Nursing Assistant
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Improving the Quality of Life of the Elderly and Disabled
IMPROVING THE QUALITY OF LIFE OF THE ELDERLY AND DISABLED PEOPLE IN HUMAN SETTLEMENTS IMPROVING THE QUALITY OF LIFE OF ELDERLY AND DISABLED PEOPLE IN HUMAN SETTLEMENTS VOLUME I A Resource Book of Policy and Programmes from around the World United Nations Centre for Human Settlements (Habitat) Nairobi, 1993 HS/284/93E ISBN 92-1-131208-6 FOREWORD The world's population is ageing dramatically. The total number of people aged 60 and older grew from 200 million in 1950 to 400 million in 1982. Their number is expected to increase to 600 million in the year 2001 when 70 per cent of them will live in developing countries. This demographic revolution has major consequences on the way human settlements are designed, managed and used. The United Nations and its agencies have undertaken many activities that recognize this reality. The General Assembly adopted the World Programme of Action concerning Disabled Persons and proclaimed 1981 the International Year of Disabled Persons. In 1982, 124 Member States adopted the International Plan of Action on Aging at the World Assembly on Aging. These two landmark events launched a variety of activities and studies during the United Nations Decade of Elderly and Disabled Persons. The United Nations Centre for Human Settlements (Habitat) launched the decade with two important documents. Designing with Care - a Guide to Adaptation of the Built Environment for Disabled Persons was published as the result of cooperation between the United Nations, UNCHS (Habitat) and the Swedish International Development Agency (SIDA). This guide pointed out that implementation of suggested design guidelines and related policies and programmes would have to be undertaken by authorities, taking into consideration the economic, social and climatic conditions of the human settlement concerned. -

DOCUMENT RESUME Essential Skills for the Care Team. A
DOCUMENT RESUME ED 419 937 CE 076 574 TITLE Essential Skills for the Care Team. A Program for New Employees in Residential and Home Care. INSTITUTION State Univ. of New York, Albany. Rockefeller Coll.; Eddy/Northeast Health, Troy, NY. SPONS AGENCY Office of Vocational and Adult Education (ED), Washington, DC. National Workplace Literacy Program. PUB DATE 1998-00-00 NOTE 456p.; For a related document, see CE 076 575. CONTRACT V198A40098-96 PUB TYPE GuideS Classroom Teacher (052) EDRS PRICE MF01/PC19 Plus Postage. DESCRIPTORS Adult Basic Education; Allied Health Occupations Education; Classroom Techniques; Competence; Competency Based Education; *Home Health Aides; *Nurses Aides; *On the Job Training; Postsecondary Education; Teaching Methods; Units of Study; *Workplace Literacy ABSTRACT This document contains modules for two types of training. It provides 20 hours of training to newly hired Nursing Assistant Trainees (NATs) in residential care settings preparing to become state Certified Nursing Assistants (CNAs), using eight stand-alone modules supported by training process guides. It also includes 7 hours of training for newly hired NATs in the home care settings preparing to become state certified Home Health Aides (HHAs), using five stand-alone modules with training process guides. The materials are suitable for workplace literacy programs for adults with low levels of English literacy skills. A learning strategies module serves as an introduction to both programs. The CNA program contains the following modules: understanding your -

Eating Disorders
What to Expect… Medical Stabilization Program for Eating Disorders CHOC has developed a multidisciplinary approach in the treatment of acute medical instability related to eating disorders. Admission is designed to: Assess and treat medical disorders resulting from abnormal eating. Provide nutritional rehabilitation Prevent long-term and life threatening complications The patient’s stay depends on the level of medical instability. Once medically stable, we will help facilitate treatment arrangements to continue treatment for the eating disorder following discharge. Treatment includes: Complete physical examination and laboratory testing Individualized medical treatment plan including vitamin and mineral supplements Cardio-respiratory monitoring Nutritional assessment and management Growth and development evaluation Psychological evaluation and monitoring Psychiatric medication evaluation and monitoring as needed What to expect during hospitalization: Patients will receive one-to-one supervision of activity at all times, including meals and snacks and bathroom privileges. Visitors limited to parents, unless otherwise authorized by the multidisciplinary team. Activity level based on vitals o Strict medical bedrest: complete bedrest with commode at bedside. May stand only for daily weight and vitals; sit in chair for linen change; bed bath only, no shower. o Bedrest with wheelchair privileges: If vital signs stable, may be pushed in a wheelchair by staff on the floor; may take seated shower, use toilet in bathroom, sit at sink. o Bedrest with ambulation privileges – may use toilet in bathroom and may shower. If vital signs stable, may be pushed in a wheelchair by staff on the floor and may be up in room for short periods, otherwise on bedrest. Outside foods are not allowed unless approved by Nutrition. -

Cruising Game Space
CRUISING GAME SPACE Game Level Design, Gay Cruising and the Queer Gothic in The Rawlings By Tommy Ting A thesis exhibition presented to OCAD University in partial fulfillment of the requirements for the degree of Master of Fine Arts in Digital Futures Toronto Media Arts Centre 32 Lisgar Street., April 12, 13, 14 Toronto, Ontario, Canada April 2019 Tommy Ting 2019 This work is licensed under the Creative Commons Attribution-Non Commercial-ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc- sa/4.0/ or send a letter to Creative Commons, 444 Castro Street, Suite 900, Mountain View, California, 94041, USA. Copyright Notice Author’s Declaration This work is licensed under the Creative Commons Attribution-NonCommercial- ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/ or send a letter to Creative Commons, 444 Castro Street, Suite 900, Mountain View, California, 94041, USA. You are free to: Share – copy and redistribute the material in any medium or format Adapt – remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms. Under the follower terms: Attribution – You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. NonCommericial – You may not use the material for commercial purposes. ShareAlike – If you remix, transform, or build upon the material, you must distribute you contributions under the same license as the original. -

2006-2007 Grievance Report
2006-2007 Final Grievance Report Summary of Grievance Process and Analysis of Grievances Received from October 2006 through June 2007 from Selected Facilities in Nevada Prepared by: Nevada Institute for Children’s Research and Policy Tara Swanson, M.A. - Research Analyst Jennifer Zipoy, M.A. - Director of Research Denise Tanata Ashby, J.D. - Executive Director Commissioned by the Nevada State Legislative Counsel Bureau Table of Contents Introduction………………………………………………………………………………………3 Methods...………………………………………………………………………………………....4 Limitations of the Data..…………………………………………………………………………7 Existing Complaint Processes.…………………………………………………………………..8 Corrections………………………………………………………………………………...8 Detention…………………………………………………………………………………..9 Child Welfare……………………………………………………………………………...9 Mental Health/Substance Abuse Treatment……………………………………………...10 Group Homes…………………………………………………………………………….10 Descriptive Statistics for all Complaints………………………………………………………10 Number of Facilities Participating by Month……………………………………………11 Complaints by Facility Type……………………………………………………………..12 Complaints by Facility Name……………………………………………………………13 Other Statistics…………………………………………………………………………...13 Complaints by Type……………………………………………………………………...14 Complaint Elements……………………………………………………………………...15 Types of Complaint Responses…………………………………………………………..15 Narrative Summary of Complaints and Responses…………………………………………..16 Heath Complaints………………………………………………………………………...16 Safety Complaints………………………………………………………………………..17 Welfare Complaints……………………………………………………………………...17 Treatment Complaints……………………………………………………………………18 -
Uploads/NCLEX Test.Pdf
73397_FMxx_FINAL.QXD 4/8/10 2:21 PM Page i NCLEX® High-Risk The Disaster Prevention Manual for Nurses Determined to Pass the RN Licensing Examination Marian C. Condon, DEd, RN, CNE Professor Department of Nursing York College of Pennsylvania York, Pennsylvania Karen S. March, PhD, RN, CCRN, ACNS-BC Professor Department of Nursing York College of Pennsylvania York, Pennsylvania 73397_FMxx_FINAL.QXD 4/8/10 2:21 PM Page ii World Headquarters Jones & Bartlett Learning Jones & Bartlett Learning Canada Jones & Bartlett Learning International 40 Tall Pine Drive 6339 Ormindale Way Barb House, Barb Mews Sudbury, MA 01776 Mississauga, Ontario L5V 1J2 London W6 7PA 978-443-5000 Canada United Kingdom [email protected] www.jblearning.com Jones & Bartlett Learning books and products are available through most bookstores and online booksellers. To contact Jones & Bartlett Learning directly, call 800-832-0034, fax 978-443-8000, or visit our website, www.jblearning.com. Substantial discounts on bulk quantities of Jones & Bartlett Learning publications are available to corpora- tions, professional associations, and other qualified organizations. For details and specific discount informa- tion, contact the special sales department at Jones & Bartlett Learning via the above contact information or send an email to [email protected]. Copyright © 2011 by Jones & Bartlett Learning, LLC All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission from the copyright owner. The authors, editor, and publisher have made every effort to provide accurate information. -

TABLE of CONTENTS SECTION 100—DEFINITIONS and LICENSURE 101. Definitions. 102. License Requirements. SECTION 200—ENFORCEMENT
61–93. STANDARDS FOR LICENSING FACILITIES FOR CHEMICALLY DEPENDENT OR ADDICTED PERSONS. (Statutory Authority: 1976 Code §§ 44–7–260 et seq.) Editor’s Note Unless otherwise noted, the following constitutes the history for 61–93, 101 to 3223. HISTORY: Added by State Register Volume 12, Issue No. 2, eff February 26, 1988. Amended by State Register Volume 25, Issue No. 5, Part 1, eff May 25, 2001; State Register Volume 34, Issue No. 6, eff June 25, 2010; State Register Volume 39, Issue No. 6, Doc. No. 4464, eff June 26, 2015; SCSR 44–6 Doc. No. 4954, eff June 26, 2020. The Table of Contents appears as published in SCSR 44-6 Doc. No. 4954; there is no text for ‘‘504. Staffing for Withdrawal Management Programs (I)’’ or ‘‘2616. Seclusion Room (II)’’. TABLE OF CONTENTS SECTION 100—DEFINITIONS AND LICENSURE 101. Definitions. 102. License Requirements. SECTION 200—ENFORCEMENT OF REGULATIONS 201. General. 202. Inspections and Investigations. 203. Consultations. SECTION 300—ENFORCEMENT ACTIONS 301. General. 302. Violation Classifications. SECTION 400—POLICIES AND PROCEDURES SECTION 500—STAFF AND TRAINING 501. General (II). 502. Administrator (II). 503. Staffing for Residential Treatment Programs (I). 504. Staffing for Withdrawal Management Programs (I). 505. Staffing for Opioid Treatment Programs (I). 506. In-service Training (II). 507. Health Status (I). 508. Counselors (II). SECTION 600—REPORTING 601. Accidents and Incidents (II). 602. Fire and Disasters (II). 603. Communicable Diseases and Animal Bites (I). 604. Administrator Change. 605. Joint Annual Report. 606. Accounting of Controlled Substances (I). 607. Facility Closure. 608. Zero Census. SECTION 700—PATIENT RECORDS 701. -
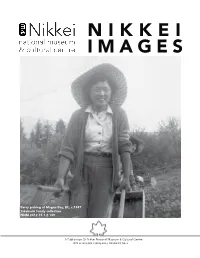
Nikkei Images Is Published by the Nikkei Example of This – All Five Regular Staff Members Are Women
n i k k e i i m a g e s Berry picking at magna Bay, BC, c.1947 Takahashi family collection nnm 2012.15.1.2.139 A Publication Of Nikkei National Museum & Cultural Centre ISSN # 1203-9017 Spring 2013, Volume 18, No. 1 Front Cover Photo – Yoko Takahashi Picking Berries 1 The Strength of Nikkei Women 2 Telling Everyone’s Stories in the Museum, by Beth Carter 3 The Diary of Kazue (Shiyoji) Oye, translated by Stan Fukawa 4 Jean Shigeko Kitagawa , by Masako Fukawa 10 Celebrating Nikkei Women 16 My Share of Good Luck, by Margaret Lyons 18 Treasures from the Collection 24 CONTENTS Berry pICkINg aT MagNa BaY, BC The STrengTh of C.1947 TakahaShI family collection Nikkei Women NNM 2012.15.1.2.139 ur current issue celebrates the strength of Japanese Canadian women. Since the earli- est days of immigration, women have been expected to help support the family. They Oworked in canneries, took in sewing, ran shops, helped on the farm, did cleaning and also maintained their children, housework and cooking. It sounds exhausting! This photograph shows Yoko Takahashi at age 15 working in the berry farms at Magna Bay, on Shuswap Lake. During the war years, the Takahashi family first went to Tashme, and in 1945 moved to Rosebery and New Denver. Because work in the Slocan Valley was scarce, many com- munity members travelled to the berry and fruit farms for several weeks of intense labour in the harvesting season. The museum collections include thousands of photographs of women at work that assist us to understand the many diverse roles women embraced within the Japanese Canadian community. -

Edited by Russell Shuttleworth and Teela Sanders
SEX AND DISABILITY: Politics, Identity and Access Edited by Russell Shuttleworth and Teela Sanders 2010 The Disability Press Leeds First published 20010 The Disability Press Centre for Disability Studies School of Sociology and Social Policy University of Leeds Leeds LS2 9JT © 2010: The Disability Press/Russell Shuttleworth and Teela Sanders, selection and editorial matter, individual chapters. The contributors. Output from disk cover supplied and printed by University Print Services, a division of Media Services at Leeds. All rights reserved. No part of this book may be reprinted or reproduced or utilised in any form by any electronic, mechanical, or other means, now known or hereafter invented, including photocopying and recording, or in any information storage or retrieval system, without permission in writing from the publishers. British Library Catalgouing in publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloguing in publication Data A catalogue record of this book has been requested ISBN: 0-9549026-6-1 Contents The Disability Press Acknowledgements Contributors Preface INTRODUCTION: THE STATE OF THE FIELD 1. Towards an Inclusive Sexuality and Disability Research Agenda— Russell Shuttleworth PART I - CONSTRUCTING THE SEXUALITY OF DISABLED PEOPLE 2. Sexual ‘Vulnerability’ of People with Learning Difficulties: A Self- Fulfilling Prophecy—Andrea Hollomotz 3. Members Only: The Use of Gay Space(s) by Gay Disabled Men— Craig Blyth 4. Crip Sexuality: Sk(r)ewed Media Representation—Bethany Stevens 5. Exploring the Barriers to Sex and Relationships for People with Learning Difficulties—Ruth Garbutt 6. Disability, Masculinity, and Sexuality in Post-Soviet Ukraine— Sarah Phillips 7. -

Abbreviations
CORPORATE CLINICAL POLICY AND PROCEDURE CORP.#: CLN: 3010 Approved For: X CHE X CHN X CHS X CHVH X CWH Page 1 of 37 CANCELS: 11/20/12; 4/12/13 EFFECTIVE: 12/4/14 TITLE: ABBREVIATIONS STATEMENT OF PURPOSE: To establish the policy and procedure to govern what abbreviations are approved for use in the medical record and what abbreviations are prohibited from use in the medical record. The Abbreviations Committee will try by policy to comply with the licensing authority of the State and accrediting bodies, e.g. JCAHO. TEXT: 1. The Abbreviations Committee is responsible for reviewing and maintaining the list of Approved Abbreviations and Prohibited Abbreviations. This Committee is multi-disciplinary and consists of members from Health Information Management, Nursing, Pharmacy, Quality Resources, and Physician as well as ad hoc representation from other hospital departments. Any healthcare provider may submit a request for change (additions/deletions) to the listings to the Abbreviations Committee for review. 2. The Abbreviations Committee will approve changes and then submit recommendations for changes to the list to the Medical Executive Committee/Council. The Medical Executive Committee/Council must approve all modifications to this list prior to implementation. 3. The master listing of the Approved Abbreviations and Prohibited Abbreviations will be on the Community Health Network InComm (intranet) and TIHH InComm (intranet), and maintained by the Director of Health Information Management. Listing to be referenced by any health care provider for clarification of abbreviations prior to use. Any abbreviations that are not on the approved list must be written out as the full word. -

Module 9: Patient Care Procedures California Community Colleges
Module 9: Patient Care Procedures Module 9: Patient Care Procedures Minimum Number of Theory Hours: 7 Recommended Clinical Hours: 20 Statement of Purpose: The purpose of this unit is to provide learning experiences that will prepare the Nurse Assistant to safely carry out procedures that support the patient/resident in meeting physical care needs that cannot be performed independently. Terminology: 1. Admission 23. Manual bed 2. Anti-embolic stockings 24. Mitered corner 3. Bandage 25. Mucous 4. Binders 26. Nasogastric tube (NGT) 5. Clean catch 27. Non-prescription 6. Defecate 28. Occupied bed 7. Discharge 29. Ointment 8. Draw sheet 30. Output 9. Edema 31. Percutaneous Endoscopic Gastrostomy (PEG) 10. Elastic bandage 32. Pruritus 11. Electric bed 33. Reflux 12. Evacuation 34. Reverse Trendelenburg 13. Excoriated 35. Scaly 14. Expectorate 36. Semi-Fowler’s position 15. Fanfold 37. Side rails 16. Fluid 38. Specimen 17. Gastrostomy tube 39. Suppository 18. Hives 40. Transfer 19. Intake 41. Trendelenburg 20. Integumentary system 42. Unoccupied bed 21. Intravenous (IV) 22. Lesions Patient, resident, and client are synonymous terms referring to the person receiving care California Community Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 58 Module 9: Patient Care Procedures Performance Standards (Objectives): Upon completion of seven (7) hours of class plus assignments and twenty (20) hours of clinical experience, the learner will be able to: 1. Define key terminology COLLECTION of SPECIMENS 2. Describe the Nurse Assistant’s role in collecting specimens (sputum, urine, and/or stool) BED CARE 3. Discuss procedures for bed making and maintaining proper body mechanics 4. -

Parent-Student Handbook for Pre-Kindergarten to Grade 5
NEW COVENANT CHRISTIAN SCHOOL Developing the Leaders of Tomorrow in a Christ-Centered Environment Parent-Student Handbook For Pre-Kindergarten to Grade 5 (Revised August 2016) The fear of the Lord is the beginning of wisdom, and the knowledge of the Holy One is understanding. Proverbs 9: 10 (NKJV) www.ncchristianschool.org Table of Contents Welcome to New Covenant Christian School ....................................................................................... 4 NCCS Contact Information.................................................................................................................... 5 Re-Enrollment Procedure...................................................................................................................... 6 Dress Code ............................................................................................................................................. 6 The Standard Uniform ...................................................................................................................... 6 Gym Uniform ..................................................................................................................................... 6 Other .................................................................................................................................................. 6 Arrival .................................................................................................................................................... 7 Dismissal, Pickup, and Afterschool ......................................................................................................