Prezbellmunt2015.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Iliopsoas Tendonitis/Bursitis Exercises
ILIOPSOAS TENDONITIS / BURSITIS What is the Iliopsoas and Bursa? The iliopsoas is a muscle that runs from your lower back through the pelvis to attach to a small bump (the lesser trochanter) on the top portion of the thighbone near your groin. This muscle has the important job of helping to bend the hip—it helps you to lift your leg when going up and down stairs or to start getting out of a car. A fluid-filled sac (bursa) helps to protect and allow the tendon to glide during these movements. The iliopsoas tendon can become inflamed or overworked during repetitive activities. The tendon can also become irritated after hip replacement surgery. Signs and Symptoms Iliopsoas issues may feel like “a pulled groin muscle”. The main symptom is usually a catch during certain movements such as when trying to put on socks or rising from a seated position. You may find yourself leading with your other leg when going up the stairs to avoid lifting the painful leg. The pain may extend from the groin to the inside of the thigh area. Snapping or clicking within the front of the hip can also be experienced. Do not worry this is not your hip trying to pop out of socket but it is usually the iliopsoas tendon rubbing over the hip joint or pelvis. Treatment Conservative treatment in the form of stretching and strengthening usually helps with the majority of patients with iliopsoas bursitis. This issue is the result of soft tissue inflammation, therefore rest, ice, anti- inflammatory medications, physical therapy exercises, and/or injections are effective treatment options. -

The Effect of Stretching Hamstring, Gastrocnemius, Iliopsoas
Open Journal of Therapy and Rehabilitation, 2015, 3, 139-145 Published Online November 2015 in SciRes. http://www.scirp.org/journal/ojtr http://dx.doi.org/10.4236/ojtr.2015.34019 The Effect of Stretching Hamstring, Gastrocnemius, Iliopsoas and Back Muscles on Pain and Functional Activities in Patients with Chronic Low Back Pain: A Randomized Clinical Trial Hamada E. Seif1, Aqeel Alenazi2, Sahar Mahmoud Hassan1, Shaji John Kachanathu3, Ashraf R. Hafez1* 1Cairo UniversityHospital, Cairo University, Cairo, Egypt 2Physical Therapy and Rehabilitation Department, College of Applied Medical Sciences, Salman Bin Abdulaziz University, Alkharj, Saudi Arabia 3Collage of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia Received 15 September 2015; accepted 6 November 2015; published 9 November 2015 Copyright © 2015 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract A back pain lasting more than 12 weeks has been defined as a chronic low back pain (LBP) [1]. More than half of people suffer from LBP [1]. The purpose of this study was to examine the effect of gastrocnemius muscle stretching in the treatment of chronic low back pain. Methods: Forty pa- tients with chronic low back pain, ages ranging from 25 to 40 years, were recruited and divided randomly into two groups. The control group followed a physical therapy program that included stretching exercises for back, hamstring and iliopsoas muscles. Strengthening exercises for abdo- minal muscle and postural instructions for activities of daily living were also performed. The ex- perimental group followed the same control-group exercises with the addition of stretching exer- cises for gastrocnemius muscles. -

Thieme: an Illustrated Handbook of Flap-Raising Techniques
4 Part 1 Flaps of the Upper Extremity Chapter 1 dyle are palpated and marked. A straight line is The Deltoid Fasciocutaneous Flap marked to connect these two landmarks. The groove between the posterior border of the del- toid muscle and the long head of triceps is pal- pated and marked. The intersection of these two lines denotes approximately the location of the vascular pedicle, as it emerges from under- The deltoid free flap is a neurovascular fascio- neath the deltoid muscle. This point may be cutaneous tissue, providing relatively thin sen- studied with a hand-held Doppler and marked sate tissue for use in soft-tissue reconstruction. if required. The deltoid fasciocutaneous flap was first de- Depending on the recipient area, the patient scribed anatomically and applied clinically by is positioned either supine, with the donor Franklin.1 Since then, the deltoid flap has been shoulder sufficiently padded with a stack of widely studied and applied.2–5 This flap is sup- towels, or in the lateral decubitus position. Myo- plied by a perforating branch of the posterior relaxants are required in muscular individuals, circumflex humeral artery and receives sensa- so as to ease retraction of the posterior border tion by means of the lateral brachial cutaneous of the deltoid muscle, especially if a long vascu- nerve and an inferior branch of the axillary lar pedicle is required for reconstruction. nerve. This anatomy is a constant feature, thus making the flap reliable. The ideal free deltoid Neurovascular Anatomy flap will be thin, hairless, of an adequate size, and capable of sensory reinnervation. -

Strain Assessment of Deep Fascia of the Thigh During Leg Movement
Strain Assessment of Deep Fascia of the Thigh During Leg Movement: An in situ Study Yulila Sednieva, Anthony Viste, Alexandre Naaim, Karine Bruyere-Garnier, Laure-Lise Gras To cite this version: Yulila Sednieva, Anthony Viste, Alexandre Naaim, Karine Bruyere-Garnier, Laure-Lise Gras. Strain Assessment of Deep Fascia of the Thigh During Leg Movement: An in situ Study. Frontiers in Bioengineering and Biotechnology, Frontiers, 2020, 8, 15p. 10.3389/fbioe.2020.00750. hal-02912992 HAL Id: hal-02912992 https://hal.archives-ouvertes.fr/hal-02912992 Submitted on 7 Aug 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. fbioe-08-00750 July 27, 2020 Time: 18:28 # 1 ORIGINAL RESEARCH published: 29 July 2020 doi: 10.3389/fbioe.2020.00750 Strain Assessment of Deep Fascia of the Thigh During Leg Movement: An in situ Study Yuliia Sednieva1, Anthony Viste1,2, Alexandre Naaim1, Karine Bruyère-Garnier1 and Laure-Lise Gras1* 1 Univ Lyon, Université Claude Bernard Lyon 1, Univ Gustave Eiffel, IFSTTAR, LBMC UMR_T9406, Lyon, France, 2 Hospices Civils de Lyon, Hôpital Lyon Sud, Chirurgie Orthopédique, 165, Chemin du Grand-Revoyet, Pierre-Bénite, France Fascia is a fibrous connective tissue present all over the body. -
Changes in the Quadriceps-To-Hamstring Muscle
Original Article https://doi.org/10.14474/ptrs.2019.8.1.45 Phys Ther Rehabil Sci pISSN 2287-7576 2019, 8 (1), 45-51 eISSN 2287-7584 www.jptrs.org Changes in the quadriceps-to-hamstring muscle ratio http://crossmark.crossref.org/dialog/?doi=10.14474/ptrs.2019.8.1.45&domain=pdf&date_stamp=2019-3-25 during wall squatting according to the straight leg raise test angle Jaeeun Kima, HyeonA Kimb, JuYeong Leeb, HoYoung Leeb, Hyoseung Jungb, YunKi Chob, HyeMin Choib, Donghyun Yic, Daewon Kangc, Jongeun Yimb,c a Department of Physical Therapy, Barosun Hospital, Seoul, Republic of Korea b Department of Physical Therapy, College of Health and Welfare, Sahmyook University, Seoul, Republic of Korea c Department of Physical Therapy, The Graduate School, Sahmyook University, Seoul, Republic of Korea Objective: The purpose of this study was to investigate the muscle activity ratio of the lower limb according to changes in straight leg raise (SLR) test angles on hamstring muscle shortening during squat exercises. Design: Randomized controlled trial. Methods: The subjects were 14 healthy adults who were informed of and agreed to the method and purpose of the study. The par- ticipants were classified into SLR groups according to two angles (over 80° or under 80°) assessed using the SLR tests. After train- ing and practicing the wall squat posture to be applied to the experiment, electromyography (EMG) was used to measure changes in muscle activity during the performance of a wall squat. After stretching, a sequence of pre-stretch tests were performed again, and the active and passive SLR tests were also reconducted; thereafter, a wall squat was performed again by attaching EMG electrodes. -

The Fascia Lata of the Thigh – More Than a “Stocking”: a Magnetic Resonance Imaging, Ultrasonography and Dissection Study
The Fascia Lata of the Thigh – More Than a “Stocking”: A Magnetic Resonance Imaging, Ultrasonography and Dissection Study. Willem Fourie. School of Anatomical Sciences, University of the Witwatersrand, 7 York Road, Parktown 2193, Johannesburg, South Africa. Phone: +27 (0)11 763 6990. Fax: +27 (0)866 180 179. E-mail: [email protected] BACKROUND: Regional descriptions of the thigh mostly exclude detailed descriptions of the fascia lata and its relationships to underlying muscles. It is cursorily described as “a strong, dense, broad single layer of deep fascia investing the thigh muscles like a stocking”. This “stocking” contributes to increased compartment pressure when the muscles contract, aiding venous return. With recent growing understanding of the role of deep fascia, it seems like the fascia lata may not solely be for compartmentalisation, containment and aiding venous return. OBSERVATIONS: During dissections of cadaver thighs, we observed that the fascial relations to underlying muscles differ from textbook descriptions, forming a separate fascia covering some muscles, while acting as an epimysial cover to others in the same region. Furthermore, in an ultrasonography (US) pilot study, some regions of the upper thigh appeared as a triple layer of fascia covering muscles. Both these observations contradicted the general descriptions in literature. AIMS: 1. To investigate the above observations further. 2. Comparing dissection observations and living subjects using magnetic resonance imaging (MRI) and ultrasonography (US). METHODS: Detailed dissection of eight cadaver thighs compared to observations from MRI and US of four living subjects’ thighs. Observations were done at the same four levels on all the thighs. RESULTS: While vastus lateralis observations corresponded to textbook descriptions, US showed the fascia lata as a triple layer in places. -
Muscle Length of the Hamstrings Using Ultrasonography Versus Musculoskeletal Modelling
Journal of Functional Morphology and Kinesiology Article Muscle Length of the Hamstrings Using Ultrasonography Versus Musculoskeletal Modelling Eleftherios Kellis * , Athina Konstantinidou and Athanasios Ellinoudis Laboratory of Neuromechanics, Department of Physical Education and Sport Sciences at Serres, Aristotle University of Thessaloniki, 62100 Serres, Greece; [email protected] (A.K.); [email protected] (A.E.) * Correspondence: [email protected] Abstract: Muscle morphology is an important contributor to hamstring muscle injury and malfunc- tion. The aim of this study was to examine if hamstring muscle-tendon lengths differ between various measurement methods as well as if passive length changes differ between individual hamstrings. The lengths of biceps femoris long head (BFlh), semimembranosus (SM), and semitendinosus (ST) of 12 healthy males were determined using three methods: Firstly, by identifying the muscle attach- ments using ultrasound (US) and then measuring the distance on the skin using a flexible ultrasound tape (TAPE-US). Secondly, by scanning each muscle using extended-field-of view US (EFOV-US) and, thirdly, by estimating length using modelling equations (MODEL). Measurements were performed with the participant relaxed at six combinations of hip (0◦, 90◦) and knee (0◦, 45◦, and 90◦) flexion angles. The MODEL method showed greater BFlh and SM lengths as well as changes in length than US methods. EFOV-US showed greater ST and SM lengths than TAPE-US (p < 0.05). SM length change across all joint positions was greater than BFlh and ST (p < 0.05). Hamstring length predicted using regression equations is greater compared with those measured using US-based methods. The EFOV-US method yielded greater ST and SM length than the TAPE-US method. -

Quadriceps and Hamstrings Coactivation in Exercises Used in Prevention And
bioRxiv preprint doi: https://doi.org/10.1101/574210; this version posted March 11, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Quadriceps and hamstrings coactivation in exercises used in prevention and 2 rehabilitation of hamstring strain injury in young soccer players 3 Gonzalo Torres1¶; David Chorro1¶; Archit Navandar2¶; Javier Rueda1¶; Luís 4 Fernández3¶; Enrique Navarro1*¶ 5 6 1Faculty of Sport Sciences, Universidad Politécnica de Madrid, Madrid, Madrid, Spain. 7 2Faculty of Sport Sciences, Universidad Europea de Madrid, Madrid, Madrid, Spain. 8 3Medical Services of Atlético de Madrid, Club Atlético de Madrid, Madrid, Madrid, 9 Spain. 10 11 12 *Corresponding author 13 E-mail: [email protected] (EN) 14 15 ¶These authors contributed equally to this work. 16 17 18 19 20 21 22 23 24 bioRxiv preprint doi: https://doi.org/10.1101/574210; this version posted March 11, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 25 Abstract 26 This study aimed to study the co-activation of hamstring-quadriceps muscles 27 during submaximal strength exercises without the use of maximum voluntary isometric 28 contraction testing and compare (i) the inter-limb differences in muscle activation, (ii) the 29 intra-muscular group activation pattern, and (iii) the activation during different phases of 30 the exercise. -
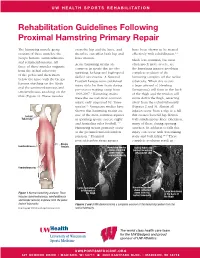
Rehabilitation Guidelines Following Proximal Hamstring Primary Repair
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines Following Proximal Hamstring Primary Repair The hamstring muscle group cross the hip and the knee, and have been shown to be treated consists of three muscles: the therefore can affect both hip and effectively with rehabilitation.1, 8 biceps femoris, semitendinosus knee motion. Much less common, but most and semimembranosus. All Acute hamstring strains are often much more severe, are three of these muscles originate common in sports that involve the hamstring injuries involving from the ischial tuberosity sprinting, kicking and high-speed complete avulsion of the of the pelvis and then insert skilled movements. A National hamstring complex off the ischial below the knee with the biceps Football League team published tuberosity. When this occurs femoris attaching on the fibula injury data for their team during a large amount of bleeding and the semimembranosus and pre-season training camp from (hematoma) will form in the back semitendinosus attaching on the 1998-2007.1 Hamstring strains of the thigh and the tendon will tibia (Figure 1). These muscles were the second most common move down the thigh, retracting injury, only surpassed by “knee away from the ischial tuberosity sprains”.1 Numerous studies have (Figures 2 and 3). Almost all shown that hamstring strains are injuries occur from a slip or a fall Ischial one of the most common injuries that creates forceful hip flexion Tuberosity in sprinting sports, soccer, rugby with simultaneous knee extension, and Australian rules football.1-12 -
Hamstring Muscle Injuries
DISEASES & CONDITIONS Hamstring Muscle Injuries Hamstring muscle injuries — such as a "pulled hamstring" — occur frequently in athletes. They are especially common in athletes who participate in sports that require sprinting, such as track, soccer, and basketball. A pulled hamstring or strain is an injury to one or more of the muscles at the back of the thigh. Most hamstring injuries respond well to simple, nonsurgical treatments. Anatomy The hamstring muscles run down the back of the thigh. There are three hamstring muscles: Semitendinosus Semimembranosus Biceps femoris They start at the bottom of the pelvis at a place called the ischial tuberosity. They cross the knee joint and end at the lower leg. Hamstring muscle fibers join with the tough, connective tissue of the hamstring tendons near the points where the tendons attach to bones. The hamstring muscle group helps you extend your leg straight back and bend your knee. Normal hamstring anatomy. The three hamstring muscles start at the bottom of the pelvis and end near the top of the lower leg. Description A hamstring strain can be a pull, a partial tear, or a complete tear. Muscle strains are graded according to their severity. A grade 1 strain is mild and usually heals readily; a grade 3 strain is a complete tear of the muscle that may take months to heal. Most hamstring injuries occur in the thick, central part of the muscle or where the muscle fibers join tendon fibers. In the most severe hamstring injuries, the tendon tears completely away from the bone. It may even pull a piece of bone away with it. -

Anatomical Variation of the Semitendinosus Muscle Origin
eISSN 1308-4038 International Journal of Anatomical Variations (2013) 6: 225–227 Case Report Anatomical variation of the semitendinosus muscle origin Published online December 28th, 2013 © http://www.ijav.org Patrick Richard FRASER Abstract Addison Reed WOOD During a routine dissection of an 87-year-old female cadaver, an aberrant muscle attachment (AMA) of the right semitendinosus (ST) muscle origin was discovered medial to the primary Armando Aviles ROSALES muscle origin. This attachment originated from the medial portion of the ischial tuberosity and inferior to the sacrotuberous ligament attachment site. It then traveled distally in the long axis Department of Cell Biology and Anatomy, University of of the femur to join the ST muscle, which showed no other variations in structure. Variation in hamstring muscle origins has been shown to predispose patients to hamstring strains and North Texas Health Science Center, 3500 Camp Bowie posterior thigh pain. This study describes a previously undocumented variation of the ST Boulevard, Fort Worth, Texas, 76107-2699, USA. origin that could predispose a patient to the aforementioned thigh pain, as well as pelvic floor pain. Patients presenting with recurrent pain or dysfunction in these areas should prompt an investigation into possible variations of hamstring muscle origins. Armando Rosales, MD © Int J Anat Var (IJAV). 2013; 6: 225–227. Department of Cell Biology & Anatomy University of North Texas Health Science Center 3500 Camp Bowie Boulevard Fort Worth, TX 76107-2699, USA. +1 (817) 735-2032 [email protected] Received February 26th, 2013; accepted August 22nd, 2013 Key words [semitendinosus] [variation] [strain] [hamstring] [muscle] Introduction 2). -
Structural Kinesiology Class 11
STRUCTURAL KINESIOLOGY CLASS 11 With John Maguire WHAT WE WILL COVER IN THIS CLASS Muscles of the Large Intestine: • Fascia Lata • Hamstrings • Lumborum The Emergency Mode 2 FASCIA LATA MUSCLE PAGE 224 Meridian Large Intestine Organ Large Intestine Action Flexes, medially rotates and abducts the hip. Origin Iliac crest posterior to the ASIS Insertion Iliotibial band Muscle Test The supine person holds the leg in a position of abduction, internal rotation, and hip flexion with the knee in hyperextension. Push the leg down and in towards the other ankle NL Top of the thigh to below the knee cap along the iliotibial band Back: a triangle from L2 – L4 on the soft tissue in the back NV #10 Parietal Eminence Indications • Intestinal problems of constipation, spastic colon, colitis and diarrhea, • Chest soreness and breast pain with menstruation. • Postural sign is the legs tend to bow 3 HAMSTRINGS PAGE 226 Meridian Large Intestine Organ Large Intestine – particularly the rectum Action Biceps Femoris (lateral hamstring) – Flexes the knee, laterally rotates the hip and the flexed knee and extends the hip. Semitendinosus and Semimembranosus (medial hamstrings) Flexes the knee, medially rotates the hip and extends the hip. Origin Ischial tuberosity and the back middle of the femur Insertion Biceps Femoris – Head of the fibula. Semitendinosus – top inside of the tibia Semimembranosus – back of the medial condyle of the tibia Muscle Test With the leg bent so the angle of the calf and the thigh is slightly more than 90 degrees, exert pressure in the middle of the hamstring to prevent cramping. Pressure is against the back of the achilles tendon to straighten the leg.