ITPE Sample.Fm
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparison of Etoricoxib and Indomethacin for the Treatment of Experimental Periodontitis in Rats
Brazilian Journal of Medical and Biological Research (2007) 40: 117-125 Etoricoxib in experimental periodontitis 117 ISSN 0100-879X Comparison of etoricoxib and indomethacin for the treatment of experimental periodontitis in rats M.C.F. Azoubel1, 1Departamento de Fisiologia e Farmacologia, A.M.A. Menezes1, 2Departamento de Morfologia, Faculdade de Medicina, D. Bezerra1, R.B. Oriá2, Universidade Federal do Ceará, Fortaleza, CE, Brasil R.A. Ribeiro1 and G.A.C. Brito2 Abstract Correspondence We investigated the effect of etoricoxib, a selective cyclooxygenase- Key words G.A.C. Brito 2 inhibitor, and indomethacin, a non-selective cyclooxygenase inhib- • Alveolar bone loss Departamento de Fisiologia itor, on experimental periodontitis, and compared their gastrointesti- • Inflammation e Farmacologia nal side effects. A ligature was placed around the second upper left • Periodontitis Faculdade de Medicina, UFC molars of female Wistar rats (160 to 200 g). Animals (6 per group) • Cyclooxygenase inhibitors Rua Coronel Nunes de Melo, 1127 • were treated daily with oral doses of 3 or 9 mg/kg etoricoxib, 5 mg/kg Etoricoxib 60430-270 Fortaleza, CE • Indomethacin Brasil indomethacin, or 0.2 mL saline, starting 5 days after the induction of Fax: +55-85-3366-8333 periodontitis, when bone resorption was detected, until the sacrifice E-mail: [email protected] on the 11th day. The weight and survival rate were monitored. Alveolar bone loss (ABL) was measured as the sum of distances Research supported by CNPq and between the cusp tips and the alveolar bone. The gastric mucosa was Fundação Cearense de Pesquisa e examined macroscopically and the periodontium and gastric and Cultura (FUNCAP). -

(FNE) and Nasal Endoscopy in Ireland During COVID-19 Pandemic Rev 1
Royal College of Surgeons in Ireland Coláiste Ríoga na Máinleá in Éirinn Interim Clinical Guidance on Flexible Nasendoscopy (FNE) and Nasal Endoscopy in Ireland during COVID-19 pandemic Rev 1 INTERIM CLINICAL GUIDANCE ON FLEXIBLE NASENDOSCOPY (FNE) AND NASAL ENDOSCOPY IN IRELAND DURING COVID-19 PANDEMIC Rev 1 INTERIM CLINICAL GUIDANCE ON FLEXIBLE NASENDOSCOPY (FNE) AND NASAL ENDOSCOPY IN IRELAND DURING COVID-19 PANDEMIC Table of Contents 1. Overview ............................................................................................................................................................................. 2 2. Purpose ............................................................................................................................................................................... 2 3. Authorship ......................................................................................................................................................................... 2 4. Target Audience .............................................................................................................................................................. 2 5. Introduction ....................................................................................................................................................................... 2 6. Risk of infection associated with FNE .................................................................................................................. 2 7. Aerosol Generating Procedures -

RADIOGRAPHY to Prepare Individuals to Become Registered Radiologic Technologists
RADIOGRAPHY To prepare individuals to become Registered Radiologic Technologists. THE WORKFORCE CAPITAL This two-year, advanced medical program trains students in radiography. Radiography uses radiation to produce images of tissues, organs, bones and vessels of the body. The radiographer is an essential member of the health care team who works in a variety of settings. Responsibili- ties include accurately positioning the patient, producing quality diagnostic images, maintaining equipment and keeping computerized records. This certificate program of specialized training focuses on each of these responsibilities. Graduates are eligible to apply for the national credential examination to become a registered technologist in radiography, RT(R). Contact Student Services for current tuition rates and enrollment information. 580.242.2750 Mission, Goals, and Student Learning Outcomes Program Effectiveness Data Radiography Program Guidelines (Policies and Procedures) “The programs at Autry prepare you for the workforce with no extra training needed after graduation.” – Kenedy S. autrytech.edu ENDLESS POSSIBILITIES 1201 West Willow | Enid, Oklahoma, 73703 | 580.242.2750 | autrytech.edu COURSE LENGTH Twenty-four-month daytime program î August-July î Monday-Friday Academic hours: 8:15am-3:45pm Clinical hours: Eight-hour shifts between 7am-5pm with some ADMISSION PROCEDURES evening assignments required Applicants should contact Student Services at Autry Technology Center to request an information/application packet. Applicants who have a completed application on file and who have met entrance requirements will be considered for the program. Meeting ADULT IN-DISTRICT COSTS the requirements does not guarantee admission to the program. Qualified applicants will be contacted for an interview, and class Year One: $2732 (Additional cost of books and supplies approx: $1820) selection will be determined by the admissions committee. -

Resection Arthroplasty for Failed Shoulder Arthroplasty
J Shoulder Elbow Surg (2013) 22, 247-252 www.elsevier.com/locate/ymse Resection arthroplasty for failed shoulder arthroplasty Stephanie J. Muh, MDa, Jonathan J. Streit, MDb, Christopher J. Lenarz, MDa, Christopher McCrum, BSc, John Paul Wanner, BSa, Yousef Shishani, MDa, Claudio Moraga, MDd, Robert J. Nowinski, DOe, T. Bradley Edwards, MDf, Jon J.P. Warner, MDg, Gilles Walch, MDh, Reuben Gobezie, MDi,* aCase Shoulder and Elbow Service, Case Western Reserve University School of Medicine, University Hospitals of Cleveland, Cleveland, OH, USA bDepartment of Orthopaedics, Case Western Reserve University School of Medicine, University Hospitals of Cleveland, Cleveland, OH, USA cCase Western Reserve University School of Medicine, Cleveland, OH, USA dDepartment of Orthopedic Surgery, Clinica Alemana Santiago, Santiago, Chile eOrthoNeuro, New Albany, OH, USA fFondren Orthopedic Group, Houston, TX, USA gHarvard Shoulder Service, Massachusetts General Hospital, Boston, MA, USA hCentre Orthopedique Santy, Shoulder Unit, Lyon, France iThe Cleveland Shoulder Institute, University Hospitals of Cleveland, Cleveland, OH, USA Background: As shoulder arthroplasty becomes more common, the number of failed arthroplasties requiring revision is expected to increase. When revision arthroplasty is not feasible, resection arthroplasty has been used in an attempt to restore function and relieve pain. Although outcomes data for resection arthroplasty exist, studies comparing the outcomes after the removal of different primary shoulder arthro- plasties have been limited. Materials and methods: This was a retrospective multicenter review of 26 patients who underwent resection arthroplasty for failure of a primary arthroplasty at a mean follow-up of 41.8 months (range, 12-130 months). Resection arthroplasty was performed for 6 failed total shoulder arthroplasties (TSAs), 7 failed hemiarthro- plasties, and 13 failed reverse TSAs. -

Home Care After Sleep Surgery-Uvulopalatopharyngoplasty (UP3) And/Or Tonsillectomy
Home Care after Sleep Surgery-Uvulopalatopharyngoplasty (UP3) and/or Tonsillectomy The above surgeries are all performed on patients to help relieve or lessen the symptoms of sleep apnea. All address the palate, or the upper part of your throat. General Information You may lack energy for several days, and may also be restless at night. This will improve over the next 10 to 14 days. It is quite common to feel progressively worse during the first five to six days after surgery. You may also become constipated during this time for three reasons: you will not be eating a regular diet, you will be taking pain medications, and you may be less active. Wound Care All of the above surgeries are performed within the mouth on the upper throat. No external incisions are made, all are internal. Depending on the surgery, you may feel and/or see some suture on your palate (upper throat). This is normal and will dissolve over the next two weeks. No specific wound care is necessary for these procedures. Diet It is important for you to drink plenty of fluids after surgery. Drink every hour while awake. A soft diet is recommended for the first 14 days (anything that you may eat without teeth constitutes as a soft diet). Avoid hot liquids/solids. It is alright if you don’t feel like eating much, as long as you drink lots of fluids. Signs that you need to drink more are when the urine is darker in color (urine should be pale yellow). A high fever that persists may also be a sign that you are not taking in enough fluids. -

2017 American College of Rheumatology/American Association
Arthritis Care & Research Vol. 69, No. 8, August 2017, pp 1111–1124 DOI 10.1002/acr.23274 VC 2017, American College of Rheumatology SPECIAL ARTICLE 2017 American College of Rheumatology/ American Association of Hip and Knee Surgeons Guideline for the Perioperative Management of Antirheumatic Medication in Patients With Rheumatic Diseases Undergoing Elective Total Hip or Total Knee Arthroplasty SUSAN M. GOODMAN,1 BRYAN SPRINGER,2 GORDON GUYATT,3 MATTHEW P. ABDEL,4 VINOD DASA,5 MICHAEL GEORGE,6 ORA GEWURZ-SINGER,7 JON T. GILES,8 BEVERLY JOHNSON,9 STEVE LEE,10 LISA A. MANDL,1 MICHAEL A. MONT,11 PETER SCULCO,1 SCOTT SPORER,12 LOUIS STRYKER,13 MARAT TURGUNBAEV,14 BARRY BRAUSE,1 ANTONIA F. CHEN,15 JEREMY GILILLAND,16 MARK GOODMAN,17 ARLENE HURLEY-ROSENBLATT,18 KYRIAKOS KIROU,1 ELENA LOSINA,19 RONALD MacKENZIE,1 KALEB MICHAUD,20 TED MIKULS,21 LINDA RUSSELL,1 22 14 23 17 ALEXANDER SAH, AMY S. MILLER, JASVINDER A. SINGH, AND ADOLPH YATES Guidelines and recommendations developed and/or endorsed by the American College of Rheumatology (ACR) are intended to provide guidance for particular patterns of practice and not to dictate the care of a particular patient. The ACR considers adherence to the recommendations within this guideline to be volun- tary, with the ultimate determination regarding their application to be made by the physician in light of each patient’s individual circumstances. Guidelines and recommendations are intended to promote benefi- cial or desirable outcomes but cannot guarantee any specific outcome. Guidelines and recommendations developed and endorsed by the ACR are subject to periodic revision as warranted by the evolution of medi- cal knowledge, technology, and practice. -

ACR–SPR-STR Practice Parameter for the Performance of Chest Radiography
The American College of Radiology, with more than 30,000 members, is the principal organization of radiologists, radiation oncologists, and clinical medical physicists in the United States. The College is a nonprofit professional society whose primary purposes are to advance the science of radiology, improve radiologic services to the patient, study the socioeconomic aspects of the practice of radiology, and encourage continuing education for radiologists, radiation oncologists, medical physicists, and persons practicing in allied professional fields. The American College of Radiology will periodically define new practice parameters and technical standards for radiologic practice to help advance the science of radiology and to improve the quality of service to patients throughout the United States. Existing practice parameters and technical standards will be reviewed for revision or renewal, as appropriate, on their fifth anniversary or sooner, if indicated. Each practice parameter and technical standard, representing a policy statement by the College, has undergone a thorough consensus process in which it has been subjected to extensive review and approval. The practice parameters and technical standards recognize that the safe and effective use of diagnostic and therapeutic radiology requires specific training, skills, and techniques, as described in each document. Reproduction or modification of the published practice parameter and technical standard by those entities not providing these services is not authorized. Revised 2017 (Resolution 2)* ACR–SPR–STR PRACTICE PARAMETER FOR THE PERFORMANCE OF CHEST RADIOGRAPHY PREAMBLE This document is an educational tool designed to assist practitioners in providing appropriate radiologic care for patients. Practice Parameters and Technical Standards are not inflexible rules or requirements of practice and are not intended, nor should they be used, to establish a legal standard of care1. -
The Importance of Orofacial Myofunctional Therapy Before and After CO2 Laser Frenectomy in Achieving Optimal Orofacial Function
LASERfocus The Importance of Orofacial Myofunctional Therapy Before and After CO2 Laser Frenectomy in Achieving Optimal Orofacial Function by Karen M. Wuertz, DDS, ABCDSM, DABLS, FOM, and Brooke Pettus, RDH, BSDH, COMS Frenectomy Methods ing, speaking, and breathing patterns may be Frenotomies performed with a scalpel or scissors can be accompanied by caused by incorrect oral posture and oral re- significant bleeding, obscuring the surgical field making it difficult to ensure strictions. Therefore, in the authors’ opinion, if the restriction has been completely removed. Because of the increased risk the removal of oral restrictions is necessary to of early primary closure of the site, postoperative active wound care is es- attain optimal orofacial function, and must be sential to reduce the risk of potential scarring. To properly restore and main- combined with regular pre- and post-frenecto- tain optimum function, active wound care should be implemented as soon my orofacial myofunctional therapy (OMT).1,4 as possible. However, if sutures are placed, the active wound care may be OMT helps re-educate the tongue and orofa- delayed so as not to cause early tearing of tissue. Due to the contact nature of cial muscles during movement and at rest to conventional procedure, there is a certain potential for infection; in addition, create new neuromuscular patterns for proper higher levels of postoperative pain and discomfort have been reported.1,2 Elec- oral function, including chewing, swallowing, trocautery and a hot glass tip of dental diodes may leave a fairly substantial speaking, and breathing.5,6 Camacho et al.7 zone of thermal tissue change3 and may result in delayed healing. -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

Estimation of the Collective Effective Dose to the Population from Medical X-Ray Examinations in Finland
Estimation of the collective effective dose to the population from medical x-ray examinations in Finland Petra Tenkanen-Rautakoskia, Hannu Järvinena, Ritva Blya aRadiation and Nuclear Safety Authority (STUK), PL 14, 00880 Helsinki, Finland Abstract. The collective effective dose to the population from all x-ray examinations in Finland in 2005 was estimated. The numbers of x-ray examinations were collected by a questionnaire to the health care units (response rate 100 %). The effective doses in plain radiography were calculated using a Monte Carlo based program (PCXMC), as average values for selected health care units. For computed tomography (CT), weighted dose length product (DLPw) in a standard phantom was measured for routine CT protocols of four body regions, for 80 % of CT scanners including all types. The effective doses were calculated from DPLw values using published conversion factors. For contrast-enhanced radiology and interventional radiology, the effective dose was estimated mainly by using published DAP values and conversion factors for given body regions. About 733 examinations per 1000 inhabitants (excluding dental) were made in 2005, slightly less than in 2000. The proportions of plain radiography, computed tomography, contrast-enhanced radiography and interventional procedures were about 92, 7, 1 and 1 %, respectively. From 2000, the frequencies (number of examinations per 1000 inhabitants) of plain radiography and contrast-enhanced radiography have decreased about 8 and 33 %, respectively, while the frequencies of CT and interventional radiology have increased about 28 and 38 %, respectively. The population dose from all x-ray examinations is about 0,43 mSv per person (in 1997 0,5 mSv). -
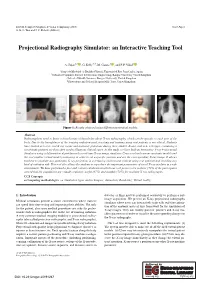
Projectional Radiography Simulator: an Interactive Teaching Tool
EG UK Computer Graphics & Visual Computing (2019) Short Paper G. K. L. Tam and J. C. Roberts (Editors) Projectional Radiography Simulator: an Interactive Teaching Tool A. Sujar1,2 , G. Kelly3,4, M. García1 , and F. P. Vidal2 1Grupo de Modelado y Realidad Virtual, Universidad Rey Juan Carlos, Spain 2School of Computer Science & Electronic Engineering, Bangor University United Kingdom 3School of Health Sciences, Bangor University, United Kingdom 4Shrewsbury and Telford Hospital NHS Trust, United Kingdom Figure 1: Results obtained using different anatomical models. Abstract Radiographers need to know a broad range of knowledge about X-ray radiography, which can be specific to each part of the body. Due to the harmfulness of the ionising radiation used, teaching and training using real patients is not ethical. Students have limited access to real X-ray rooms and anatomic phantoms during their studies. Books, and now web apps, containing a set of static pictures are then often used to illustrate clinical cases. In this study, we have built an Interactive X-ray Projectional Simulator using a deformation algorithm with a real-time X-ray image simulator. Users can load various anatomic models and the tool enables virtual model positioning in order to set a specific position and see the corresponding X-ray image. It allows teachers to simulate any particular X-ray projection in a lecturing environment without using real patients and avoiding any kind of radiation risk. This tool also allows the students to reproduce the important parameters of a real X-ray machine in a safe environment. We have performed a face and content validation in which our tool proves to be realistic (72% of the participants agreed that the simulations are visually realistic), useful (67%) and suitable (78%) for teaching X-ray radiography. -

The Cementum: Its Role in Periodontal Health and Disease*
THE JOURNAL OF PERIODONTOLOGY JULY, NINETEEN HUNDRED SIXTY ONE The Cementum: Its Role In Periodontal Health and Disease* by DONALD A. KERR, D.D.S., M.S.,** Ann Arbor, Michigan HE cementum is a specialized calcified tissue of mesenchymal origin which provides for the attachment of the periodontal fibers to the surface of the Troot. It consists of 45 to 50 per cent inorganic material and 50 to 55 per cent organic material with the inorganic material in a hydroxyl apatite structure. The primary cementum is formed initially by appositional growth from the dental sac and later from the periodontal membrane under the influence of cementoblasts. It is formed in laminated layers with the incorporation of Sharpey's fibers into a fibrillar matrix which undergoes calcification. Cementum deposition is a Continuous process throughout life with new cementum being deposited over the old cemental surface. Cementum is formed by the organiza• tion of collagen fibrils which are cemented together by a matrix produced by the polymerization of mucopolysaccharides. This material is designated as cementoid and becomes mature cementum upon calcification. The significance of the continuous deposition of cementum has received various interpretations. 1. Continuous deposition of cementum is necessary for the reattachment of periodontal fibers which have been destroyed or which require reorientation due to change in position of teeth. It is logical that there should be a continuous deposition of cementum because it is doubtful that the initial fibers are retained throughout the life of the tooth, and therefore new fibers must be continually formed and attached by new cementum.