Full Text (PDF)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EGFR Confers Exquisite Specificity of Wnt9a-Fzd9b Signaling in Hematopoietic Stem Cell Development
bioRxiv preprint doi: https://doi.org/10.1101/387043; this version posted August 7, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Grainger, et al, 2018 EGFR confers exquisite specificity of Wnt9a-Fzd9b signaling in hematopoietic stem cell development Stephanie Grainger1, Nicole Nguyen1, Jenna Richter1,2, Jordan Setayesh1, Brianna Lonquich1, Chet Huan Oon1, Jacob M. Wozniak2,3,4, Rocio Barahona1, Caramai N. Kamei5, Jack Houston1,2, Marvic Carrillo-Terrazas3,4, Iain A. Drummond5,6, David Gonzalez3.4, Karl Willert#,¥,1, and David Traver¥,1,7. ¥co-corresponding authors: [email protected]; [email protected] #Lead contact 1Department of Cellular and Molecular Medicine, University of California, San Diego, La Jolla, California, 92037, USA. 2Biomedical Sciences Graduate Program, University of California, San Diego, La Jolla, California, 92037, USA. 3Skaggs School of Pharmacy and Pharmaceutical Science, University of California, San Diego, La Jolla, California, 92093, USA. 4Department of Pharmacology, University of California, San Diego, La Jolla, California, 92092 5Massachusetts General Hospital Nephrology Division, Charlestown, Massachusetts, 02129, USA. 6Harvard Medical School, Department of Genetics, Boston MA 02115 7Section of Cell and Developmental Biology, University of California, San Diego, La Jolla, California, 92037, USA. Running title: A mechanism for Wnt-Fzd specificity in hematopoietic stem cells Keywords: hematopoietic stem cell (HSC), Wnt, Wnt9a, human, zebrafish, Fzd, Fzd9b, FZD9, EGFR, APEX2 1 bioRxiv preprint doi: https://doi.org/10.1101/387043; this version posted August 7, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. -

Complement Pathway Biomarkers and Age-Related Macular Degeneration
Eye (2016) 30, 1–14 © 2016 Macmillan Publishers Limited All rights reserved 0950-222X/16 www.nature.com/eye 1 2,3 Complement pathway M Gemenetzi and AJ Lotery REVIEW biomarkers and age- related macular degeneration Abstract In the age-related macular degeneration accounts for 35% of all cases of late AMD and (AMD) ‘inflammation model’, local inflamma- 20% of legal blindness attributable to AMD,4,5 tion plus complement activation contributes to cannot be treated or prevented at the moment the pathogenesis and progression of the dis- and indeed may be increased by anti-VEGF ease. Multiple genetic associations have now therapy.6,7 been established correlating the risk of devel- In this review, we present and comment on opment or progression of AMD. Stratifying the response to both complement and non- patients by their AMD genetic profile may complement-based treatments, in relation to facilitate future AMD therapeutic trials result- complement pathway mechanisms and ing in meaningful clinical trial end points with complement gene regulation of these smaller sample sizes and study duration. mechanisms. We discuss current and potential – Eye (2016) 30, 1 14; doi:10.1038/eye.2015.203; treatments for both wet and dry AMD in relation published online 23 October 2015 to complement pathway pathogenetic 1Royal Eye Unit, Kingston mechanisms. Hospital NHS Foundation Trust, Kingston Upon Thames, UK Introduction The complement system Based on the pioneering work of Dr Judah The innate immune system is composed of 2Southampton Eye Unit, ‘ ’ Folkman, novel research into angiogenesis immunological effectors that provide robust, Southampton University Hospital, Southampton, UK generated the commercial development of drugs immediate, and nonspecific immune responses. -

G Protein-Coupled Receptors
S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2015/16: G protein-coupled receptors. British Journal of Pharmacology (2015) 172, 5744–5869 THE CONCISE GUIDE TO PHARMACOLOGY 2015/16: G protein-coupled receptors Stephen PH Alexander1, Anthony P Davenport2, Eamonn Kelly3, Neil Marrion3, John A Peters4, Helen E Benson5, Elena Faccenda5, Adam J Pawson5, Joanna L Sharman5, Christopher Southan5, Jamie A Davies5 and CGTP Collaborators 1School of Biomedical Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK, 2Clinical Pharmacology Unit, University of Cambridge, Cambridge, CB2 0QQ, UK, 3School of Physiology and Pharmacology, University of Bristol, Bristol, BS8 1TD, UK, 4Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK, 5Centre for Integrative Physiology, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2015/16 provides concise overviews of the key properties of over 1750 human drug targets with their pharmacology, plus links to an open access knowledgebase of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. The full contents can be found at http://onlinelibrary.wiley.com/doi/ 10.1111/bph.13348/full. G protein-coupled receptors are one of the eight major pharmacological targets into which the Guide is divided, with the others being: ligand-gated ion channels, voltage-gated ion channels, other ion channels, nuclear hormone receptors, catalytic receptors, enzymes and transporters. These are presented with nomenclature guidance and summary information on the best available pharmacological tools, alongside key references and suggestions for further reading. -

Multi-Functionality of Proteins Involved in GPCR and G Protein Signaling: Making Sense of Structure–Function Continuum with In
Cellular and Molecular Life Sciences (2019) 76:4461–4492 https://doi.org/10.1007/s00018-019-03276-1 Cellular andMolecular Life Sciences REVIEW Multi‑functionality of proteins involved in GPCR and G protein signaling: making sense of structure–function continuum with intrinsic disorder‑based proteoforms Alexander V. Fonin1 · April L. Darling2 · Irina M. Kuznetsova1 · Konstantin K. Turoverov1,3 · Vladimir N. Uversky2,4 Received: 5 August 2019 / Revised: 5 August 2019 / Accepted: 12 August 2019 / Published online: 19 August 2019 © Springer Nature Switzerland AG 2019 Abstract GPCR–G protein signaling system recognizes a multitude of extracellular ligands and triggers a variety of intracellular signal- ing cascades in response. In humans, this system includes more than 800 various GPCRs and a large set of heterotrimeric G proteins. Complexity of this system goes far beyond a multitude of pair-wise ligand–GPCR and GPCR–G protein interactions. In fact, one GPCR can recognize more than one extracellular signal and interact with more than one G protein. Furthermore, one ligand can activate more than one GPCR, and multiple GPCRs can couple to the same G protein. This defnes an intricate multifunctionality of this important signaling system. Here, we show that the multifunctionality of GPCR–G protein system represents an illustrative example of the protein structure–function continuum, where structures of the involved proteins represent a complex mosaic of diferently folded regions (foldons, non-foldons, unfoldons, semi-foldons, and inducible foldons). The functionality of resulting highly dynamic conformational ensembles is fne-tuned by various post-translational modifcations and alternative splicing, and such ensembles can undergo dramatic changes at interaction with their specifc partners. -

New Developments in Glaucoma Therapy
New Developments in Glaucoma Therapy 100 - Oral Author: Ganesh Prasanna Presenter: Ganesh Prasanna Institution: Alcon Research Ltd Department: Glaucoma Research Ganesh Prasanna, Ph.D. Ocular Biology, Pfizer Global R&D, San Diego, CA 92121 Current affiliation: Alcon Research Ltd., Fort Worth, TX 76134 EFFECT OF PF-04217329 A PRO-DRUG OF A SELECTIVE PROSTAGLANDIN EP2 AGONIST ON INTRAOCULAR PRESSURE IN PRECLINICAL MODELS OF GLAUCOMA Purpose: While prostaglandin FP analogs are leading the therapeutic intervention for glaucoma, new target classes also are being identified with new lead compounds being developed for IOP reduction. One target class currently being investigated includes the prostaglandin EP receptor agonists. Recently PF-04217329 (Taprenepag isopropyl), a prodrug of CP-544326 (active acid metabolite), a potent and selective EP2 receptor agonist, was successfully evaluated for its ocular hypotensive activity in a clinical study involving patients with primary open angle glaucoma. The preclinical attributes of CP-544326 and PF-0421329 will be presented. Methods: PF-04217329 and active acid metabolite, CP-544326 were evaluated in cell based assays for receptor binding and EP2 receptor functional activity were used. Rabbits were used for assessing corneal permeability, ocular pharmacokinetic studies, EP2 receptor activation and IOP, whereas normal dogs and lasered ocular hypertensive cynomolgus monkeys were also used for IOP studies. Results: CP-544326 was found to be a potent and selective EP2 agonist (receptor binding IC50 = 10 nM; functional activity EC50 = 0.25 nM) whose corneal permeability and ocular bioavailability were significantly increased when the compound was dosed as the isopropyl ester prodrug, PF-04217329. Topical ocular dosing of PF-04217329 was well tolerated in preclinical species and caused an elevation of cAMP in aqueous humor/iris-ciliary body indicative of in-vivo EP2 target receptor activation. -

MCR-17-2-Highlights 335..335
Molecular Cancer Research Highlights February 2019 * Volume 17 * Number 2 Selected Articles from This Issue Protein-protein interaction network involving genes associated with GO:receptor activity Pan-Cancer Metastasis Correlates TGFBR3 ACVR2A NR2C2 NR2F1 AHR HNF4G HNF4A GRIK5 ARNT CALCRL CRCP ASGR1 TLR4 TLR5 GRID2 et al. DLG3 MED13 CFI TSHR ASGR2 TNFRSF4 CD226 Chen and Zhang Page 476 TLR1 ERBB4 MED17 SEC63 TLR10 AGER GRIA2 NR0B2 MED30 GLP1R LHCGR DERL1 TNFRSF9 ITGB2 KCNJ1 ESRRG NR5A2 Chen and Zhang and colleagues describe a systematic analysis SEC62 SORL1 MERTK BMPR2 GPR183 TRAM1 BMPR1A CFTR KCNH2 GPC6 of molecular correlates of metastasis using The Cancer Genome NRP1 PTPRR EPHB6 CD80 MED14 MED1 PPARA CELSR2 NCAM1 RYK CD86 Atlas (TCGA) datasets across 11 different cancer types, with data PPARG STRA6 EPNA3 LRP2 EFNB2 INTS6 CD28 PIGR ESRRB involving mRNA, microRNA, protein, and DNA methylation. NR4A2 THRAP3 TFRC GRM5 CD79B FLT1 ATP6AP2 NTRK1 INSRR NR3C1 XPR1 While some differential expression patterns associated with FCGR2C KDR ITGB1 CD79A CD3G AMOT ITGA4 IL2RA INSR PTPRC metastasis may be shared across multiple cancer types, each NR2F2 CD4 FZD4 DDR2 CXCR5 CD36 CD46 ITGAV ITGB6 VTN one also shows a metastasis signature that is distinct. When DLG1 CXCR4 CD1D IFNAR1 CALM3 GRM7 CNR1 FZD5 CD55 HCRTR1 combining TCGA data with that from multiple independent ADRB1 GABRR1 CSF1R NPC1 CR2 GABRR2 F2R F2 KCNQ5 CD47 LIFR ANTXR2 MET CD97 GP1BA fi LRP6 CR1 P2RX2 ABCC9 IL6ST pro ling datasets of metastatic tumors, the resulting catalog of FLT4 OSMR PTPRH P2RX4 KCNJ8 CUL5 GHR PTPRB gene-level alterations, according to cancer type, provides a Higher expression in metastasis versus primary for given cancer type BRCA CESC CRC ESCA HNSC PAAD PCPG PRAD SARC SKCM THCA resource for future studies. -

Supplementary Information
Osa et al Supplementary Information Clinical implications of monitoring nivolumab immunokinetics in previously treated non– small cell lung cancer patients Akio Osa, Takeshi Uenami, Shohei Koyama, Kosuke Fujimoto, Daisuke Okuzaki, Takayuki Takimoto, Haruhiko Hirata, Yukihiro Yano, Soichiro Yokota, Yuhei Kinehara, Yujiro Naito, Tomoyuki Otsuka, Masaki Kanazu, Muneyoshi Kuroyama, Masanari Hamaguchi, Taro Koba, Yu Futami, Mikako Ishijima, Yasuhiko Suga, Yuki Akazawa, Hirotomo Machiyama, Kota Iwahori, Hyota Takamatsu, Izumi Nagatomo, Yoshito Takeda, Hiroshi Kida, Esra A. Akbay, Peter S. Hammerman, Kwok-kin Wong, Glenn Dranoff, Masahide Mori, Takashi Kijima, Atsushi Kumanogoh Supplemental Figures 1 – 8 1 Osa et al Supplemental Figure 1. The frequency of nivolumab-bound T cells was maintained in patients who continued treatment. Nivolumab binding in CD8 and CD4 T cells was analyzed at two follow-up points, as indicated, in fresh peripheral blood from three representative cases from protocol 1 that continued treatment. 2 Osa et al Supplemental Figure 2. Long-term follow-up of nivolumab binding to T cells from fresh whole blood. Nivolumab binding was followed up in fresh peripheral blood from an additional case, Pt.7. 3 Osa et al Supplemental Figure 3. Long-term duration of nivolumab binding is due to sustained circulation of residual nivolumab in plasma. (A) PBMCs acquired from Pt.8 and 9 at pretreatment (pre PBMCs) and after a single dose (post 1 PBMCs) were cultured in regular medium without nivolumab (top and middle). Pre PBMCs were also incubated with 10 µg/ml nivolumab in vitro before the cultures were started (bottom). Nivolumab binding status was monitored at the indicated time points. -

Supplementary Data, Ms Iring Et Al. Re-Revised
Supplementary Data András Iring et al., “Shear stress-induced endothelial adrenomedullin signaling regulates vascular tone and blood pressure” Supplementary Tables Supplementary Table 1. Target sequences of siRNAs used in the siRNA screen (Fig. 4A). Gene Target sequence (5´-3´) ADORA2A CGGAACAGCTCCCAGGTCT ADORA2A GCTGTTAGATCCTCCATGT ADORA2A GGCTTTCCACGGGTTCAGA ADORA2B GAGACTTCCGCTACACTTT ADORA2B GAGCTCATGGATCACTCAA ADORA2B GATGCAGCCACGAACGTGA ADRB1 CAGATCTGGTCATGGGTCT ADRB1 GTGTCATCGCCCTGGACCA ADRB1 CCATCTCGGCGCTGGTGTC ADRB2 CAAGTTCTACTTGAAGGAA ADRB2 CAACTTCTGGTGTGAGTTT ADRB2 GTCATCACAGCCATTGCCA CALCRL GATCAGTTCTGATACGCAA CALCRL GATACTCTCCGTAGTGCAT CALCRL GATTTATGATTTACCTATA CCRL1 GTATGAAGTGATCTGTATA CCRL1 GCTACTTCATCACGGCAAA CCRL1 GCATCAAACATCTGCATTT CCRL2 GACCCTACAATATTGTACT CCRL2 GCTTCTTTACCGGACTTCA CCRL2 CCTGTTGCTCTACTCCATA CELSR1 CTATGAGGAGAATCGAGTA CELSR1 GACTGAAGGTCCAGACGCA CELSR1 CCAACATCGCCACGCTGAA CELSR3 CCTTTGTAACCAGAGAGAT CELSR3 CAGCTTATGATCCAGATGT CELSR3 GCAATACCGGGAGACGCTT CXCR7 GCATGAGTGTGGATCGCTA CXCR7 GCTACGACACGCACTGCTA CXCR7 CTTTGGAGCAGAATGCCAA 2 ELTD1 CTCTTCTAATTCAACTCTT ELTD1 CAAGTTTATTACTAATGAT ELTD1 GTACCATACAGCTATAGTA FZD1 GTAACCAATGCCAAACTTT FZD1 GATTAGCCACCGAAATAAA FZD1 CAGTGTTCCGCCGAGCTCA FZD2 CGCTTTGCGCGCCTCTGGA FZD2 GACATGCAGCGCTTCCGCT FZD2 CGCACTACACGCCGCGCAT FZD4 GTATGTGCTATAATATTTA FZD4 CCATTGTCATCTTGATTAT FZD4 CCAACATGGCAGTGGAAAT FZD5 GGATTTAAGGCCCAGTTTA FZD5 GACCATAACACACTTGCTT FZD5 CAAGTGATCCTGGGAAAGA FZD6 GCATTGTATCTCTTATGTA FZD6 GTGCTTACTGAGTGTCCAA FZD6 CCAATTACTGTTCCCAGAT FZD8 CCATCTGCCTAGAGGACTA -

FZD4 Gene Frizzled Class Receptor 4
FZD4 gene frizzled class receptor 4 Normal Function The FZD4 gene provides instructions for making a protein called frizzled-4. This protein is embedded in the outer membrane of many types of cells, where it is involved in transmitting chemical signals from outside the cell to the cell's nucleus. Specifically, frizzled-4 participates in the Wnt signaling pathway, a series of steps that affect the way cells and tissues develop. Wnt signaling is important for cell division (proliferation), attachment of cells to one another (adhesion), cell movement (migration), and many other cellular activities. Studies suggest that, at the cell surface, the frizzled-4 protein interacts with a protein called norrin (produced from the NDP gene). The two proteins fit together like a key in a lock. Researchers suspect that when norrin attaches (binds) to frizzled-4, it initiates a multi-step process that regulates the activity of certain genes. During early development, signaling by norrin and frizzled-4 plays a critical role in the specialization of cells in the retina, which is the light-sensing tissue at the back of the eye. This signaling pathway is also involved in the establishment of a blood supply to the retina and the inner ear. Health Conditions Related to Genetic Changes Familial exudative vitreoretinopathy More than 20 mutations in the FZD4 gene have been identified in people with an eye disorder called familial exudative vitreoretinopathy. Some of these mutations change single protein building blocks (amino acids) in frizzled-4, while others insert or delete genetic material in the FZD4 gene. Most FZD4 mutations reduce the amount of frizzled- 4 that is produced within cells. -

WNT Signalling in Chronic Lung Diseases
Thorax Online First, published on April 17, 2017 as 10.1136/thoraxjnl-2016-209753 State of the art review ‘WNT-er is coming’: WNT signalling in chronic lung Thorax: first published as 10.1136/thoraxjnl-2016-209753 on 17 April 2017. Downloaded from diseases H A Baarsma,1 M Königshoff1,2 1Comprehensive Pneumology ABSTRACT involved in the phosphorylation and subsequent Center, Helmholtz Center Chronic lung diseases represent a major public health degradation of β-catenin. Binding of a specific WNT Munich, Ludwig Maximilians University Munich, University problem with only limited therapeutic options. An ligand (eg, WNT-3A) to one of the Frizzled recep- Hospital Grosshadern, Member important unmet need is to identify compounds and tors (FZD1 through FZD10) and subsequent activa- of the German Center for Lung drugs that target key molecular pathways involved in the tion of the low-density lipoprotein receptor-related Research (DZL), Munich, pathogenesis of chronic lung diseases. Over the last proteins 5 and 6 (LRP5/6) co-receptors triggers an Germany 2 decade, there has been extensive interest in investigating intracellular signalling cascade, which results in Division of Pulmonary ‘β ’ Sciences and Critical Care Wingless/integrase-1 (WNT) signalling pathways; and inactivation of the -catenin destruction complex . Medicine, Department of WNT signal alterations have been linked to pulmonary Hence, cytosolic β-catenin can accumulate, translo- Medicine, University of disease pathogenesis and progression. Here, we cate to the nucleus and, in association with T cell Colorado School of Medicine, comprehensively review the cumulative evidence for WNT factor/lymphoid enhancer factor-1 (TCF/LEF) Aurora, Colorado, USA pathway alterations in chronic lung pathologies, including family of transcription factors, induce specific gene 1 Correspondence to idiopathic pulmonary fibrosis, pulmonary arterial expression (figure 1). -

Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 12-2013 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Medical Cell Biology Commons, and the Medical Molecular Biology Commons Recommended Citation Bogard, Amy Sue , "Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells" (2013). Theses and Dissertations (ETD). Paper 330. http://dx.doi.org/10.21007/etd.cghs.2013.0029. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Document Type Dissertation Degree Name Doctor of Philosophy (PhD) Program Biomedical Sciences Track Molecular Therapeutics and Cell Signaling Research Advisor Rennolds Ostrom, Ph.D. Committee Elizabeth Fitzpatrick, Ph.D. Edwards Park, Ph.D. Steven Tavalin, Ph.D. Christopher Waters, Ph.D. DOI 10.21007/etd.cghs.2013.0029 Comments Six month embargo expired June 2014 This dissertation is available at UTHSC Digital Commons: https://dc.uthsc.edu/dissertations/330 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells A Dissertation Presented for The Graduate Studies Council The University of Tennessee Health Science Center In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy From The University of Tennessee By Amy Sue Bogard December 2013 Copyright © 2013 by Amy Sue Bogard. -
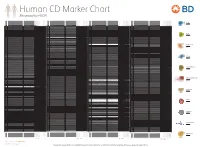
Reviewed by HLDA1
Human CD Marker Chart Reviewed by HLDA1 T Cell Key Markers CD3 CD4 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD8 CD1a R4, T6, Leu6, HTA1 b-2-Microglobulin, CD74 + + + – + – – – CD74 DHLAG, HLADG, Ia-g, li, invariant chain HLA-DR, CD44 + + + + + + CD158g KIR2DS5 + + CD248 TEM1, Endosialin, CD164L1, MGC119478, MGC119479 Collagen I/IV Fibronectin + ST6GAL1, MGC48859, SIAT1, ST6GALL, ST6N, ST6 b-Galactosamide a-2,6-sialyl- CD1b R1, T6m Leu6 b-2-Microglobulin + + + – + – – – CD75 CD22 CD158h KIR2DS1, p50.1 HLA-C + + CD249 APA, gp160, EAP, ENPEP + + tranferase, Sialo-masked lactosamine, Carbohydrate of a2,6 sialyltransferase + – – + – – + – – CD1c M241, R7, T6, Leu6, BDCA1 b-2-Microglobulin + + + – + – – – CD75S a2,6 Sialylated lactosamine CD22 (proposed) + + – – + + – + + + CD158i KIR2DS4, p50.3 HLA-C + – + CD252 TNFSF4,