Methsuximide in Intractable Epilepsies in Childhood
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Considerations in Perioperative Assessment of Valproic Acid Coagulopathy Claude Abdallah George Washington University
Himmelfarb Health Sciences Library, The George Washington University Health Sciences Research Commons Anesthesiology and Critical Care Medicine Faculty Anesthesiology and Critical Care Medicine Publications 1-2014 Considerations in perioperative assessment of valproic acid coagulopathy Claude Abdallah George Washington University Follow this and additional works at: http://hsrc.himmelfarb.gwu.edu/smhs_anesth_facpubs Part of the Anesthesia and Analgesia Commons APA Citation Abdallah, C. (2014). Considerations in perioperative assessment of valproic acid coagulopathy. Journal of Anaesthesiology Clinical Pharmacology, Volume 30, Issue 1 (). http://dx.doi.org/10.4103/0970-9185.125685 This Journal Article is brought to you for free and open access by the Anesthesiology and Critical Care Medicine at Health Sciences Research Commons. It has been accepted for inclusion in Anesthesiology and Critical Care Medicine Faculty Publications by an authorized administrator of Health Sciences Research Commons. For more information, please contact [email protected]. [Downloaded free from http://www.joacp.org on Tuesday, February 25, 2014, IP: 128.164.86.61] || Click here to download free Android application for this journal Revv iew Article Considerations in perioperative assessment of valproic acid coagulopathy Claude Abdallah Department of Anesthesiology, Children’s National Medical Center, The George Washington University Medical Center, NW Washington, DC, USA Abstract Valproic acid (VPA) is one of the widely prescribed antiepileptic drugs in children with multiple indications. VPA-induced coagulopathy may occur and constitute a pharmacological and practical challenge affecting pre-operative evaluation and management of patients receiving VPA therapy. This review summarizes the different studies documenting the incidence, severity and available recommendations related to this adverse effect. -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

Health Reports for Mutual Recognition of Medical Prescriptions: State of Play
The information and views set out in this report are those of the author(s) and do not necessarily reflect the official opinion of the European Union. Neither the European Union institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Executive Agency for Health and Consumers Health Reports for Mutual Recognition of Medical Prescriptions: State of Play 24 January 2012 Final Report Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Acknowledgements Matrix Insight Ltd would like to thank everyone who has contributed to this research. We are especially grateful to the following institutions for their support throughout the study: the Pharmaceutical Group of the European Union (PGEU) including their national member associations in Denmark, France, Germany, Greece, the Netherlands, Poland and the United Kingdom; the European Medical Association (EMANET); the Observatoire Social Européen (OSE); and The Netherlands Institute for Health Service Research (NIVEL). For questions about the report, please contact Dr Gabriele Birnberg ([email protected] ). Matrix Insight | 24 January 2012 2 Health Reports for Mutual Recognition of Medical Prescriptions: State of Play Executive Summary This study has been carried out in the context of Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross- border healthcare (CBHC). The CBHC Directive stipulates that the European Commission shall adopt measures to facilitate the recognition of prescriptions issued in another Member State (Article 11). At the time of submission of this report, the European Commission was preparing an impact assessment with regards to these measures, designed to help implement Article 11. -

(12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant Et Al
US 2010.0143507A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2010/014.3507 A1 Gant et al. (43) Pub. Date: Jun. 10, 2010 (54) CARBOXYLIC ACID INHIBITORS OF Publication Classification HISTONE DEACETYLASE, GABA (51) Int. Cl. TRANSAMINASE AND SODIUM CHANNEL A633/00 (2006.01) A 6LX 3/553 (2006.01) A 6LX 3/553 (2006.01) (75) Inventors: Thomas G. Gant, Carlsbad, CA A63L/352 (2006.01) (US); Sepehr Sarshar, Cardiff by A6II 3/19 (2006.01) the Sea, CA (US) C07C 53/128 (2006.01) A6IP 25/06 (2006.01) A6IP 25/08 (2006.01) Correspondence Address: A6IP 25/18 (2006.01) GLOBAL PATENT GROUP - APX (52) U.S. Cl. .................... 424/722:514/211.13: 514/221; 10411 Clayton Road, Suite 304 514/456; 514/557; 562/512 ST. LOUIS, MO 63131 (US) (57) ABSTRACT Assignee: AUSPEX The present invention relates to new carboxylic acid inhibi (73) tors of histone deacetylase, GABA transaminase, and/or PHARMACEUTICALS, INC., Sodium channel activity, pharmaceutical compositions Vista, CA (US) thereof, and methods of use thereof. (21) Appl. No.: 12/632,507 Formula I (22) Filed: Dec. 7, 2009 Related U.S. Application Data (60) Provisional application No. 61/121,024, filed on Dec. 9, 2008. US 2010/014.3507 A1 Jun. 10, 2010 CARBOXYLIC ACID INHIBITORS OF HISTONE DEACETYLASE, GABA TRANSAMNASE AND SODIUM CHANNEL 0001. This application claims the benefit of priority of Valproic acid U.S. provisional application No. 61/121,024, filed Dec. 9, 2008, the disclosure of which is hereby incorporated by ref 0004 Valproic acid is extensively metabolised via erence as if written herein in its entirety. -

Dialysis of Drugs Source Documents Last Updated September 17, 2012
Dialysis of Drugs Source Documents Last updated September 17, 2012 Note: Year indicates date of Dialysis of Drugs edition. Abacavir Izzedine H, et al. Pharmacokinetics of abacavir in HIV-1-infected patients with impaired renal function. Nephron 2001; 89:62-67. (2002) Abatacept Orencia prescribing information (2007) Abiraterone acetate Zytiga prescribing information (2012) Acenocoumarol Sintrom prescribing information (2005) Acetylcysteine Soldini D, et al. Pharmacokinetics of N-acetylcysteine following repeated intravenous infusion in haemodialysis patients. Eur J Clin Pharmacol 2005; 60:859-864. (2006) Acid colloidal hydrocolloid Flamigel package insert (2012) Acitretin Stuck AE, et al. Pharmacokinetics of acitretin and its 13-cis metabolite in patients on haemodialysis. Br J Clin Pharmacol. 1989; 27:301-4. (2004) Aclidinium bromide Tudorza PI (2013) Adalimumab Humira prescribing information (2005) Adefovir Hepsera prescribing information (2004) Professional services information from company (2004) Aflibercept Eylea package information (2013) Agalsidase alfa and beta (see galactosidase) Replagal product information from FDA web site (2006) Kosch M, et al. Enzyme replacement therapy administered during hemodialysis in patients with Fabry disease. Kidney Int 2004; 66:1279-1282. (2005) Pastores GM, et al. Safety and pharmacokinetics of agalsidase alfa in patients with Fabry disease and end-stage renal disease. Nephrol Dial Transplant 2007; 22:1920-1925. (2008) Fabrazyme prescribing information (2008) Replagal product information from European web site (2008) Agomelatine Valdoxan PI (2012) Albinterferon Alfa-2b Serra DB, et al. Single-Dose Pharmacokinetics, Safety, and Tolerability of Albinterferon 1 Alfa-2b in Subjects with End-Stage Renal Disease on Hemodialysis Compared to Those in Matched Healthy Volunteers. Antimicrob Agents Chemother. 2011;55:473-7. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -

Monotherapy Versus Polytherapy in Epilepsy: a Framework for Patient Management
Monotherapy versus Polytherapy in Epilepsy: a Framework for Patient Management J.H. Schneiderman ABSTRACT: The long-standing debate between proponents of monotherapy and those of polytherapy for treatment of epilepsy has been rekindled by the recent development of several new antiepileptic drugs. The likelihood of improved seizure control on polytherapy must be weighed against the risk of increased side effects, complex drug interactions and cost. Providing maximal seizure control while avoiding over- treatment is a challenge which requires an ongoing critical evaluation of each patient's management. This review provides a framework for decision-making by considering issues affecting the choice between monotherapy and polytherapy in five clinical situations: 1) newly diagnosed epilepsy; 2) seizures on monotherapy; 3) seizures controlled on polytherapy; 4) not controlled on polytherapy; 5) change in medi cal condition. RESUME: La monotherapie versus la polytherapie dans Pepilepsie: un cadre pour le traitement des patients. Le vieux debat entre les promoteurs de la monotherapie et ceux de la polytherapie dans le traitement de Pepilepsie a ete repris a cause du developpement recent de plusieurs nouveaux medicaments antiepileptiques. La probability d'un meilleur controle des crises par une polytherapie doit etre evaluee par rapport au risque d'effets secondaires plus importants, d'interactions medicamenteuses complexes et du cout de la medication. C'est un d6fi que d'arriver a un controle maximal des crises tout en evitant de surtraiter, ce qui demande une evaluation critique constante du traite ment de chaque patient. Cette revue fournit un cadre pour la prise de decision en considerant les raisons qui influen- cent le choix entre la monotherapie et la polytherapie dans cinq situations cliniques: 1) un nouveau diagnostic d'epilepsie; 2) des crises sous monotherapie; 3) un controle des crises sous polytherapie; 4) une absence de controle sous polytherapie; 5) un changement dans l'etat medical du patient. -

Antiepileptic Drugs (Aeds) Polypharmacy Could Lead to Buried Pharmacokinetic Interactions Due to CYP450
Send Orders of Reprints at [email protected] Drug Metabolism Letters, 2012, 6, 207-212 207 Antiepileptic Drugs (AEDs) Polypharmacy Could Lead to Buried Pharmacokinetic Interactions due to CYP450 Z. Tolou-Ghamari* Isfahan Neuroscience Research Centre, Faculty of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran Abstract: CYP450 enzymes are basics for the metabolism of several medications such as numerous AEDs. As AEDs polypharmacy could lead to hidden pharmacokinetic interactions due to CYP450, therefore, the aim of this study was to determine a proper guideline for AEDs prescription in Iranian epileptic population. A cross-sectional study of fifty-four patients’ (n=23 females; n= 31 males with a mean age of 27 years) located in the Epilepsy Ward of Kashani Hospital of Isfahan University of Medical Sciences was carried out during the year 2011. Variables including sex, age, age of seizure onset, type and number of AEDs were recorded in d-Base. Results showed that the number of prescriptions based on AEDs polypharmacy was 77.8%. The most important drugs in prescriptions were carbamazepine (n=41) that is a potent inducer of CYP450 and valproic acid (n=31) that is a potent inhibitor of CYP450 simultaneously. Administration of AEDs was based on: three (n=17), four (n=7), five (n=4) or six (n=3) AEDs simultaneously. To avoid side effects, in prescribing AEDs that act as CYP450inhibitors or inducers concomitantly, their spectrum of interactions should be predicted. Keywords: AEDs, polypharmacy, CYP450, inducer, inhibitor. INTRODUCTION sufficiently manage their seizures. There is association between commencement, persistence and discontinuation of Epilepsy is a recurrent neurological disorder AEDs [7]. -
Genetic and Phenotypic Heterogeneity Suggest Therapeutic Implications in SCN2A-Related Disorders
doi:10.1093/brain/awx054 BRAIN 2017: Page 1 of 21 | 1 Genetic and phenotypic heterogeneity suggest therapeutic implications in SCN2A-related disorders Markus Wolff,1,Ã Katrine M. Johannesen,2,3,Ã Ulrike B. S. Hedrich,4,Ã Silvia Masnada,5 Guido Rubboli,2,6 Elena Gardella,2,3 Gaetan Lesca,7,8,9 Dorothe´e Ville,10 Mathieu Milh,11,12 Laurent Villard,12 Alexandra Afenjar,13 Sandra Chantot-Bastaraud,13 Cyril Mignot,14 Caroline Lardennois,15 Caroline Nava,16,17 Niklas Schwarz,4 Marion Ge´rard,18 Laurence Perrin,19 Diane Doummar,20 Ste´phane Auvin,21,22 Maria J. Miranda,23 Maja Hempel,24 Eva Brilstra,25 Nine Knoers,25 Nienke Verbeek,25 Marjan van Kempen,25 Kees P. Braun,26 Grazia Mancini,27 Saskia Biskup,28 Konstanze Ho¨rtnagel,28 Miriam Do¨cker,28 Thomas Bast,29 Tobias Loddenkemper,30 Lily Wong-Kisiel,31 Friedrich M. Baumeister,32 Walid Fazeli,33 Pasquale Striano,34 Robertino Dilena,35 Elena Fontana,36 Federico Zara,37 Gerhard Kurlemann,38 Joerg Klepper,39 Jess G. Thoene,40 Daniel H. Arndt,41 Nicolas Deconinck,42 Thomas Schmitt-Mechelke,43 Oliver Maier,44 Hiltrud Muhle,45 Beverly Wical,46 Claudio Finetti,47 Reinhard Bru¨ckner,48 Joachim Pietz,49 Gu¨nther Golla,50 Dinesh Jillella,51 Karen M. Linnet,52 Perrine Charles,53 Ute Moog,54 Eve O˜ iglane-Shlik,55 John F. Mantovani,56 Kristen Park,57 Marie Deprez,58 Damien Lederer,58 Sandrine Mary,58 Emmanuel Scalais,59 Laila Selim,60 Rudy Van Coster,61 Lieven Lagae,62 Marina Nikanorova,2 Helle Hjalgrim,2,3 G. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

20-427S011 Vigabatrin Clinical BPCA
CLINICAL REVIEW Application Type NDA Efficacy Supplement Application Number(s) NDA 20427 S-011/S-012 (tablet) NDA 22006 S-012/S-013 (oral solution) Priority or Standard Priority Submit Date(s) April 26, 2013 Received Date(s) April 26, 2013 PDUFA Goal Date October 26, 2013 Division / Office DNP/ ODE 1 Reviewer Name(s) Philip H. Sheridan, M.D. Review Completion Date September 27, 2013 Established Name Vigabatrin (Proposed) Trade Name Sabril Therapeutic Class Anticonvulsant Applicant Lundbeck Inc. Formulation(s) Tablet Sachet for Oral Solution Dosing Regimen BID Indication(s) Complex Partial Seizures Infantile Spasms Intended Population(s) Adult and Pediatric Reference ID: 3396639 Template Version: March 6, 2009 APPEARS THIS WAY ON ORIGINAL Reference ID: 3396639 Clinical Review Philip H. Sheridan, MD NDA 20427 S011/S-012; NDA 22006 S-012/S-013 Sabril (Vigabatrin) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 9 1.1 Recommendation on Regulatory Action ............................................................. 9 1.2 Risk Benefit Assessment .................................................................................... 9 1.4 Recommendations for Postmarket Requirements and Commitments .............. 11 2 INTRODUCTION AND REGULATORY BACKGROUND ...................................... 12 2.1 Product Information .......................................................................................... 12 2.2 Tables of Currently Available Treatments for Proposed Indications ................ -
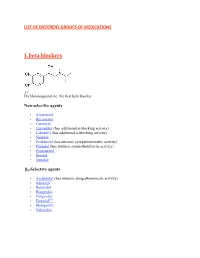
List of Different Groups of Medications
LIST OF DIFFERENT GROUPS OF MEDICATIONS 1.beta blockers Dichloroisoprenaline, the first beta blocker. Non-selective agents • Alprenolol • Bucindolol • Carteolol • Carvedilol (has additional α-blocking activity) • Labetalol (has additional α-blocking activity) • Nadolol • Penbutolol (has intrinsic sympathomimetic activity) • Pindolol (has intrinsic sympathomimetic activity) • Propranolol • Sotalol • Timolol β1-Selective agents • Acebutolol (has intrinsic sympathomimetic activity) • Atenolol • Betaxolol • Bisoprolol • Celiprolol [39] • Esmolol • Metoprolol • Nebivolol 2.Antiarrhythmic classification + • Class I agents interfere with the sodium (Na ) channel. • Class II agents are anti-sympathetic nervous system agents. Most agents in this class are beta blockers. + • Class III agents affect potassium (K ) efflux. • Class IV agents affect calcium channels and the AV node. • Class V agents work by other or unknown mechanisms. • Overview table Clas Known as Examples s • Quinidine • Procainamide Ia fast-channel blockers • Disopyramide • Lidocaine • Phenytoin Ib • Mexiletine Flecainide Ic • • Propafenone • Moricizine • Propranolol • Esmolol • Timolol Metoprolol II Beta-blockers • • Atenolol • Bisoprolol • Amiodarone • Sotalol III IV slow-channel • Verapamil blockers • Diltiazem • Adenosine V • Digoxin 3.Antidepressants Selective serotonin reuptake inhibitors (SSRIs • Celexa): usual dosing is 20 mg initially; maintenance 40 mg per day; maximum dose 60 mg per day. • Escitalopram (Lexapro, Cipralex): usual dosing is 10 mg and shown to be as effective as 20 mg in most cases. Maximum dose 20 mg. Also helps with anxiety. • Paroxetine (Paxil, Seroxat): Also used to treat panic disorder, OCD, social anxiety disorder, generalized anxiety disorder and PTSD. Usual dose 25 mg per day; may be increased to 40 mg per day. Available in controlled release 12.5 to 37.5 mg per day; controlled release dose maximum 50 mg per day.