Orkney Winter Plan 2020/21
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
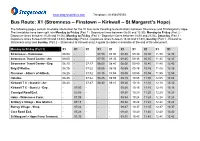
Bus Route X1
www.stagecoachbus.com Telephone: 01856870555. Bus Route: X1 (Stromness – Finstown – Kirkwall – St Margaret’s Hope) The following pages contain timetable information for the X1 bus route travelling to destinations between Stromness and St Margaret’s Hope. The timetables have been split into Monday to Friday (Part 1 - Departure times between 06:00 and 12:30), Monday to Friday (Part 2 - Departure times between 13:20 and 18:00), Monday to Friday (Part 3 - Departure times between 18:30 and 21:05), Saturday (Part 1 - Departure times between 07:00 and 13:30), Saturday (Part 2 - Departure times between 14:30 and 01:30), Sunday (Part 1 - Kirkwall to Stromness only) and Sunday (Part 2 – Stromness to Kirkwall only) A guide to codes is available at the end of this document. Monday to Friday (Part 1) X1 X1 X1 X1 X1 X1 X1 X1 X1 X1 Stromness - Hamnavoe. 06:00 - - 07:50 08:30 08:40 09:30 10:30 11:30 12:30 Stromness Travel Centre - Arr. 06:05 - - 07:55 08:35 08:45 09:35 10:35 11:35 12:35 Stromness Travel Centre - Dep. 06:10 - 07:17 08:00 08:40 08:50 09:40 10:40 11:40 12:40 Brig O’Waithe. 06:15 - 07:22 08:05 08:45 08:55 09:45 10:45 11:45 12:45 Finstown - Allan’s of Gillock. 06:25 - 07:32 08:15 08:55 09:05 09:55 10:55 11:55 12:55 Hatston. 06:35 - 07:42 08:25 09:05 09:15 10:05 11:05 12:05 13:05 Kirkwall T C - Stand 2 - Arr. -

NEWSLETTER of the ORKNEY FAMILY HISTORY SOCIETY No 79 September 2016
SIB FOLK NEWS NEWSLETTER OF THE ORKNEY FAMILY HISTORY SOCIETY No 79 September 2016 GRAPHICS JOHN SINCLAIR 2 NEWSLETTER OF THE ORKNEY FAMILY HISTORY SOCIETY Issue No 79 September 2016 ORKNEY FAMILY HISTORY NEWSLETTER No 79 SEPTEMBER 2016 COVER SIB HIGHLIGHTS PAGE 2 From the Chair PAGES 3,4,5 more reminiscences from Jackie Brown Pages 6 & 7 Peter's very important ancestor From PAGES 8,9,10 Norman Windwick the Chair recalls his childhood at the Toc H Welcome to the September issue of the Sib Folk News at the end of a PAGE 11 summer of lovely weather and a very busy time in the office. In Orkney as a Tumbledown 'Gyrehouse' Stenness whole, we must have had record numbers of tourists this year with over 100 cruise ships including Orkney in their itinerary plus all the holidaymakers who PAGES 12 & 13 visited our islands. The Kirkwall Shops. A stroll down The Family History Society had a table in the exhibition hall at the Vintage memory lane Rally in August and it was good to see and have a chat with our members and welcome some new ones as well. Remember, we look forward to seeing PAGES 14 & 15 you in the office if you get stuck with your research or if you just want to say Captain James 'hello'. Renton Waters The website is being updated with more interesting and helpful resources PAGES 16 & 17 Mandy Thomson bitten so don't forget to check out www.orkneyfhs.co.uk and you will be amazed by the Orkney at the amount of information freely available to our members. -

Service St Margaret's Hope (Ferry Terminal) - Stromness (Hamnavoe) X1 Monday - Friday (Not Bank Holidays)
Service St Margaret's Hope (Ferry Terminal) - Stromness (Hamnavoe) X1 Monday - Friday (not Bank Holidays) Operated by: OC Stagecoach Highlands Timetable valid from 5 Sep 2021 until further notice Service: X1 X1 X1 X1 X1 X1 X1 X1 X1 X1 X1 Notes: XPrd1 Operator: OC OC OC OC OC OC OC OC OC OC OC St Margarets Hope, Ferry terminal Depart: .... .... .... .... .... .... 07:37 .... .... 08:47 09:47 Burray, Shop .... .... .... .... .... .... 07:45 .... .... 08:55 09:55 St Marys, Graeme Park .... .... .... .... .... .... 07:54 .... .... 09:04 10:04 Kirkwall, Hospital Entrance .... .... 06:21 .... .... 07:45 08:05 .... .... 09:15 10:15 Kirkwall, Travel Centre (Stand 2) Arrive: .... .... 06:24 .... .... 07:48 08:08 .... .... 09:18 10:18 Kirkwall, Travel Centre (Stand 2) Depart: 05:05 06:05 06:25 06:55 .... 07:50 .... 08:50 .... 09:20 10:20 Kirkwall, Hatston Bus Garage 05:10 06:10 06:30 07:00 07:10 07:55 .... 08:55 09:00 09:25 10:25 Finstown, Allan's of Gillock 05:20 06:20 06:40 07:10 07:20 08:05 .... 09:05 09:10 09:35 10:35 Stenness, Garage 05:27 06:27 06:47 07:17 07:27 08:12 .... 09:12 09:17 09:42 10:42 Stromness, Travel Centre Arrive: 05:35 .... 06:55 07:25 .... 08:20 .... 09:20 09:30 09:50 10:50 Stromness, Travel Centre Depart: 05:36 .... 06:56 07:26 .... 08:22 .... 09:22 .... 09:52 10:52 Stromness, Hamnavoe Estate Arrive: 05:39 06:35 06:59 07:29 07:35 08:25 ... -

FOI) the Balfour, Foreland Road, Kirkwall, Orkney KW15 1NZ
Freedom of Information (FOI) The Balfour, Foreland Road, Kirkwall, Orkney KW15 1NZ www.ohb.scot.nhs.uk RE: Freedom of Information Request 202021 / 055 – Falls Data Your Query Date of Request June 2020 1. I would like to request any data you hold on falls from the last 5 years. a) I am looking for the total number of falls sorted by hospital from the last 5 years? b) I am looking for the total number of falls sorted by ward from the last 2 years? 2. I would also like to request all email addresses for ward managers and falls leads/groups within the trust? 3. On average how much does falls cost the trust per year? Clarification Question 2 and 3 are an expansion of question 1. I hope this clarifies for you. In addition please could the data be sorted by the last 5 full calendar years and please include any data that the trust hold for this year too. Response Please be advised that NHS Orkney is a small remote and rural health board which operates one hospital – the Balfour. 1. a) Please note the methodology for measuring falls locally has changed over time. The methodology used for collecting this data is different from previous years. The data provided excludes any falls as a result of ‘assisted lowering’ which were counted in previous years. The total of excluded falls using the new methodology is 4 for 2019 and 3 for 2020. Year 2015 2016 2017 2018 2019 2020 Number of 63 82 113 88 103 *42 patient falls recorded *As at 25/06/2020. -

Ferry Timetables
1768 Appendix 1. www.orkneyferries.co.uk GRAEMSAY AND HOY (MOANESS) EFFECTIVE FROM 24 SEPTEMBER 2018 UNTIL 4 MAY 2019 Our service from Stromness to Hoy/Graemsay is a PASSENGER ONLY service. Vehicles can be carried by prior arrangement to Graemsay on the advertised cargo sailings. Monday Tuesday Wednesday Thursday Friday Saturday Sunday Stromness dep 0745 0745 0745 0745 0745 0930 0930 Hoy (Moaness) dep 0810 0810 0810 0810 0810 1000 1000 Graemsay dep 0825 0825 0825 0825 0825 1015 1015 Stromness dep 1000 1000 1000 1000 1000 Hoy (Moaness) dep 1030 1030 1030 1030 1030 Graemsay dep 1045 1045 1045 1045 1045 Stromness dep 1200A 1200A 1200A Graemsay dep 1230A 1230A 1230A Hoy (Moaness) dep 1240A 1240A 1240A Stromness dep 1600 1600 1600 1600 1600 1600 1600 Graemsay dep 1615 1615 1615 1615 1615 1615 1615 Hoy (Moaness) dep 1630 1630 1630 1630 1630 1630 1630 Stromness dep 1745 1745 1745 1745 1745 Graemsay dep 1800 1800 1800 1800 1800 Hoy (Moaness) dep 1815 1815 1815 1815 1815 Stromness dep 2130 Graemsay dep 2145 Hoy (Moaness) dep 2200 A Cargo Sailings will have limitations on passenger numbers therefore booking is advisable. These sailings may be delayed due to cargo operations. Notes: 1. All enquires must be made through the Kirkwall Office. Telephone: 01856 872044. 2. Passengers are requested to be available for boarding 5 minutes before departure. 3. Monday cargo to be booked by 1600hrs on previous Friday otherwise all cargo must be booked before 1600hrs the day before sailing. Cargo must be delivered to Stromness Pier no later than 1100hrs on the day of sailing. -

Emergency Care Weekly Metadata
Publication Metadata (including revision details) Metadata Description Indicator Publication Weekly Update of Emergency Department Activity and Waiting title Times. Description This publication reports key statistics on attendances at Emergency Departments (ED) across Scotland. The information presented in the publication includes trends in the number of attendances and length of time patients spend in ED. Theme Health and Social Care Topic Emergency Care Format Webpage, Excel workbook and CSV. Data source(s) NHS Board aggregate submissions to PHS on Emergency Department Activity and Waiting Times. Date that data Tuesday of the week prior to publication are acquired Release date Every Tuesday Frequency Weekly Timeframe of New data for the week ending 9 days before publication (e.g. 16 data and April publication contains data for week ending 7 April) timeliness Continuity of 1) A&E discharge times at hospitals in NHS Lothian were not data accurately recorded up to November 2017. The Academy of Medical Royal Colleges was commissioned by Scottish Government to ascertain the causes for the data issues in NHS Lothian. The review findings were published 26 June 2018. 2) Since 3 March 2015, the Scottish Government (SG) has released Official Statistics weekly A&E activity and waiting times information for the EDs in Scotland, derived from aggregate information supplied by NHS Boards on the number of attendances and 4, 8, and 12 hour waits. PHS (formally ISD) took over this data collection for statistics covering the week ending 7 June 2015. 3) From 20 May 2018, Raigmore hospital in NHS Highland trialled a new patient flow system. As a consequence the accuracy of some patients’ waits may have been affected between this date and 4 July, however the total number of attendances remains correct. -
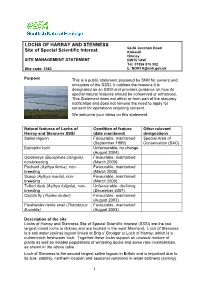
Lochs of Harray and Stenness Site of Special Scientific Interest (SSSI) Are the Two Largest Inland Lochs in Orkney and Are Located in the West Mainland
LOCHS OF HARRAY AND STENNESS 54-56 Junction Road Site of Special Scientific Interest Kirkwall Orkney SITE MANAGEMENT STATEMENT KW15 1AW Tel: 01856 875 302 Site code: 1083 E: [email protected] Purpose This is a public statement prepared by SNH for owners and occupiers of the SSSI. It outlines the reasons it is designated as an SSSI and provides guidance on how its special natural features should be conserved or enhanced. This Statement does not affect or form part of the statutory notification and does not remove the need to apply for consent for operations requiring consent. We welcome your views on this statement. Natural features of Lochs of Condition of feature Other relevant Harray and Stenness SSSI (date monitored) designations Saline lagoon Favourable, maintained Special Area of (September 1999) Conservation (SAC) Eutrophic loch Unfavourable, no change (August 2004) Goldeneye (Bucephala clangula), Favourable, maintained non-breeding (March 2000) Pochard (Aythya ferina), non- Favourable, maintained breeding (March 2000) Scaup (Aythya marila), non- Favourable, maintained breeding (March 2000) Tufted duck (Aythya fuligula), non- Unfavourable, declining breeding (December 2007) Caddis fly (Ylodes reuteri) Favourable, maintained (August 2003) Freshwater nerite snail (Theodoxus Favourable, maintained fluviatilis) (August 2003) Description of the site Lochs of Harray and Stenness Site of Special Scientific Interest (SSSI) are the two largest inland lochs in Orkney and are located in the west Mainland. Loch of Stenness is a salt water (saline) lagoon linked at Brig o’ Brodgar to Loch of Harray, which is a nutrient-rich freshwater loch. Together these lochs support an unusual mixture of plants as well as notable populations of wintering ducks and some rare invertebrates, as shown in the above table. -

The Kirk in the Garden of Evie
THE KIRK IN THE GARDEN OF EVIE A Thumbnail Sketch of the History of the Church in Evie Trevor G Hunt Minister of the linked Churches of Evie, Firth and Rendall, Orkney First Published by Evie Kirk Session Evie, Orkney. 1987 Republished 1996 ComPrint, Orkney 908056 Forward to the 1987 Publication This brief history was compiled for the centenary of the present Evie Church building and I am indebted to all who have helped me in this work. I am especially indebted to the Kirk’s present Session Clerk, William Wood of Aikerness, who furnished useful local information, searched through old Session Minutes, and compiled the list of ministers for Appendix 3. Alastair Marwick of Whitemire, Clerk to the Board, supplied a good deal of literature, obtained a copy of the Title Deeds, gained access to the “Kirk aboon the Hill”, and conducted a tour (even across fields in his car) to various sites. He also contributed valuable local information and I am grateful for all his support. Thanks are also due to Margaret Halcro of Lower Crowrar, Rendall, for information about her name sake, and to the Moars of Crook, Rendall, for other Halcro family details. And to Sheila Lyon (Hestwall, Sandwick), who contributed information about Margaret Halcro (of the seventeenth century!). TREVOR G HUNT Finstown Manse March 1987 Foreword to the 1996 Publication Nearly ten years on seemed a good time to make this history available again, and to use the advances in computer technology to improve its appearance and to make one or two minor corrections.. I was also anxious to include the text of the history as a page on the Evie, Firth and Rendall Churches’ Internet site for reference and, since revision was necessary to do this, it was an opportunity to republish in printed form. -

NHS Guidlines
NHSScotland Identity guidelines Identikit Introduction In December 2000, Susan Deacon MSP, In this publication, the Minister said: “The public relate to and recognise Minister for Health and Community Care, the NHS. They believe their care is launched ‘Our National Health: provided by a national health service and staff take pride in the fact that a plan for action, a plan for change’ they work for the NHS. Research tells us that the variety of differently which set out a clear direction for the NHS named NHS bodies confuses the in Scotland with the aims of improving public and alienates staff. As part of our proposals to rebuild the National people’s health and creating a 21st century Health Service we will promote a new identity for the NHS in Scotland.” health service. The guidelines that follow provide an essential design toolkit to establish “Alongside the changes in NHS this new identity. The guidelines cover signage, vehicles, uniforms, stationery, boardrooms, we will re-establish literature, forms and other items. The a national identity for the aim is to replace, over time, the array of existing identities within NHS NHS in Scotland.” organisations with the single NHS identity while avoiding wastage and unnecessary expenditure. Our National Health: a plan for action, a plan for change section 3/page 31 2 Contents Section 1 Our national identity 4 Exclusion zone 6 Minimum size 6 Section 2 Identity structure 7 Essential elements 9 Identity variants 10 Caring device 12 Positioning the identity 14 Other identities 15 Working in partnership 16 Section 3 Identities for ideas & initiatives 17 Initiatives 18 Section 4 NHSScotland typefaces 19 Stone Sans 20 Arial 24 Garamond 25 Times New Roman 26 Literature 27 Section 5 Colour 28 Using colour 29 Primary colours 30 Colour palette 31 Tints 32 Printing the identity 33 3 Section One Our national identity Together, the initials ‘NHS’ and the caring symbol form the foundations of our identity. -

A Warm Welcome to Dounby Community School
Parents & Carers Information Booklet 2020-21 CONTENTS Vision, Values and Aims ................................................................... 1 Quick Contact List ........................................................................... 2 About Our School ............................................................................. 3 School Staff ...................................................................................... 5 Managing Covid-19 in School .......................................................... 6 Keeping You Informed ..................................................................... 7 School Organisation ......................................................................... 8 School Calendar ................................................................................. 9 Being Absent ...................................................................................... 10 Daily Checklist ................................................................................... 10 Play and School Clubs ....................................................................... 14 Curriculum........................................................................................... 15 Religious Observance & Learning .................................................. 18 Working with Parents and Carers ................................................. 19 Pupil Council ........................................................................................ 21 Additional Learning Needs ............................................................ -

Prime Stock Show and Sale 2018
PRIME STOCK SHOW AND SALE 2018 Champion of our 2018 Prime Stock Show and sale was this tremendous Limousin x Heifer shown by Fraser Leslie Odinstone Shapinsay out of Livet Hustler. This Heifer won the Young Farmers Cattle section and went on to win the overall Championship. The Heifer weighed 650 kilos and sold for £2200 to Williamsons East Road Kirkwall (Pictured are Fraser Leslie and our Judge Mr D Buchan Auchtydore Farms Aberdeenshire) Reserve Champion was the Limousin Steer Shown by Balfour Baillie Sebay View Tankerness This Steer scaled 620 kilos and sold for £2000 to E Flett Butchers Stromness, purchased on their behalf by local livestock agent W S L Muir Upper Onston Stenness The Steer also won the cup for best beast opposite sex to the Champion. Champion pair of lambs was these Beltex x Texel’s scaling 52 kilos from Biggings Farm Ltd. They sold for £170 per head and were purchased by E Flett Butchers Stromness. Inga Kemp’s Texel cross Lamb won the Young Farmers Section, it weighed 58 kilos and realised £125 and was purchased by Dounby Butchers. Cattle Class Results Class 1 Light Steer 1st No 6 B Baillie Sebay View Tankerness £2000 E Flett Butcher Stromness 2nd No 3 T & J Leslie Quoymorhouse Shapinsay £1391.50 Craigie Butcher Brig Larder 3rd No 4 T & J Leslie Quoymorhouse Shapinsay £1417.50 Craigie Butcher Brig Larder Class 2 Heavy Steer 1st No 5 R & J Johnston Hewan Shapinsay £1430 Williamsons East Road Kirkwall 2nd No 1 J & R Stanger South Seatter Sandwick £1496 Williamsons East Road Kirkwall 3rd No 7 A T Rendall Old hall Stromness -

Festive Period Domestic and Commercial Refuse Collections
Festive Period Domestic and Commercial Refuse Collections Mainland and Linked South Isles Domestic and commercial refuse collection days over the Christmas and New Year period are listed below. Regular waste collections will resume on Monday 6 January 2020. Domestic and Fortnightly Trade Refuse Collections Area. Normally Collected. Refuse Collection Dates. Area 1 – Kirkwall (Central and North West). Monday. Monday 23 December. Area 3 – Kirkwall (Central). Wednesday. Monday 23 December. Area 6 – East Holm, Deerness, Tankerness and Toab. Monday. Monday 23 December. Area 2 – Kirkwall (West). Tuesday. Tuesday 24 December. Area 7 – Kirkwall (South), Holm, Burray (North). Tuesday. Tuesday 24 December. Area 8 – South Ronaldsay and Burray (South). Wednesday. Tuesday 24 December. Area 4 – Kirkwall (South East). Thursday. Friday 27 December. Area 5 – Kirkwall (North East). Friday. Friday 27 December. Area 9 – Stromness (Central). Monday. Monday 30 December. Area 11 –Stromness (Outer), Sandwick and Birsay. Wednesday. Monday 30 December. Area 10 – Stromness (Outer Areas) and Stenness (West). Tuesday. Tuesday 31 December. Area 12 – Dounby, Birsay and Evie. Thursday. Friday 3 January 2020. Area 13 – Firth, Rendall, Evie and Harray. Friday. Friday 3 January 2020. Area 14 – Finstown, Stenness (East) and Harray. Thursday. Friday 3 January 2020. Area. Normally Collected. Refuse Collection Dates. Area 15 – Orphir and Stenness (West). Friday. Friday 3 January 2020. Domestic Recycling Information Please note alterations for domestic recycling collection over the festive period. Recycling centres will remain open – see separate advert for opening times. Area: Last recycling collection: Next recycling collection: Area 1 – Kirkwall (Central and North West). Monday 16 December. Monday 13 January 2020. Area 6 – East Holm, Deerness, Tankerness and Toab.