Defining Regulators of Human Hematopoietic Stem Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Parish of St. John Bosco
Parish of St. John Bosco November 26, 2017 260 Westchester Avenue Parish Offices: 16 Washington St., Port Chester, NY 10573 914-881-1400 / Fax: 914-939-2807 Web: Portchestercatholicchurch.org Mass Intentions Saturday, November 25 8:00AM (OLM)(E) +Deceased Parents of Salesians 4:00PM (OLM)(E) +Antonio Boccarossa— Sister Jennifer 7:00PM (OLM)(S) (Salud) Consepcion Tacuri— Esposo Sunday, November 26 7:30AM (OLM)(E) +Rita Ianello— Joe & Sons 9:00AM (OLM)(S) (Cumpl.) Debbie McCarthy— Husband 9:00AM (CC)(P) Pro Populo 11:00AM (OLM)(E) +Kenneth Munnick— Joe & Peggy 11:00AM (CC) (PO) +Stanislaw Kowrach— Daughter 11:00AM (HR)(S) +Jose Cabrera & Rosa Jadan— Rosa Cabrera 12:30PM (CC)(E) +Tullio Scochera— Family 1:00PM (OLM)(S) Accion de Gracias— Familia Gonzalez 5:00PM (OLM )(S) +Felipe Flores— Hermanos Host And Wine Monday, November 27 6:30AM (OLM)(E) All the Deceased on Altar November 26—December 2 8:00AM (OLM)(E) +Diane Chopski— Sister In Memory of: 12:00PM (OLM)(E) +Rosie Carlucci— Carole Fulco Deceased members of the 7:30PM (OLM)(S) +Jesus Espinoza— Su Nieta Dora Rivera Bologna & McCrory Fam. Tuesday, November 28 Requested by: 6:30AM (OLM)(E) +Emily Forta— Son Angelo & Family Family 8:00AM (OLM)(E) +Valentine Family— Marie & Children 12:00PM (OLM)(E) +Angelo Licari— Carole Fulco & Family 7:30PM (OLM)(S) +Ana Rosa Basantes— Hijas & Nietos Wednesday, November 29 Our Parish 6:30AM (OLM)(E) For the People Mission Statement 8:00AM (OLM)(E) +Louise Marino— Gertrude & Anthony Morabito The Parish of St. John Bosco is a 12:00PM (OLM)(E) +Carmela Sirena— Peggyann Munnick multi-cultural, multi-lingual 7:30PM (OLM)(S) (Cumple.) Carlos Pasasin Catholic Faith community that Thursday, November 30 proclaims Jesus Christ. -

State of New Jersey Medicaid Fraud Division Provider Exclusion Report
State of New Jersey 1 Medicaid Fraud Division Provider Exclusion Report Updated on: 8/23/2021 **ADDITIONAL NPI NUMBERS MAY BE ASSOCIATED WITH THE LISTED INDIVIDUALS/ENTITIES** PROVIDER NAME TITLE DATE OF NPI NUMBER STREET CITY STA ZIP ACTION EFFECTIVE EXPIRATION BIRTH TE DATE DATE 2258 PHARMACY, INC. 2258 THIRD AVENUE NEW YORK NY 10035 SUSPENSION 7/20/2003 6522 VENTNOR AVE. 6522 VENTNOR AVENUE VENTNOR NJ 08406 DISQUALIFICATION PHARMACY, INC. ABARCA, CHERYL R. LPN 8/15/1962 528 3RD STREET NEWARK NJ 07107 SUSPENSION 6/20/2005 ABASHKIN, ROMAN CHHA 12/21/1981 72 RIDGEVIEW TERRACE WAYNE NJ 07470 DISQUALIFICATION 5/29/2015 ABASHKIN, ROMAN CHHA 12/21/1981 72 RIDGEVIEW TERRACE WAYNE NJ 07470 DISQUALIFICATION 6/3/2016 ABBASSI, JADAN MD 9/19/1944 1194807255 1618 MAIN AVENUE CLIFTON NJ 07011 DISQUALIFICATION 11/21/2016 PERMANENT ABBASSI, JADAN MD 9/19/1944 1194807255 115 NELLIS DRIVE WAYNE NJ 07470 DISQUALIFICATION 6/20/2018 PERMANENT ABDALLA, IZZELDIN 4/5/1967 1116 ANNE STREET ELIZABETH NJ 07201 DISQUALIFICATION 11/10/1999 ABDELGANI, AMIR ALLENWOOD USP WHITE DEER PA 17887 DISQUALIFICATION 11/26/2001 ABDELGANI, FADIL TERRE HAUTE USP TERRE HAUTE IN 47808 DISQUALIFICATION 11/26/2001 ABDELHAMID, MANAL RPH 5/28/1969 7100 BOULEVARD EAST, 11G GUTTENBERG NJ 07093 DEBARMENT 3/15/2001 ABDOLLAHI, MITRA DMD 8/31/1966 1033329230 646 N. SARATOGA DRIVE MOORESTOWN NJ 08057 DISQUALIFICATION 11/5/2007 7/19/2019 ABERBACH, STEVEN RPH 8/5/1944 23 STONEGATE DRIVE WATCHUNG NJ 07069 DEBARMENT 12/19/2003 ABOOD, ABDOLMAID S. 1/20/1966 64 BEVAN STREET JERSEY CITY NJ 07306 SUSPENSION 5/7/1997 ABOODS MEDICAL LIVERY 64 BEVAN STREET JERSEY CITY NJ 07306 DISQUALIFICATION 5/22/1994 ABOUELHODA, AHMED RPH 3/23/1974 33-17 60TH STREET, APT. -
Marriage Certificates
GROOM LAST NAME GROOM FIRST NAME BRIDE LAST NAME BRIDE FIRST NAME DATE PLACE Abbott Calvin Smerdon Dalkey Irene Mae Davies 8/22/1926 Batavia Abbott George William Winslow Genevieve M. 4/6/1920Alabama Abbotte Consalato Debale Angeline 10/01/192 Batavia Abell John P. Gilfillaus(?) Eleanor Rose 6/4/1928South Byron Abrahamson Henry Paul Fullerton Juanita Blanche 10/1/1931 Batavia Abrams Albert Skye Berusha 4/17/1916Akron, Erie Co. Acheson Harry Queal Margaret Laura 7/21/1933Batavia Acheson Herbert Robert Mcarthy Lydia Elizabeth 8/22/1934 Batavia Acker Clarence Merton Lathrop Fannie Irene 3/23/1929East Bethany Acker George Joseph Fulbrook Dorothy Elizabeth 5/4/1935 Batavia Ackerman Charles Marshall Brumsted Isabel Sara 9/7/1917 Batavia Ackerson Elmer Schwartz Elizabeth M. 2/26/1908Le Roy Ackerson Glen D. Mills Marjorie E. 02/06/1913 Oakfield Ackerson Raymond George Sherman Eleanora E. Amelia 10/25/1927 Batavia Ackert Daniel H. Fisher Catherine M. 08/08/1916 Oakfield Ackley Irving Amos Reid Elizabeth Helen 03/17/1926 Le Roy Acquisto Paul V. Happ Elsie L. 8/27/1925Niagara Falls, Niagara Co. Acton Robert Edward Derr Faith Emma 6/14/1913Brockport, Monroe Co. Adamowicz Ian Kizewicz Joseta 5/14/1917Batavia Adams Charles F. Morton Blanche C. 4/30/1908Le Roy Adams Edward Vice Jane 4/20/1908Batavia Adams Edward Albert Considine Mary 4/6/1920Batavia Adams Elmer Burrows Elsie M. 6/6/1911East Pembroke Adams Frank Leslie Miller Myrtle M. 02/22/1922 Brockport, Monroe Co. Adams George Lester Rebman Florence Evelyn 10/21/1926 Corfu Adams John Benjamin Ford Ada Edith 5/19/1920Batavia Adams Joseph Lawrence Fulton Mary Isabel 5/21/1927Batavia Adams Lawrence Leonard Boyd Amy Lillian 03/02/1918 Le Roy Adams Newton B. -

NAME SCHOOL YEAR SPORT MAJOR Matthew Knych BRY Sr
(3.20 GPA or higher) NAME SCHOOL YEAR SPORT MAJOR Matthew Knych BRY Sr. Baseball Accounting Joseph Paparelli BRY Sr. Baseball Actuarial Math Nathan Wrighter BRY So. Baseball Applied Mathematics Malik Daley BRY Jr. Baseball Finance Nicholas Angelini BRY So. Baseball Finance Jack Owens BRY So. Baseball HRMC Mason Palmieri BRY So. Baseball Management Tyler Panno BRY So. Baseball Marketing Nolan Hayward BRY Jr. Baseball Polictical Science James Ciliento BRY Fr. Baseball Undeclared Nash Eppard BRY Fr. Baseball Undeclared Bryan Hart BRY Fr. Baseball Undeclared Jack Ipsen BRY Fr. Baseball Undeclared James Titus BRY Fr. Baseball Undeclared Gabriel Van Ness BRY Jr. Men’s Golf Accounting Hayden Maroun BRY Sr. Men’s Golf Finance Mckinley Slade BRY Sr. Men’s Golf Finance Cameron Giles BRY So. Men’s Golf Information Systems William Del Biaggio BRY Fr. Men’s Golf Undeclared Connor Henderson BRY Fr. Men’s Golf Undeclared Payton Kim BRY Fr. Men’s Golf Undeclared Daron Merian BRY Fr. Men’s Golf Undeclared Matthew Stafford BRY Fr. Men’s Golf Undeclared Mario Wilson BRY Fr. Men’s Golf Undeclared Thomas Kennedy BRY Jr. Men’s Lacrosse Accounting Kevin Beimfohr BRY So. Men’s Lacrosse Accounting Kyle Mummau BRY Sr. Men’s Lacrosse Biology Spencer Herman BRY Sr. Men’s Lacrosse Entrepreneurship Brett Baker BRY Sr. Men’s Lacrosse Finance Tucker James BRY Sr. Men’s Lacrosse Finance Jared Kaden BRY Sr. Men’s Lacrosse Finance Kenneth Massa BRY Sr. Men’s Lacrosse Finance Charles South BRY Sr. Men’s Lacrosse Finance Michael Tufano BRY Sr. Men’s Lacrosse Finance Kyle Cornell BRY Jr. -

MARYLAND STATE ARTS COUNCIL Meeting Minutes – September 23
MARYLAND STATE ARTS COUNCIL Meeting Minutes – September 23, 2016 The Maryland State Arts Council (MSAC) held its meeting in Baltimore on September 23, 2016. Chair Shelley Morhaim called the meeting to order. Present: Carole Alexander, Barbara Bershon, Aileen Carlucci, Anthony Cornwell, Carla Du Pree, Joan Lyon, Doug Mann, Shelley Morhaim, Jack Rasmussen, Robinson Rowe, Carol Trawick, Gary Vikan, Marty McGowan (Representing Delegate Alonzo Washington), Anne West, MSAC staff Absent: Alex Castro, Senator Richard Madaleno, Julie Madden Guests: Pam Breaux, CEO, National Assembly of State Art Agencies (NASAA), John Schratwieser, Executive Director, Maryland Citizens for the Arts (MCA) Approval of Consent Agenda All consent agenda items were approved as presented. Chair’s Report Shelley Morhaim reported the following: Shelley welcomed everyone to the meeting, then proceeded with roundtable introductions of Council and Staff Welcome to our new Councilors: Aileen Carlucci, Robinson Rowe, and Anne West Welcome to the new Grants and Database Manager, Lauren Fowler It was a busy summer for the Maryland State Arts Council . The IAA awards were held in June Special thanks to the staff for making the evening a great success . Anne & Shelley joined First Lady, Yumi Hogan at an Open House in Hamden . The First Lady also held an art exhibit in August Thanks to those that attended the event . Shelley visited the Ocean City Art League . Theresa and Shelley met with GBCA to discuss various items . Shelley attended the Baltimore City Arts Guild meeting in Pikesville . We held New Councilor Orientation in August Special thanks to Barbara, Julie, and Joan for their participation Shelley, Barbara, and Carol attended the 50th Anniversary Steering Committee meeting The Baker Awards were held at the Baltimore Museum of Art This was a spectacular event The Motor house will be having a grand opening tomorrow of Open Works, which is a makers space Council and staff attended the NASAA conference in Grand Rapids, MI . -
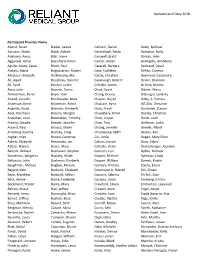
Updated As of May 2018 Participant Provider Name Abend, Susan
Updated as of May 2018 Participant Provider Name Abend, Susan Bieber, James Carlucci, Daniel Daley, Michael Abruzzo, Maria Black, Robert Carmichael, Paula Damiano, Holly Adelowo, Amos Blair, Irene Carswell, Brett Darrah, John Aggarwal, Achal Blanchard, Karyn Cartier, Aileen DeAngelis, AnnMarie Aguilar Lopez, Cesar Block, Paul Casaceli, Barbara DeGrand, David Alatalo, Maria Bogdasarian, Robert Case, Cathleen DePan, Cormac Albakour, Mustafa Bolkhovsky, Alla Castle, Christine Desmond, Cassandra Ali, Asjad Boudreau, Danielle Cavanaugh, Robert Devlin, Shannon Ali, Syed Bourne, Leslie Celestin, James Di Anni, Brooke Alosi, Julie Bowzer, Tonya Chad, David Dibner, Maria Ammerman, Karen Boyer, Gail Chang, Donny DiGiorgio, Lyndsey Anand, Curuchi Braithwaite, Marc Chaplin, Daylin Dilley, S. Patricia Anderson, Kevin Braveman, Robin Chastain, Iryna DiTullio, Christine Angelini, Paula Brennan, Kimberly Chau, Frank Donhowe, Steven Apte, Darshana Brescia, Morgan Chaudhary, Omer Dooley, Christine Arakelian, Joan Bresnahan, Timothy Chen, Linyun Doret, Leah Arcand, Claudia Brewer, Jennifer Chen, Tina Dorfman, Justin Arcand, Paul Briasco, Marie Chiang, Jennifer Drexler, Albert Arramraj, Kavitha Brotsky, Craig Chudasama, Nidhi Druker, Kari Asghar, Irfan Brown, Courtney Ciu, Linda Dugan, Mary Ellen Askew, Elizabeth Brozovsky, Jan Cohen, Joseph Duro, Edlira Atlassi, Hassna Bruce, Mary Collette, Helen Durrenberger, Jocelyne Balcom, William Buchanan, Stephen Connors, Lori Dybka, Michael Balodimos, Iphigenia Buckley, Wade Cooper, Michael Dylewicz, Linda Batbouta, -

Janesville Police Department Adult Arrests Between Selected Dates
Janesville Police Department Adult Arrests Between Selected Dates Arrests From: 12/1/2016 12:00:00AM To: 12/31/2016 12:00:00PM Contact Date Event Number Person Name Location of Arrest Statute Description 12/01/2016 JV1663882STEINHOFF, MATTHEW MARK JPD DISORDERLY CONDUCT 12/01/2016 JV1663882STEINHOFF, MATTHEW MARK JPD CRIMINAL TRESPASS TO DWELLING 12/01/2016 JV1664099PETTIS, AMARIO WESLEY 2837 LIBERTY LANE PROBATION VIOLATION 12/01/2016 JV1663987WESTON, TANNER JOSEPH 220 S JACKSON SEXUAL INTERCOURSE 16 & OLDER 12/01/2016 JV1663987WESTON, TANNER JOSEPH 220 S JACKSON SEXUAL ASSAULT-3RD DEGREE 12/01/2016 JV1663987WESTON, TANNER JOSEPH 220 S JACKSON PROBATION VIOLATION 12/01/2016 JV1663987WESTON, TANNER JOSEPH 220 S JACKSON POS W/INT DEL THC <=200G 12/01/2016 JV1663987WESTON, TANNER JOSEPH 220 S JACKSON MANUF/DELIVER THC <=200G 12/01/2016 JV1664217 PEASE, COREY JON BATTERY 12/01/2016 JV1664222FLOOD, AUSTIN DEAN 123 S RIVER ABUSE HAZARDOUS SUBS- USE 12/01/2016 JV1664228FLOOD, AUSTIN DEAN 123 S RIVER PROBATION VIOLATION 12/01/2016 JV1664206JONSON, EMILY CATHERINE 2500 MILTON AVE RETAIL THEFT-MUNICIPAL 12/01/2016 JV1664206LAMPE, RAQUEL ALISSA 2500 MILTON AVE RETAIL THEFT-MUNICIPAL 12/02/2016 JV1664246WUTTKE, GRIFFIN D 304 N CROSBY ARMED ROBBERY 12/02/2016 JV1664246WUTTKE, GRIFFIN D 304 N CROSBY POSSESS DRUG PARAPHERNALIA 12/02/2016 JV1664246CALTAGERONE, MICHAEL 304 N CROSBY ARMED ROBBERY 12/02/2016 JV1664246DUMMER,C JUSTIN RAYMOND 304 N CROSBY ARMED ROBBERY 12/02/2016 JV1664246WEEKS, TIMMY LEE 304 N CROSBY ARMED ROBBERY 12/02/2016 JV1664246BLYE, -

Rental Properties As of April 2021 # Street Owner 24
RENTAL PROPERTIES AS OF APRIL 2021 # STREET OWNER 24 ADMIRALS WAY TAYLOR, STEVEN C. 1 ALEXANDER DRIVE DELUCA, ANTHONY 2 ALEXANDER DRIVE CATARINA, JOSEPH D 3 ALEXANDER DRIVE MACKER MANAGEMENT, LLC 5 ALEXANDER DRIVE FOX, ZENOBIA 6 ALEXANDER DRIVE CARAVAGGIO, LISA A 9 ALEXANDER DRIVE GARDINER, DAVID R 13 ALEXANDER DRIVE 13 ALEXANDER DRIVE, LLC 18 ALEXANDER DRIVE DEMTY, PAUL J. LIVING TR 22 ALGONQUIN ROAD 22 ALGONQUIN, LLC 23 ALGONQUIN ROAD BROCK, MICHAEL A. 32 ALGONQUIN ROAD HAUTANIEMI, JUSTIN 51 ALGONQUIN ROAD GOODISON, RICHARD 100 ALGONQUIN ROAD #25 CARLTON, DONALD R., JR. 14 ALGONQUIN TRAIL ARAS, TIMOTHY E. 37 ALGONQUIN TRAIL SEASIDE PROPERTIES, LLC 7 ALLAGASH TRAIL GREENBERG, MARTIN B 10 ALLAGASH TRAIL VOSE, DEAN 14 ALLAGASH TRAIL MANCINI NARRAGANSETT TRUST 27 ALLAGASH TRAIL BOURK, DAVID J 31 ALLAGASH TRAIL TARRO, ANTHONY M 44 ALLAGASH TRAIL CHOQUETTE, JAMES H. 45 ALLAGASH TRAIL MCMORROW, THOMAS 52 ALLAGASH TRAIL PAB PROPERTIES, LLC 75 ALLAGASH TRAIL ROSSONI, ERIC P 89 ALLAGASH TRAIL SZUMITA, RICHARD P 97 ALLAGASH TRAIL THIS MUST BE THE PLACE, LLC 99 ALLAGASH TRAIL AIELLO, PETER 101 ALLAGASH TRAIL AIELLO, PETER R 117 ALLAGASH TRAIL RAPILLO, STEVEN 14 ANAWAN AVENUE PROCACCINI, JONATHON ERIK 15 ANAWAN AVENUE SPIEZIO, NICHOLAS J 7 ANCHORAGE ROAD CONTILLO, MARY B 16 ANCHORAGE ROAD PARE, STEVEN M 27 ANCHORAGE ROAD ZANFARDINO, FRANK P 1 ANGELL ROAD JENNINGS, ROY T. 2 ANGELL ROAD REYNOLDS, JOSEPH P, II 4 ANGELL ROAD DIRAIMO, MICHAEL R REVOC TRUST 6 ANGELL ROAD BARBIERI, BLAIR J 9 ANGELL ROAD KELLY, JOHN J. III 11 ANGELL ROAD JENE, MARY-JEAN ET AL 12 ANGELL ROAD DELMONICO, DOMENIC 14 ANGELL ROAD LEONE, JASON T 16 ANGELL ROAD GAFFNEY, ANTHONY J 17 ANGELL ROAD MG HOLDINGS, LLC 23 ANGELL ROAD RUSSO, JOHN R. -

Town of Manchester, Ct Real Estate Property List (With Assessment Data) Listing Ownership As of May 17, 2018
TOWN OF MANCHESTER, CT REAL ESTATE PROPERTY LIST (WITH ASSESSMENT DATA) LISTING OWNERSHIP AS OF MAY 17, 2018 To Search in Adobe Reader / Acrobat: Press Control Key + F and enter in the Street Name you are looking for CONDO STREET UNIT # STREET NAME # OWNER'S NAME CO-OWNER'S NAME 17 AARON DRIVE ANSALDI ASSOCIATES 20 AARON DRIVE BRODEUR MICHAEL P & CYNTHIA L 2 ABBE ROAD BUGNACKI MICHAEL 9 ABBE ROAD BUGNACKI MICHAEL & SHEILA 23 ABBE ROAD BUGNACKI MICHAEL 37 ABBE ROAD ZYREK ANDREW R & ZYREK GEORGE P 3 ACADEMY STREET ZIMOWSKI AMIE C 11 ACADEMY STREET LALIBERTE ERNEST A & MARGARET 15 ACADEMY STREET LAVOIE DAVID & KRISTIN 16 ACADEMY STREET CURRY RICHARD L L/U & JAMES F & OLINATZ LAURA J 19 ACADEMY STREET RYAN ERIN M 20 ACADEMY STREET RIVAL JESSICA & JAMES 23 ACADEMY STREET WHITAKER RICHARD A & JOANN B 30 ACADEMY STREET SNYDER JOSEPH T 37 ACADEMY STREET COTE RONALD R & DIANE L 47 ACADEMY STREET MOORE COREY ANTONIO 48 ACADEMY STREET TEDFORD GORDON W 49 ACADEMY STREET CZAPOROWSKI JOAN M & JANE H 54 ACADEMY STREET THOMAS MONIQUE A 55 ACADEMY STREET WAGGONER ALBERT A JR & SUZAN E FERAGNE PAUL & LAUREL 57 ACADEMY STREET LETITIA MARGARET C 58 ACADEMY STREET VAIDA MATTHEW R 62 ACADEMY STREET HITE DEREK & SHACARRA 24 ADAMS STREET MANCHESTER SPORTS CENTER INC 33 ADAMS STREET RETAIL PROPERTY TWO LLC 41 ADAMS STREET CONNECTICUT SOUTHERN RAILROAD INC ATTN TAX DEPARTMENT 45 ADAMS STREET FAY JOHN P 58 ADAMS STREET POM-POM GALI LLC 60 ADAMS STREET POM-POM GALI LLC 81 ADAMS STREET EIGHTY ONE ADAMS STREET LLC 81 ADAMS STREET EIGHTY ONE ADAMS STREET LLC 109 ADAMS -

Calendar/Parent Guide
Croton-Harmon Schools Calendar & Parent Guide 2021–2022 chufsd.org 2 A Message from the Superintendent of Schools Dear Croton-Harmon Students, Parents, Staff and I encourage our Croton-Harmon School Community to be bold in our critical Community, thinking and always choose to demonstrate character by taking initiative, thinking flexibly, and using empathy. It is with pure joy that I welcome you to the 2021-2022 school year. It is a time for new beginnings and wonderful Although this has been a time of significant change, many constants remain. Our opportunities. Over the past year our students, faculty, staff administrators, teachers and staff eagerly wait to greet our students and are ready and community have all shown great resilience. As we look to begin another incredible school year. So let’s get started!! toward the future, we know how effectively we can work through challenges together as a learning community. Yours in Mission Possible, As I reflect on our tagline, “Think.Create.Reflect.Respect.” I am reminded about how critical thinking, (the process Dr. Deborah O’Connell of continuously asking questions while acquiring knowledge, developing a plan, Dr. Deborah O’Connell, Superintendent of Schools evaluating a claim, supporting an idea, and considering different perspectives), is central to our work as a school district, and know that our teachers and administrators have been busy planning for this school year which I am sure promises to be rich with opportunities to think critically. Additionally, our tagline speaks to one’s character. Developing character is equally as important as being a critical and creative thinker. -

Total Aaaaa Name PP Perf. PP Perf. PP Perf
Silo Ptrifecta Pfour Man Jeffe's HB Club Championship BMW M/M Ind. Match Play Team Match Play Total aaaaa name PP Perf. PP Perf. PP Perf. PP Perf. PP Perf. PP Perf. PP Perf. PP Perf. 0 Acromite, Gary 20 20 20 60 Adfield, Donovan 20 40 60 Aggers, Steve 20 20 40 Ahrens, Thomas 20 60 80 Allen, Mike 20 80 20 80 200 Ambrose, Jay 20 60 20 20 40 20 20 80 280 Anderson, David 20 20 Anderson, Greg 20 20 Ashton, John 20 20 40 Avery, Brandon 20 20 160 20 120 340 Avery, Guy 20 160 20 40 240 Balfanz, Todd 20 20 Barbour, Bob 20 40 20 80 Beaty, Shaun 20 80 20 20 20 20 20 120 320 Benshoof, Jim 20 20 20 40 20 20 80 220 Benshoof, Mitch 20 20 40 20 20 120 Bobolz, David 20 20 20 20 80 Bopp, Alan 20 20 20 20 160 240 Bordewick, Christian 20 20 Bourg, Kenneth 20 80 100 Brown, Mike 20 40 20 40 20 20 20 20 200 Buchner, Mitch 20 160 180 Bundy, Bill 20 60 20 100 Burns, Chris 20 20 20 160 220 Callies, Lance 20 60 20 20 160 280 Campbell, Craig 20 20 40 Carlucci, Brandon 20 20 Carson, Kendall 20 20 Chester, Craig 20 40 20 40 20 20 60 220 Chinnock, Tom 20 20 20 60 Clair, Francis 20 20 40 80 Cogan, Scott 20 20 Crowley, John 20 20 40 Curry, Ray 20 80 100 Dean, Ray 20 20 40 Decker, Gene 20 20 Dees, Josh 20 20 Demirorz, Bahadir 20 60 20 100 Devenny, Paul 20 80 100 Devine, Garrett 20 20 Devine, Mark 20 120 140 Dyekman, Gary 20 20 60 20 20 20 80 240 Earley, Mark 20 20 40 Eide, Aaron 20 60 20 20 120 Eikner, David 20 60 20 100 Eikner, Matt 20 60 20 100 Eisenhauer, John 20 20 20 20 80 English, Ron 20 20 Everett, Steve 20 20 20 80 20 20 80 20 280 Everhart, Dallas 20 20 20 80 -

Carlucci, Frank
The Association for Diplomatic Studies and Training Foreign Affairs Oral History Project AMBASSADOR FRANK CHARLES CARLUCCI III Interviewed by: Charles Stuart Kennedy Initial interview date: April 1, 1997 Copyright 2000 A ST TABLE OF CONTENTS (Continuation of inter iew) State Department - Bureau of Near East Affairs 1956-1957 Suez Crisis ,ohannesburg. South Africa - Commercial Officer 1957-1959 African National Congress En ironment Foreign Ser ice Institute 0FSI1 - French 2anguage Training 1959-1960 2eopold ille. Congo - Political Officer 1960-1962 Independence Patrice 2umumba Riots Flight to Stanley ille Rescuing Belgians E acuation 6atanga secession CIA Russian assistance Adoula 6asa ubu Carlucci attac7ed Allison Palmer 8N operation 9obutu House arrest Stanley ille Congolese go ernment State Department - Congo Des7 Officer 1962-1963 State team 1 Congressional interest 8N in ol ement (Stanley ille E ent) State Department - Personnel Officer 1963 ;anzibar - First Secretary General 1964-1965 En ironment Communist bloc presence NASA trac7ing station 6arume Go ernment contacts Tanzania merger Press 2umumba 8ni ersity PNGed >Punishment? State Department - FSI - Italian 2anguage Training 1965 Rio de ,aneiro. Brazil - Portuguese 2anguage Training 1965 Rio de ,aneiro. Brazil - Executi e Officer 1965-196A 9ilitary go ernment 9AAG mission TOPSB mission Aid program suspended Cernon (Dic7) Dalters Staff Dissent Tuthill Economic problems Brasilia Politics 8.S. objecti es Democracy Anti-Americanism CIA Office of Economic Opportunity - Director 196A-1970 2egal Ser ices Program California Rural 2egal Assistance Programs Friends and foes >Haircut? suits 2 Dhite House support ,ohn 9itchell Office of 9anagement and Budget 1970-1972 George Shultz Office of 9inority Business Enterprise Go ernment departments - assessment Federal budget Budget and Impoundment Act of 1974 Defense budget Supplemental Security Income Program President NixonFs iews Deinberger and Shultz Re enue sharing Nixon Dhite House firing Department of Health.