The Impacts, Vulnerabilities, and Interventions Associated With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Forestry Books, 1820-1945
WASHINGTON STATE FORESTRY BIBLIOGRAPHY: BOOKS, 1820‐1945 (334 titles) WASHINGTON STATE FORESTRY BIBLIOGRAPHY BOOKS (published between 1820‐1945) 334 titles Overview This bibliography was created by the University of Washington Libraries as part of the Preserving the History of U.S. Agriculture and Rural Life Grant Project funded and supported by the National Endowment of the Humanities (NEH), Cornell University, the United States Agricultural Information Network (USAIN), and other land‐grant universities. Please note that this bibliography only covers titles published between 1820 and 1945. It excludes federal publications; articles or individual numbers from serials; manuscripts and archival materials; and maps. More information about the creation and organization of this bibliography, the other available bibliographies on Washington State agriculture, forestry, and fisheries, and the Preserving the History of U.S. Agriculture and Rural Life Grant Project for Washington State can be found at: http://www.lib.washington.edu/preservation/projects/WashAg/index.html Citation University of Washington Libraries (2005). Washington State Agricultural Bibliography. Retrieved from University of Washington Libraries Preservation Web site, http://www.lib.washington.edu/preservation/projects/WashAg/index.html © University of Washington Libraries, 2005, p. 1 WASHINGTON STATE FORESTRY BIBLIOGRAPHY: BOOKS, 1820‐1945 (334 titles) 1. After the War...Wood! s.l.: [1942]. (16 p.). 2. Cash crops from Washington woodlands. S.l.: s.n., 1940s. (30 p., ill. ; 22 cm.). 3. High‐ball. Portland, Ore.: 1900‐1988? (32 p. illus.). Note: "Logging camp humor." Other Title: Four L Lumber news. 4. I.W.W. case at Centralia; Montesano labor jury dares to tell the truth. Tacoma: 1920. -
Jefferson County Hazard Identification and Vulnerability Assessment 2011 2
Jefferson County Department of Emergency Management 81 Elkins Road, Port Hadlock, Washington 98339 - Phone: (360) 385-9368 Email: [email protected] TABLE OF CONTENTS PURPOSE 3 EXECUTIVE SUMMARY 4 I. INTRODUCTION 6 II. GEOGRAPHIC CHARACTERISTICS 6 III. DEMOGRAPHIC ASPECTS 7 IV. SIGNIFICANT HISTORICAL DISASTER EVENTS 9 V. NATURAL HAZARDS 12 • AVALANCHE 13 • DROUGHT 14 • EARTHQUAKES 17 • FLOOD 24 • LANDSLIDE 32 • SEVERE LOCAL STORM 34 • TSUNAMI / SEICHE 38 • VOLCANO 42 • WILDLAND / FOREST / INTERFACE FIRES 45 VI. TECHNOLOGICAL (HUMAN MADE) HAZARDS 48 • CIVIL DISTURBANCE 49 • DAM FAILURE 51 • ENERGY EMERGENCY 53 • FOOD AND WATER CONTAMINATION 56 • HAZARDOUS MATERIALS 58 • MARINE OIL SPILL – MAJOR POLLUTION EVENT 60 • SHELTER / REFUGE SITE 62 • TERRORISM 64 • URBAN FIRE 67 RESOURCES / REFERENCES 69 Jefferson County Hazard Identification and Vulnerability Assessment 2011 2 PURPOSE This Hazard Identification and Vulnerability Assessment (HIVA) document describes known natural and technological (human-made) hazards that could potentially impact the lives, economy, environment, and property of residents of Jefferson County. It provides a foundation for further planning to ensure that County leadership, agencies, and citizens are aware and prepared to meet the effects of disasters and emergencies. Incident management cannot be event driven. Through increased awareness and preventive measures, the ultimate goal is to help ensure a unified approach that will lesson vulnerability to hazards over time. The HIVA is not a detailed study, but a general overview of known hazards that can affect Jefferson County. Jefferson County Hazard Identification and Vulnerability Assessment 2011 3 EXECUTIVE SUMMARY An integrated emergency management approach involves hazard identification, risk assessment, and vulnerability analysis. This document, the Hazard Identification and Vulnerability Assessment (HIVA) describes the hazard identification and assessment of both natural hazards and technological, or human caused hazards, which exist for the people of Jefferson County. -

Supreme Court of the United States ______
No. 19-247 In the Supreme Court of the United States __________________ CITY OF BOISE, IDAHO, Petitioner, v. ROBERT MARTIN, ET AL., Respondents. __________________ On Petition for Writ of Certiorari to the United States Court of Appeals for the Ninth Circuit __________________ BRIEF OF THE CITY OF ABERDEEN, WASHINGTON AMICUS CURIAE IN SUPPORT OF THE CITY OF BOISE __________________ JOHN EDWARD JUSTICE MARY PATRICE KENT JEFFREY SCOTT MYERS Corporation Counsel Law, Lyman, Daniel, Counsel of Record Kamerrer & Bogdanovich, P.S. Office of Corporation Counsel, Post Office Box 11880 City of Aberdeen Olympia, WA 98508-1880 200 East Market Street (360) 754-3480 Aberdeen, WA 98520 (360) 357-3511 (fax) (360) 537-3233 [email protected] (360) 532-9137 (fax) [email protected] [email protected] Counsel for Amicus Curiae City of Aberdeen, Washington in Support of Petition of City of Boise Becker Gallagher · Cincinnati, OH · Washington, D.C. · 800.890.5001 i TABLE OF CONTENTS TABLE OF AUTHORITIES . iii INTEREST OF AMICUS CURIAE . 1 SUMMARY OF ARGUMENT . 2 ARGUMENT . 3 I. Context/Background . 3 II. Aberdeen Experience: River Street Property ..................................... 5 A. Background ........................ 5 B. Monroe, et al. v. City of Aberdeen, et al. 8 C. Aitken, et al. v. City of Aberdeen . 8 III. Martin does not clearly define “available overnight shelter” . 12 IV. Martin has impermissibly expanded prohibitions against criminalization to generally applicable protections of public health and welfare. 13 V. Martin has created unintended consequences including appropriating of public property for personal use; and shifting responsibility for local management of homelessness to the federal judiciary. 15 A. -

Pacific Lamprey 2020 Regional Implementation Plan Washington
Pacific Lamprey 2020 Regional Implementation Plan for the Washington Coast/Puget Sound Regional Management Units Submitted to the Conservation Team August 12, 2020 Primary Authors Primary Editors M.Plumb U.S. Fish and Wildlife Service This page left intentionally blank I. Status and Distribution of Pacific lamprey in the RMUs A. General Description of the RMUs The Puget Sound/Strait of Juan de Fuca Region is bordered by the Strait of Juan de Fuca to the west, the Cascade Range to the east, Puget Sound systems to the south, and the U.S.–Canada border to the north (Figure 1). The Puget Sound/Strait of Juan de Fuca Region includes all Washington river basins flowing into the Puget Sound, Hood Canal, and Strait of Juan de Fuca. The major river basins in the Puget Sound initiate from the Cascade Range and flow west, discharging into Puget Sound, with the exception of the Fraser River system, which flows northwest into British Columbia. All of the major river basins in Hood Canal and the Strait of Juan de Fuca originate in the Olympic Mountains. This region is comprised of 20 4th field HUCs ranging in size from 435-6,604 km2 (Table 1). The Washington Coast Region is bordered by the Pacific Ocean to the West, Cape Flattery to the North, Olympic Mountain Range and Willapa Hills to the East, and the Columbia River to the South (Figure 2). This region includes all Washington river basins flowing directly into the Pacific Ocean. The Washington Coast Region includes the Hoh-Quillayute, Queets-Quinault, Upper and Lower Chehalis, Grays Harbor, and Willapa Bay sub-regions, or 4th field HUCs, ranging in size from 1,471-3,393 km2 (Table 2). -

The Resource
Chapter II THE RESOURCE LOCATOR MAP OF CLALLAM COUNTY DESCRIPTION OF PLANNING AREA • NARRATIVE • PHYSICAL FEATURES • CHARACTERISTIC LANDSCAPES HISTORIC RESOURCES • NATIONAL REGISTER OF HISTORIC PLACES • WASHINGTON STATE REGISTER OF HISTORIC PLACES APPENDICES • APPENDIX A – GENERALIZED FUTURE LAND USE MAP • APPENDIX B – PHYSIOGRAPHIC ZONES MAP • APPENDIX C – CHARACTERISTIC LANDSCAPES MAP LOCATOR OF MAP CLALLAM COUNTY Chapter II, Page 1 DESCRIPTION OF THE PLANNING AREA NARRATIVE Clallam County lies across the northern half of Washington’s Olympic Peninsula, the northwest corner of the Pacific Northwest. Its western and northern boundaries are the Pacific Ocean and Strait of Juan de Fuca shorelines. The southern boundary cuts through Olympic National Park, the nearly million-acre wilderness interior of the Peninsula. The high mountains, rugged coastlines, deep forest, miles of unspoiled rivers, clean air and water, and mild marine climate offer a most unusual combination of environmental amenities. When the cultural, educational, and social amenities available in the cities and towns are considered, along with the range of living styles from small town to rural to backwoods, the county becomes a uniquely desirable place to live and work. The county is rich in natural resources. The Olympic Peninsula is one of the most productive timber-growing areas in the country, and 60 percent of Clallam County’s land area is in commercial timberland. The ocean waters once contained a vast fishery. Salmon have been the most significant species for commercial and sports fishermen, but twenty-four other commercially significant species are also landed. Some species of salmon have now become listed as threatened or endangered. -

Olympic Peninsula Tourism Commission 2019 Media Kit
Olympic Peninsula Tourism Commission 2019 Media Kit Hoh Rain Forest, Olympic National Park Located in Washington’s northwest corner, the Olympic Peninsula is a land like no other. It is both environmentally and culturally rich. From the jigsaw coastlines, temperate rainforest, and glacial-capped peaks of Olympic National Park to the organic farms and wineries of the Dungeness and Chimacum Valleys; from the cultural centers of native tribes dotting the Highway 101 Pacific Coast Scenic Byway to the maritime history of its port towns, there’s an adventure for every age and spirit here. Holiday Lights Blyn, WA Olympic National Park A Modern-day Eden The Olympic Peninsula is home to the 1,400 square mile Olympic National Park. A designated UNESCO World Heritage Site and International Biosphere Reserve, the park has three distinctly different ecosystems; the Pacific coastline, the Olympic Mountains and the primeval rain forests. In 1976, Olympic became an International Biosphere Reserve; and in 1981, it was designated a World Heritage Site. These diverse ecosystems are still largely pristine due to its wilderness designations. The wild and rugged coastline along the Pacific Ocean stretches over 70 miles and is the longest undeveloped coast in the contiguous United States. The extensive alpine forests are home to some of the world’s largest conifers, towering 300 feet tall and measuring 25 feet around. Among the ancient forests of old-growth trees exists the largest temperate rainforest on the earth. Found on the Pacific Coast of North America, stretching from Oregon to Alaska. The rugged Olympic Mountains, home to Mount Olympus and over 60 glaciers, are thought to be beautiful enough for the gods to dwell. -

02-Grays Harbor Sediment Literature Review
Plaza 600 Building 600 Stewart Street, Suite 1700 Seattle, Washington 98101 206.728.2674 June 29, 2015 National Fisheries Conservation Center 308 Raymond Street Ojai, California 93023 Attention: Julia Sanders Subject: Cover Letter Literature Review & Support Services Grays Harbor, Washington File No. 21922-001-00 GeoEngineers has completed the literature search regarding sedimentation within Grays Harbor estuary. The attached letter report and appendices summarize our efforts to gather and evaluate technical information regarding the sedimentation conditions in Grays Harbor, and the corresponding impacts to shellfish. This literature search was completed in accordance with our signed agreement dated May 5, 2015, and is for the express use of the National Fisheries Conservation Center and its partners in this investigation. We will also provide to you electronic copies of the references contained in the bibliography. We thank you for the opportunity to support the National Fisheries Conservation Center as you investigate the sedimentation issues in Grays Harbor. We look forward to working with you to develop mitigation strategies that facilitate ongoing shellfish aquaculture in Grays Harbor. Sincerely, GeoEngineers, Inc. Timothy P. Hanrahan, PhD Wayne S. Wright, CFP, PWS Senior Fluvial Geomorphologist Senior Principal TPH:WSW:mlh Attachments: Grays Harbor Literature Review & Support Services Letter Report Figure 1. Vicinity Map Appendix A. Website Links Appendix B. Bibliography One copy submitted electronically Disclaimer: Any electronic form, facsimile or hard copy of the original document (email, text, table, and/or figure), if provided, and any attachments are only a copy of the original document. The original document is stored by GeoEngineers, Inc. and will serve as the official document of record. -
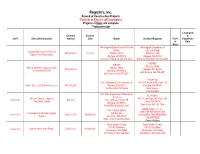
Projects *Projects in Red Are Still in Progress Projects in Black Are Complete **Subcontractor
Rognlin’s, Inc. Record of Construction Projects *Projects in Red are still in progress Projects in black are complete **Subcontractor % Complete Contract Contract & Job # Description/Location Amount Date Owner Architect/Engineer Class Completion of Date Work Washington Department of Fish and Washington Department of Wildlife Fish and Wildlife Log Jam Materials for East Fork $799,000.00 01/11/21 PO Box 43135 PO Box 43135 Satsop River Restoration Olympia, WA 98504 Olympia, WA 98504 Adrienne Stillerman 360.902.2617 Adrienne Stillerman 360.902.2617 WSDOT WSDOT PO Box 47360 SR 8 & SR 507 Thurston County PO Box 47360 $799,000.00 Olympia, WA 98504 Stormwater Retrofit Olympia, WA 98504 John Romero 360.570.6571 John Romero 360.570.6571 Parametrix City of Olympia 601 4th Avennue E. 1019 39th Avenue SE, Suite 100 Water Street Lift Station Generator $353,952.76 Olympia, WA 98501 Puyallup, WA 98374 Jim Rioux 360-507-6566 Kevin House 253.604.6600 WA State Department of Enterprise SCJ Alliance Services 14th Ave Tunnel – Improve 8730 Tallon Lane NE, Suite 200 20-80-167 $85,000 1500 Jefferson Street SE Pedestrian Safety Lacey, WA 98516 Olympia, WA 98501 Ross Jarvis 360-352-1465 Bob Willyerd 360.407.8497 ABAM Engineers, Inc. Port of Grays Harbor 33301 9th Ave S Suite 300 Terminals 3 & 4 Fender System PO Box 660 20-10-143 $395,118.79 12/08/2020 Federal Way, WA 98003-2600 Repair Aberdeen, WA 98520 (206) 357-5600 Mike Johnson 360.533.9528 Robert Wallace Grays Harbor County Grays Harbor County 100 W. -
2020 Visitor Guide & Business Directory
2020 Visitor Guide & Business Directory NORTH MASON North Mason Chamber of Commerce 1967 – 2020 Allyn • Belfair • Grapeview • Hoodsport • Lake Cushman Mason Lake • Shelton • Skokomish Valley • Tahuya • Union 2020 Visitor Guide & Business Directory Table of Contents • Acknowledgements ............. 43 Welcome to Our “Sunset Edition!” • Allyn ....................................... 15 • Belfair .................................... 16 • Belfair Licensing ................. 4 • Boys & Girls Club ................. 12 • Chairman’s Welcome........... 4 • Chairman’s Circle ................. 6 • Chamber Dues ..................... 6 • Chamber Royalty ................. 8-9 • Cornhole at the Gala! .......... 10 • Festivals ................................. 24 • Golf ........................................ 29 • Grapeview ............................ 17 • Hoodsport/Cushman/Skok. 20 • HUB Center for Seniors ........ 12 • MAP / Advertiser List ........... 22 • Mason Lake .......................... 18 • Medical Services ................. 13 • Membership Alphabetical 34 • Membership by Category ..... 30 • North Mason Schools ......... 14 • Parks & Recreation .............. 28 • President/CEO’s Message .... 6 • Shelton .................................. 19 • Shop Local ............................ 7 COVER: Picture your dream day – on Hood Canal? Case Inlet? Lake Cushman? Spencer Lake? The list goes on. • Tahuya .................................. 26 All it takes is a couple of inflatable floaties, the beverage of your choice, and of course, who will spend -

Bucket List Runs on Washington's Olympic Peninsula
Bucket List Runs on Washington’s Olympic Peninsula Lace Up Your Tennys and Get Ready to Be Wowed FOR IMMEDIATE RELEASE PRESS CONTACT Lynnette Braillard, 541-350-0594 [email protected] (Port Angeles, Washington) Foot running season in Port Angeles, Washington kicks off every spring with several running, walking and multi-sport events on the Olympic Peninsula and in the Olympic National Park. These four fitness events and runs should be on your bucket list: North Olympic Discovery Marathon – Every June http://nodm.com/ This scenic run along the Strait of Juan de Fuca takes place along a section of the Olympic Discovery Trail – a 70+ mile paved trail system that extends from Port Townsend to Port Angeles and beyond. This full marathon, half-marathon, 10K and 5K running event is an official Boston Marathon qualifier and a certified USA Track & Field course. There’s also a marathon walk, a marathon relay option and a 1.2-mile kids’ run. The best place for spectating is the finish line at City Pier in downtown Port Angeles. A percentage of race fees go to local charities – over $20,000 was given out in 2017. Over 600 volunteers ensure this race is well- organized and the local craft beer and wine at the finish line keeps the waterfront party going. Riding your bike to the start line is encouraged – bike parking is available at the new green bike racks in front of H2O Waterfront Bistro in downtown. GOAT Run (Great Olympic Adventure Trail) – Every September https://greatoatrun.org/ This is the only run on the Olympic Peninsula that goes into the Olympic National Park. -

Vegetation Classification for San Juan Island National Historical Park
National Park Service U.S. Department of the Interior Natural Resource Stewardship and Science San Juan Island National Historical Park Vegetation Classification and Mapping Project Report Natural Resource Report NPS/NCCN/NRR—2012/603 ON THE COVER Red fescue (Festuca rubra) grassland association at American Camp, San Juan Island National Historical Park. Photograph by: Joe Rocchio San Juan Island National Historical Park Vegetation Classification and Mapping Project Report Natural Resource Report NPS/NCCN/NRR—2012/603 F. Joseph Rocchio and Rex C. Crawford Natural Heritage Program Washington Department of Natural Resources 1111 Washington Street SE Olympia, Washington 98504-7014 Catharine Copass National Park Service North Coast and Cascades Network Olympic National Park 600 E. Park Ave. Port Angeles, Washington 98362 . December 2012 U.S. Department of the Interior National Park Service Natural Resource Stewardship and Science Fort Collins, Colorado The National Park Service, Natural Resource Stewardship and Science office in Fort Collins, Colorado, publishes a range of reports that address natural resource topics. These reports are of interest and applicability to a broad audience in the National Park Service and others in natural resource management, including scientists, conservation and environmental constituencies, and the public. The Natural Resource Report Series is used to disseminate high-priority, current natural resource management information with managerial application. The series targets a general, diverse audience, and may contain NPS policy considerations or address sensitive issues of management applicability. All manuscripts in the series receive the appropriate level of peer review to ensure that the information is scientifically credible, technically accurate, appropriately written for the intended audience, and designed and published in a professional manner. -

Eastern Jefferson County Bicycle Map North Beach Co
Admiralty Inlet Strait of Juan de Fuca Map Legend Eastern Jefferson County Bicycle Map North Beach Co. Park P.S. Express T 4ft + 2ft to 4ft No h POINT WILSON pugetsoundexpress.com re e C This map is intended to provide information to cyclists so that they can make their own decisions as to which route is 360/385-5288 Shoulder Shoulder Shoulder r Introduction ab s Fort Worden State Park Ferry to San Juan Islands R suited for their skill level. Facilities on the Olympic Peninsula range from narrow roads with no shoulders to roads with bike lanes or wide d 49th St shoulders, separated trails with no motorized traffic to off-road mountain bike trails. Likewise, vehicular traffic varies from low to high on the ek re W St C Washington State Ferries e y roads throughout the area. v r A e k ve l o Port Townsend–Coupeville Route a o Walnut St s s C Jackson St wsdot.wa.gov/ferries a C The roads have been coded with input from local bicycle commuters, recreational cyclists 888/808-7977 d Port Townsend Jamestown R and transportation planners using criteria important to bicyclists. Grade, pavement A Juan San Caution Area: narrow roads, poor visibility or no shoulders Fir St Protection Island Cherry St n condition, paved shoulder width, vehicle travel lane width, traffic volumes and F St Monroe St L Hastings Ave Visitor Information Center x POINT o Olympic Discovery Trail: Off-road On-Road c speed were some of the factors used in determining the suitability of the National Wildlife Refuge l e 360/385-2722 i v HUDSON A Woodcock Rd W s Strangers enjoypt.com roads.