical Society watertownhistoricalsociety.org7 Property of the Watertown Historical Society watertownhistoricalsociety.org Property of the Watertown Historical Society watertownhistoricalsociety.org Stone Rededicated. At 2:30 o'clock Sunday alteafternoor n arah Whitman Trumbull chapter, .ughter of the American Revolu- tion rededicated the Rev. John Trumbull marker to the Old ceme-- tery on Main street with about 100 in attendance, including about 35 members of Sarah Whitman Trum- bull chapter and 25 members of the Sons of the Revolution. The mark- er has been recut which was made possible through the Sarah Whit man Trumbull chapter and the Sons of the Revolution. Rev. John Trumbull was th< first pastor of First Congregation- _ al church in Watertown which was •| located in the southwest corner of the Old cemetery. Mrs. Edgar G. Norton, regen • of the local chapter greeted those • in attendance and was in charge of the services as follows: In- vocation, Rev. Oscar L. Locke greetings from State President o: D. A. R. Miss Emeline Street of New Haven; greetings from State President S. A. R. Mr. Tomlin- son of Meriden; greetings from Mattatuck chapter, 3.. A. R. Judge Frederick Peasley of Cheshire; historical sketch by Ex-Regent of local chapter, Mrs. Eugene H —Photo by John Haley, Hartford Lamphier; dedicatory, Rev. Clar- MISS RUTH EVANS ence E. Wells; unveiling of mark- Daughter of Mr. and Mrs. Arthur G. Evans of Watertown, who er, Miss Alice Lamphier and Miss was graduated from the Rhode Island School of Design In Providence, Priscilla Atwood; benediction, Dr. B. I., recently. -

The Glengarry for GLENGARRIANS for GLENGARRIANS TETS FINEST WEEKLY NEWSPAPER in EASTERN ONTARIO
ALL THE NEWS ^ ALL THE NEWS OF GLENGARRY OF GLENGARRY The Glengarry FOR GLENGARRIANS FOR GLENGARRIANS TETS FINEST WEEKLY NEWSPAPER IN EASTERN ONTARIO Alexandria, On; Friday, June 14, 1946 $2.00 A YEA* VOL LIV—No. 24 Interesting Early Summer Weddings Was With Royal Liberals Must Prepare Now For Their Honor Servicemen At St. Telesphore VILLENEUVE—MACDONALD ( dress of light blue crepe with hand Party At Preview Return To Power, Oliver Declares A wedding of wide interest was embroidered trim and navy blue ac- quietly solemnized in the Chapel at cessories, Miss Theresa Thauvette, Col. D. C Cameron Lead Billfolds And Money the Bishop’s House, Alexandria Wed- sister of rhe groom, was maid of honor Provincial House Leader Critical Of Drew 1 Presented To Eleven nesday morning, June 12th, ’ at 8 and she chose a street length dress in Canadian Forces In Administration In Rousing; Speech At Repats At Welcoming o'clock, when Mrs. Florence G. Mac- ’pink tone and edged with lace. Her ac Victory Parade Glengarry Annual Opening East Ontario Tour donald, daughter of Mr. T. J. Gorm- cessories were in black. The bride wore ley, Alexandria, and of the late Mi's, ja corsage of red roses and lilies of the Eleven servicemen were honored In LONDON, June 8.—As in war, Bri- Hon. Farquhar Oliver, M.P.P. for Gormley, was married to Mr. Bernard valley while the corsage of her .attend the St Telesphore Community Hall on tain went all out in peace today to Southeast Grey and leader of the Lib- W. Villeneuve, son of Mr. -
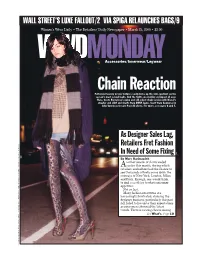
Chain Reaction Patterned Hosiery in Luxe Textures Easily Kicks up the Style Quotient on the Season’S Most Casual Looks
WALL STREET’S LUXE FALLOUT/2 VIA SPIGA RELAUNCHES BAGS/9 WWDWomen’s Wear Daily • The Retailers’MONDAY Daily Newspaper • March 24, 2008 • $2.00 Accessories/Innerwear/Legwear Chain Reaction Patterned hosiery in luxe textures easily kicks up the style quotient on the season’s most casual looks. And the tights are making an impact all over. Here, Custo Barcelona’s nylon and silk velvet chain version with Diesel’s sweater and shirt and shorts from DKNY Jeans. Scarf from Converse by John Varvatos; Cesare Paciotti shoes. For more, see pages 6 and 7. As Designer Sales Lag, Retailers Fret Fashion In Need of Some Fixing By Marc Karimzadeh SENTS; STYLED BY COURT WILLIAMS COURT SENTS; STYLED BY nother season of shows ended Aearlier this month, during which retailers and editors had the chance to see thousands of looks come down the runways of New York, London, Milan and Paris. Enough, one would think, to find something to whet consumer appetites. Not so fast. Many fashion executives are increasingly frustrated, claiming the designer business, particularly this past fall, failed to live up to their expectations as consumers shunned the latest trends. There is a rising chorus among See What’s, Page10 PHOTO BY GEORGE CHINSEE; MODEL: LEAH HIGHT/FUSION; HAIR BY DARIA WRIGHT/DARIAWRIGHT.COM; MAKEUP BY BRYAN LYNDE/RJ BENNETT REPRE LYNDE/RJ BRYAN MAKEUP BY DARIA WRIGHT/DARIAWRIGHT.COM; GEORGE CHINSEE; MODEL: LEAH HIGHT/FUSION; HAIR BY PHOTO BY 2 WWD, MONDAY, MARCH 24, 2008 WWD.COM Wall St. Cutbacks Could Weigh on Luxe By Evan Clark tion of that is in the form of bonuses.