Bringing Lean to Life: Making Processes Flow in Healthcare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Implementation of Kanban, a Lean Tool, in Switchgear Manufacturing Industry – a Case Study
Proceedings of the International Conference on Industrial Engineering and Operations Management Paris, France, July 26-27, 2018 Implementation of Kanban, a Lean tool, In Switchgear Manufacturing Industry – A Case Study Shashwat Gawande College Of Engineering, Pune Department of Industrial Engineering and management Savitribai Phule Pune University Pune, Maharashtra 44, India [email protected] Prof. J.S Karajgikar College Of Engineering, Pune Department of Industrial Engineering and management Savitribai Phule Pune University Pune, Maharashtra 44, India [email protected] Abstract Kanban is a scheduling system for lean and just in time manufacturing industries or services firms. It is a very effective tool for running a production system as a whole, in this system problem areas are highlighted by measuring lead time and cycle time of the full process the other benefits of the Kanban system is to establish an upper limit to work in process inventory to avoid over capacity. The objective of this case study is to implement a standard Kanban System for a Electrical manufacturing MNC company. With this system, the firm implemented use of just in time to reduce the inventory cost stocked during the process. This case study also shows that the Kanban implementation is not only bounded to the company but to their vendor also, from where, some of the components are been assembled. A replenishment strategy was also developed, tested and improved at the company location. A complete instruction manual is also developed as a reference Keywords Value Steam Mapping, Kanban, Root Cause Analysis, Replenishment Strategy 1. Introduction Lean manufacturing or simply ‘lean’ is a systematic method for waste reduction within a manufacturing system without affecting productivity. -

Extension of the Lean 5S Methodology to 6S with an Additional Layer to Ensure Occupational Safety and Health Levels
sustainability Article Extension of the Lean 5S Methodology to 6S with An Additional Layer to Ensure Occupational Safety and Health Levels Mariano Jiménez 1,2 , Luis Romero 2,* , Jon Fernández 2, María del Mar Espinosa 2 and Manuel Domínguez 2 1 Department of Mechanical Engineering, Technical School of Engineering—ICAI, Comillas Pontifical University, 25, 28015 Madrid, Spain 2 Design Engineering Area, Industrial Engineering School, National Distance Education University (UNED), 38, 28015 Madrid, Spain * Correspondence: [email protected] Received: 12 June 2019; Accepted: 11 July 2019; Published: 12 July 2019 Abstract: This paper proposes an expansion of the Lean 5S methodology, which includes the concept of Safety–Security as 6S. Implementation was done by a standardized process tested in a pilot area that is part of the Integrated Industrial Manufacturing System Laboratory at the Higher Technical School of Engineering (ICAI). The additional 6S phase (Safety-Security) thoroughly reviews all areas of an industrial plant by analyzing the risks at each workstation, which let employees be fitted out with protection resources depending on each of their personal characteristics and to guarantee the safety of the workstation by strictly complying with occupational safety and health and machinery use standards, which must hold a CE certificate of compliance. The main objective was to increase the scope of 5S methodology to respond to the occupational safety and health needs for machines required in optimizing production processes. It is important to remember that companies must guarantee that their employees use personal protection equipment (PPE) at their work posts or stations that protect them properly from risks to their health and safety and that cannot be prevented or sufficiently limited by using collective means of protection or by adopting work organization measures. -

Material Replenishment System
MATERIAL REPLENISHMENT SYSTEM REPLENISHMENT METHODS FOR VISUALIZING MATERIAL NEEDS IN A LEAN MANUFACTURING COMPANY Examensarbete – Högskoleingenjör Industriell ekonomi Stefan Andersson Johan Elfvenfrost År: 2016.18.07 I Svensk titel: Material återfyllningssystem Engelsk titel: Material replenishment system Utgivningsår: 2016 Författare: Stefan Andersson, Johan Elfvenfrost Handledare: Sara Lorén, Högskolan i Borås Magnus Hansson Fallenius, IAC Group Göteborg Examinator: Andreas Hagen II Abstract This thesis work has been written both for and in co-operation with the company IAC Group Gothenburg. The main purpose of the report is to find a new alternative material replenishment system which will improve the internal material flow and eliminate unnecessary work activities such as manual call offs. The aim is to find a new system to reduce the incidental costs incurred and improve customer service in quality and performance. Observations and interviews were conducted and an analysis of the current situation was made. Waste was identified in the form of unnecessary transport, specifically in milk runs, where time was spent looking for materials to be loaded. This creates uncertainty and may contribute to increased costs and poor customer service. Three different options for a new replenishment system were developed which were compared with the theory and present situation. The proposal was evaluated with respect to cost, available support, complexity and future compatibility. The analysis of the theory and current state shows the importance of a long-term solution with few risks of waste. The solution that best cope with this is an e-Kanban system that automates the replenishment system and would make manual material call offs disappear completely. -
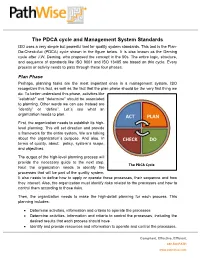
White Paper the PDCA Cycle and Management System Standards
The PDCA cycle and Management System Standards ISO uses a very simple but powerful tool for quality system standards. This tool is the Plan- Do-Check-Act (PDCA) cycle shown in the figure below. It is also known as the Deming cycle after J.W. Deming, who proposed the concept in the 50s. The entire logic, structure, and sequence of standards like ISO 9001 and ISO 13485 are based on this cycle. Every process or activity needs to pass through these four phases. Plan Phase Perhaps, planning tasks are the most important ones in a management system. ISO recognizes this fact, as well as the fact that the plan phase should be the very first thing we do. To better understand this phase, activities like “establish” and “determine” should be associated to planning. Other words we can use instead are “identify” or “define”. Let´s see what an organization needs to plan. ACT PLAN First, the organization needs to establish its high- level planning. This will set direction and provide a framework for the entire system. We are talking about the organization´s purpose. And also, in CHECK DO terms of quality, about: policy, system´s scope, and objectives. The output of the high-level planning process will provide the necessary guide to the next step. The PDCA Cycle Next the organization needs to identify the processes that will be part of the quality system. It also needs to define how to apply or operate these processes, their sequence and how they interact. Also, the organization must identify risks related to the processes and how to control them according to those risks. -

The Concept and Implementation of Kaizen in an Organization
Global Journal of Management and Business Research: A Administration and Management Volume 19 Issue 1 Version 1.0 Year 201 Type: Double Blind Peer Reviewed International Research Journal Publisher: Global Journals Online ISSN: 2249-4588 & Print ISSN: 0975-5853 The Concept and Implementation of Kaizen in an Organization By Lubna Rahman Lina & Hafiz Ullah University of Dhaka Abstract- For continuous improvement in an organization, Japanese philosophy Kaizen is very popular. Flawless concepts of kaizen methodology and proper implementation of tools can lead to a successful kaizen program in a company. From the reviews of various case studies, it has revealed that most of the companies have implemented kaizen efficiently and observe better performance. Besides, some companies also failed to implement kaizen due to the lacking of proper knowledge about the concepts of kaizen. Keywords: kaizen, 5 why technique, 5s, 7 QC tools, 7 wastes, jidoka, PDCA cycle, poka-yoke. GJMBR-A Classification: JEL Code: M00 TheConceptandImplementationofKaizeninanOrganization Strictly as per the compliance and regulations of: © 2019. Lubna Rahman Lina & Hafiz Ullah. This is a research/review paper, distributed under the terms of the Creative Commons Attribution-Noncommercial 3.0 Unported License http://creativecommons.org/licenses/by-nc/3.0/), permitting all non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. The Concept and Implementation of Kaizen in an Organization α σ Lubna Rahman Lina & Hafiz Ullah Abstract - For continuous improvement in an organization, over the longer term, without having to go through any Japanese philosophy Kaizen is very popular. Flawless radical innovation. It can be a much gentler and concepts of kaizen methodology and proper implementation employee-friendly way to institute the changes that must of tools can lead to a successful kaizen program in a occur as a business grows and adapts to its changing company. -

Agile and Devops Overview for Business
NELKINDA SOFTWARE CRAFT Ƅ TRAINING Agile and DevOps Overview for Business Duration: 2 Days Available Languages: English Audience Everyone who is steering or involved in software delivery: Business, Management, Operations, Development, for example: CxOs, managers, directors, team leads, systems administrators, development managers, business analysts, requirements engineers, architects, product owners, scrum masters, IT operations sta', IT stakeholders, developers, testers Goals Agile and DevOps are the big drivers of organizational transformation today. What do they mean? Where do they come from? What are their goals? How can they help my organization and my team? How can I use and implement them? And are there any side-e'ects or challenges to consider? Learn the answers to these questions in a holistic perspective from the CxO level to the code about what Agile and DevOps mean for organizations of all sizes. Contents • Business Case for Improving the Software Development Life Cycle ◦ Evolution of the Software Development Life Cycle (SDLC) ◦ Business Drivers of the SDLC Evolution ◦ Principles of Agile, DevOps, Extreme Programming (XP), and Software Craft ◦ Goals and Objectives of Agile, DevOps (Development Operations), XP, and Software Craft ◦ The Pipeline for Value Delivery • Essential Principles ◦ Manifesto for Agile Software Development ("Agile Manifesto") ◦ The Values and Principles of XP ◦ Manifesto of Software Craft ◦ The Two Values of Software ◦ The Deming (PDCA, plan-do-check-act) Cycle ◦ The XP Feedback Loops ◦ Parkinson's Law and Timeboxing ◦ Conway's Law, Organizational Structure and Cross-functional responsibility ◦ KPIs (Key Performance Indicators) and Drivers: Story-Point Velocity, Cycle Time, WIP (Work In Progress) limit ◦ Heisenberg's Uncertainty Principle of Agile Estimation 1/3 https://nelkinda.com/training/DevOps-Driven-Agile © Copyright 2015-2020 Nelkinda Software Craft Private Limited. -
Implementation of Lean Tools in Apparel Industry to Improve Productivity and Quality
Current Trends in Fashion Technology & Textile Engineering ISSN: 2577-2929 Review Article Curr Trends Fashion Technol Textile Eng Volume 4 - Issue 1 - July 2018 Copyright © All rights are reserved by Prakash C DOI: 10.19080/CTFTTE.2018.04.555628 Implementation of Lean Tools in Apparel Industry to Improve Productivity and Quality Mothilal B and Prakash C* Department of Fashion Technology, Sona College of Technology, India Submission: April 19, 2018; Published: July 02, 2018 *Corresponding author: Prakash C, Department of Fashion Technology, Sona College of Technology, India, Tel No: ; Fax: +91-427- 4099888; Email: Abstract The rapid change in apparel styles, deviation of order quantities and increasing quality levels at the lowest possible cut-rate, demand the market. To increase the productivity of the apparel industries we need to reduce the wastage of the manufacturing and time to manufacture the product.apparel manufacturing Lean is the tool industry to reduce to the be focusedwastage on in moreall process effective of apparel and efficient manufacturing, manufacturing reducing processes cost and for value survival added in anto theimmensely product. competitive This paper proposes the lean tool for the apparel industry to reduce the overall wastage of the industries. Keywords: Abbreviations:Apparel FMEA: industry; Failure Eco-efficiency; Mode and Effect Industrial Analysis; wastes; SFPS: Single Lean Failuretools Points; TPM: Total Productive Maintenance; OEE: Overall Equipment Effectiveness; PDCA: Plan-Do-Check-Act or Plan-Do-Check-Adjust; PDSA: Plan-Do-Study-Act Introduction Tapping D [1] observed that lean strategy is to eliminate wastes Lean tools from the process. Any excess in equipment’s, materials, parts, and working period beyond the requirement is generally referred as of waste (muda), the improvement of quality, and production waste. -

APPLICATION of KANBAN SYSTEM for IMPLEMENTING LEAN MANUFACTURING (A CASE STUDY) 1 2 3 B.Vijaya Ramnath, C
Journal of Engineering Research and Studies Research Article APPLICATION OF KANBAN SYSTEM FOR IMPLEMENTING LEAN MANUFACTURING (A CASE STUDY) 1 2 3 B.Vijaya Ramnath, C. Elanchezhian and R. Kesavan Address for Correspondence 1,2 Research Scholar, 3Asst. Professor, Department of Production Technology, Anna University, MIT Campus, Chennai-44, Tamilnadu Email: [email protected] ====================================================================== ABSTRACT This paper deals with implementation of lean manufacturing in Engine valve machining cell in a leading auto components manufacturing industry in the South India. The main objective of this paper is to provide a background on lean manufacturing, present an overview of manufacturing wastes and introduce the tools and techniques that are used to transform a company into a high performing lean enterprise. Value stream mapping is a main tool used to identify the opportunities for various lean techniques. The focus of the lean manufacturing approach is on cost reduction by eliminating Non- Value added activities. Applications have spanned many sectors including automotive, electronics and consumer products manufacturing. In this paper, Value Stream Mapping (VSM) is used to map the current operating state for production line. This map is used to identify sources of waste and to identify lean tools for reducing the waste. To eliminate the wastes found from the current state map Kanban system is suggested for pre machining section and single piece flow concept is suggested for machining section. Then a future state map has been developed for the system with lean tools applied to it KEYWORDS: Lean manufacturing, Value Stream Mapping and Kanban System 1. INTRODUCTION system focused on and driven by customers, Many manufacturers are now critically both internal and external. -

A Framework of E-Kanban System for Indonesia Automotive Mixed-Model Production Line
International Journal of Science and Research (IJSR) ISSN: 2319-7064 ResearchGate Impact Factor (2018): 0.28 | SJIF (2018): 7.426 A Framework of e-Kanban System for Indonesia Automotive Mixed-Model Production Line Santo Wijaya1, Fransisca Debora2, Galih Supriadi3, Insan Ramadhan4 1Department of Computer Engineering, META Industry of Polytechnic, Cikarang Technopark Building, Lippo Cikarang, West Java 17550, Indonesia 2Department of Industrial Engineering, META Industry of Polytechnic, Cikarang Technopark Building, Lippo Cikarang, West Java 17550, Indonesia 3PT. Trimitra Chitrahasta, Delta Silicon 2 Industrial Estate, West Java 17530, Indonesia 4Agency for the Assessment and Application of Technology, Puspiptek Serpong, Indonesia Abstract: The paper describes a development framework of e-Kanban (electronic Kanban) system for Indonesia automotive mixed- model production line. It is intended to solve problems found during the implementation of traditional kanban system in the subjected company. The traditional kanban system posed inefficiencies in the production line and it has been identified in this paper. The impact is significant in causing delay information for production instruction, loss of kanban cards, inaccurate inventory, and other human- related errors. We also identified that these inefficiencies are also increasing with the increase of product variety and volume in mixed- model production line. The presented framework is the extension of the traditional kanban system that has been running for over one year in the subject company. Design framework objective is to handle all the inefficiencies problem occurred and improve the overall efficiency of material and information flow within the production line. It is a combination of paper-based kanban and software-based kanban system. Paper-based kanban handles the movement of man and material in the production line. -

Takt Time Grouping: a Method to Implement Kanban-Flow Manufacturing in an Unbalanced Process with Moving Constraints Mitchell Alan Millstein University of Missouri-St
University of Missouri, St. Louis IRL @ UMSL Dissertations UMSL Graduate Works 7-6-2014 Takt Time Grouping: A Method to Implement Kanban-Flow Manufacturing in an Unbalanced Process with Moving Constraints Mitchell Alan Millstein University of Missouri-St. Louis, [email protected] Follow this and additional works at: https://irl.umsl.edu/dissertation Part of the Business Commons Recommended Citation Millstein, Mitchell Alan, "Takt Time Grouping: A Method to Implement Kanban-Flow Manufacturing in an Unbalanced Process with Moving Constraints" (2014). Dissertations. 242. https://irl.umsl.edu/dissertation/242 This Dissertation is brought to you for free and open access by the UMSL Graduate Works at IRL @ UMSL. It has been accepted for inclusion in Dissertations by an authorized administrator of IRL @ UMSL. For more information, please contact [email protected]. Takt Time Grouping A Method to Implement Kanban-Flow Manufacturing in an Unbalanced Process with Moving Constraints & Comparison to One Piece Flow and Drum Buffer Rope: Which is Better, When and Why Mitchell A. Millstein M.B.A, Washington University – St. Louis, MO, 1996 B.S., Engineering, Rutgers University – New Brunswick, NJ, 1988 A Thesis Submitted to The Graduate School at the University of Missouri – St. Louis in partial fulfillment of the requirements for the degree Ph.D. in Business Administration with an emphasis in Logistics and Supply Chain Management Advisory Committee Joseph P. Martinich, Ph.D. Chairperson Robert M. Nauss, Ph.D. L. Douglas Smith, Ph.D. Donald C. Sweeney II, Ph.D. Revision: July 2, 2014 Copyright, Mitchell A. Millstein, 2014 1 Contents Abstract ......................................................................................................................................................... 7 Section 1: Introduction ................................................................................................................................ -

Review Paper on “Poka Yoke: the Revolutionary Idea in Total Productive Management” 1,Mr
Research Inventy: International Journal Of Engineering And Science Issn: 2278-4721, Vol. 2, Issue 4 (February 2013), Pp 19-24 Www.Researchinventy.Com Review Paper On “Poka Yoke: The Revolutionary Idea In Total Productive Management” 1,Mr. Parikshit S. Patil, 2,Mr. Sangappa P. Parit, 3,Mr. Y.N. Burali 1,Final Year U.G. Students, Mechanical Engg. Department,Rajarambapu Institute of Technology Islampur (Sangli),Shivaji University, Kolhapur (India) 2,P.G. Student, Electronics Engg. Department, Rajarambapu Institute of Technology Islampur (Sangli), Shivaji University, Kolhapur (India) Abstract: Poka-yoke is a concept in total quality management which is related to restricting errors at source itself. It deals with "fail-safing" or "mistake-proofing". A poka-yoke is any idea generation or mechanism development in a total productive management process that helps operator to avoid (yokeru) mistakes (poka). The concept was generated, and developed by Shigeo Shingo for the Toyota Production System. Keywords— Mistake-proofing, Total quality management, Total productive management. I INTRODUCTION In today’s competitive world any organisation has to manufacture high quality, defect free products at optimum cost. The new culture of total quality management, total productive management in the manufacturing as well as service sector gave birth to new ways to improve quality of products. By using various tools of TQM like KAIZEN, 6 sigma, JIT, JIDCO, POKA YOKE, FMS etc. organisation is intended to develop quality culture.[2,6] The paper is intended to focus basic concept of poka yoke, types of poka yoke system, ways to achieve simple poka yoke mechanism. It also covers practical study work done by various researchers . -

Lean Methodology and Its Derivates Usage for Production Systems in Modern Industry
Applied Engineering Letters Vol.2, No.4, 144-148 (2017) e-ISSN: 2466-4847 LEAN METHODOLOGY AND ITS DERIVATES USAGE FOR PRODUCTION SYSTEMS IN MODERN INDUSTRY Marko Miletić1, Ivan Miletić1 1Faculty of Engineering, University of Kragujevac, Serbia Abstract: ARTICLE HISTORY With lean methodology usage being the only way to stay competitive on Received 15.11.2017. nowadays market, it is important to implement it and spread it through the Accepted 07.12.2017. organization. Available 15.12.2017. In this paper, purpose of lean is explained, the most important definition and tools are given and differences between problem solving approaches are explained. KEYWORDS It can be concluded that problem solving approaches are in first look Lean Manufacturing, World Class Manufacturing, Toyota different, having also different number of steps, but they are adapted to the Production System, Basic Tools, company in which they are used and that they depend on the size, Continuous Improvement complexity and expected closing time of project. 1. INTRODUCTION which is initiated by management and bottom-up initiated by people on shop floor. The concept of lean methodology is nowadays Therefore, TPS is used in many industries and widely used in companies around the world in companies, adapted to its products and needs and order to maximise production by minimising loses now defined as common used methodologies such at the same time. Roots of integration of entire as: Lean [1], Lean Six Sigma [2], World Class production system done in flow was made by Manufacturing, Toyota Production System [3], Ford Henry Ford in 1913. However, true usage of lean Production System, Bosch Production System, etc… concept was started by Toyota owner Kiischiro Purpose of this paper is to show tools widely Toyoda and engineer Kaiichi Ohno after WWII, and used in these methodologies and present their finally summarized in 1980s rebranding their TPS main foundations.