Definitions of Medicare Code Edits
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
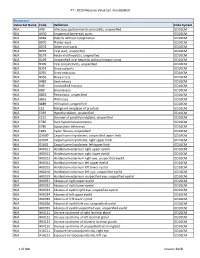
PT - 2020 Measure Value Set Avoidableed
PT - 2020 Measure Value Set_AvoidableED Numerator Value Set Name Code Definition Code System N/A A09 Infectious gastroenteritis and colitis, unspecified ICD10CM N/A A630 Anogenital (venereal) warts ICD10CM N/A B069 Rubella without complication ICD10CM N/A B070 Plantar wart ICD10CM N/A B078 Other viral warts ICD10CM N/A B079 Viral wart, unspecified ICD10CM N/A B179 Acute viral hepatitis, unspecified ICD10CM N/A B199 Unspecified viral hepatitis without hepatic coma ICD10CM N/A B309 Viral conjunctivitis, unspecified ICD10CM N/A B354 Tinea corporis ICD10CM N/A B355 Tinea imbricata ICD10CM N/A B356 Tinea cruris ICD10CM N/A B483 Geotrichosis ICD10CM N/A B49 Unspecified mycosis ICD10CM N/A B80 Enterobiasis ICD10CM N/A B852 Pediculosis, unspecified ICD10CM N/A B853 Phthiriasis ICD10CM N/A B889 Infestation, unspecified ICD10CM N/A C61 Malignant neoplasm of prostate ICD10CM N/A E039 Hypothyroidism, unspecified ICD10CM N/A E215 Disorder of parathyroid gland, unspecified ICD10CM N/A E780 Pure hypercholesterolemia ICD10CM N/A E786 Lipoprotein deficiency ICD10CM N/A E849 Cystic fibrosis, unspecified ICD10CM N/A G5600 Carpal tunnel syndrome, unspecified upper limb ICD10CM N/A G5601 Carpal tunnel syndrome, right upper limb ICD10CM N/A G5602 Carpal tunnel syndrome, left upper limb ICD10CM N/A H00011 Hordeolum externum right upper eyelid ICD10CM N/A H00012 Hordeolum externum right lower eyelid ICD10CM N/A H00013 Hordeolum externum right eye, unspecified eyelid ICD10CM N/A H00014 Hordeolum externum left upper eyelid ICD10CM N/A H00015 Hordeolum externum -

Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N
case report Oman Medical Journal [2017], Vol. 32, No. 6: Hypocalcemia Associated with Subcutaneous Fat Necrosis of the Newborn: Case Report and Literature Review Alphonsus N. Onyiriuka 1* and Theodora E. Utomi2 1Endocrine and Metabolic Unit, Department of Child Health, University of Benin Teaching Hospital, Benin City, Nigeria 2Special Care Baby Unit, Department of Nursing Services, St Philomena Catholic Hospital, Benin City, Nigeria ARTICLE INFO ABSTRACT Article history: Subcutaneous fat necrosis of the newborn (SCFNN) is a rare benign inflammatory Received: 4 November 2015 disorder of the adipose tissue but may be complicated by hypercalcemia or less frequently, Accepted: 21 October 2016 hypocalcemia, resulting in morbidity and mortality. Here we report the case of a neonate Online: with subcutaneous fat necrosis who surprisingly developed hypocalcemia instead DOI 10.5001/omj.2017.99 of hypercalcemia. A full-term female neonate was delivered by emergency cesarean section for fetal distress and was subsequently admitted to the Special Care Baby Keywords: Hypocalcemia; Infant, Unit. The mother’s pregnancy was uncomplicated up to delivery. Her anthropometric Newborn; Subcutaneous Fat measurements were birth weight 4.1 kg (95th percentile), length 50 cm (50th percentile), Necrosis; Perinatal Stress. and head circumference 34.5 cm (50th percentile). The Apgar scores were 2, 3, and 8 at 1, 5, 10 minutes, respectively. There was no abnormal facies and she was fed with breast milk only. On the seventh day of life, the infant was found to have multiple nodules located in the neck, upper back, and right arm. The nodules were firm, well circumscribed with no evidence of tenderness. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -
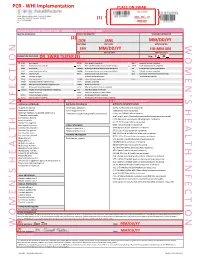
Womens Health Requisition Forms
PCR - WHI Implementation PLACE ON SWAB 10854 Midwest Industrial Blvd. St. Louis, MO 63132 MM DD YY Phone: (314) 200-3040 | Fax (314) 200-3042 (1) CLIA ID #26D0953866 JANE DOE v3 PCR MOLECULAR REQUISITION - WOMEN'S HEALTH INFECTION PRACTICE INFORMATION PATIENT INFORMATION *SPECIMEN INFORMATION (2) DOE JANE MM/DD/YY LAST NAME FIRST NAME DATE COLLECTED W O M E ' N S H E A L T H I F N E C T I O N SSN MM/DD/YY HH:MM AM SSN DATE OF BIRTH TIME COLLECTED REQUESTING PHYSICIAN: DR. SWAB TESTER (3) Sex: F X M (4) Diagnosis Codes X N76.0 Acute vaginitis B37.49 Other urogenital candidiasis A54.9 Gonococcal infection, unspecified N76.1 Subacute and chronic vaginitis N89.8 Other specified noninflammatory disorders of vagina A59.00 Urogenital trichomoniasis, unspecified N76.2 Acute vulvitis O99.820 Streptococcus B carrier state complicating pregnancy A64 Unspecified sexually transmitted disease N76.3 Subacute and chronic vulvitis O99.824 Streptococcus B carrier state complicating childbirth A74.9 Chlamydial infection, unspecified N76.4 Abscess of vulva B95.1 Streptococcus, group B, as the cause Z11.3 Screening for infections with a predmoninantly N76.5 Ulceration of vagina of diseases classified elsewhere sexual mode of trasmission N76.6 Ulceration of vulva Z22.330 Carrier of group B streptococcus Other: N76.81 Mucositis(ulcerative) of vagina and vulva N70.91 Salpingitis, unspecified N76.89 Other specified inflammation of vagina and vulva N70.92 Oophoritis, unspecified N95.2 Post menopausal atrophic vaginitis N71.9 Inflammatory disease of uterus, unspecified -

Thyroid Disease in the Perinatal Period
Thyroid Thyroid disease in Simon Forehan the perinatal period Background Thyroid dysfunction affects 2–3% of pregnant women and Thyroid hormone plays a critical role in fetal development. In one in 10 women of childbearing age with normal thyroid pregnancy, increased thyroid hormone synthesis is required to function have underlying thyroid autoimmunity, which may meet fetal needs, resulting in increased iodine requirements. indicate reduced functional reserve.1 Up to 18% of women in Objective the first trimester in Australia are thyroid antibody positive.2 This article outlines changes to thyroid physiology and Thyroid hormone plays a critical role in pregnancy and iodine requirements in pregnancy, pregnancy specific understanding the unique changes to thyroid physiology in reference ranges for thyroid function tests and detection and pregnancy has important implications for the definition and management of thyroid conditions in pregnancy. treatment of thyroid disorders in pregnancy. Discussion Thyroid dysfunction affects 2–3% of pregnant women. Pregnancy specific reference ranges are required to define Thyroid physiology and pregnancy thyroid conditions in pregnancy and to guide treatment. The fetus is dependent on transplacental transfer of maternal thyroxine Overt maternal hypothyroidism is associated with adverse (T4). Deiodination of maternal T4 by the fetus results in local fetal pregnancy outcomes; thyroxine treatment should be production of liothyronine (T3), which is particularly important for commenced immediately in this condition. Thyroxine neurological development.3,4 Maternal T3 does not cross the placenta treatment has also been shown to be effective for pregnant and appears to have little, if any, role in development. Other changes in women with subclinical hypothyroidism who are thyroid pregnancy include an increase in thyroid binding globulin (TBG), resulting peroxidase antibody positive. -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Disseminated Eosinophilic Infiltration of a Newborn Infant, with Perforation of the Terminal Ileum and Bile Duct Obstruction
Arch Dis Child: first published as 10.1136/adc.56.1.66 on 1 January 1981. Downloaded from 66 Shinozaki, Saito, and Shiraki infant who acquired hepatitis from her mother. Br Med J 6 Yoshida A, Tozawa M, Furukawa N, Oya N, Kusunoki T, 1970; iv: 719-21. Kiyosawa N. HBsAg-positive chronic active hepatitis in 3 Bancroft W H, Warkel R L, Talbert A A, Russell P K. a 1 and 1/2 year-old-child (in Japanese). Shonika Shinryo Family with hepatitis-associated antigen. JAMA 1971; 1977;40: 1246-50. 217:1817-20. McCarthy J W. Hepatitis B antigen (HBAg)-positive chronic aggressive hepatitis and cirrhosis in an 8-month- Correspondence to Dr T Shinozaki, Department of old infant. A case report. JPediatr 1973; 83: 638-9. Paediatrics, Teikyo University School of Medicine, 11-1 5 Fujiwara T, Abe M, Tachi N, Jo M, Shiroda M. Kaga, 2 Chome, Itabashi-ku, Tokyo 173, Japan. HBsAg-positive infantile hepatitis associated with chronic aggressive hepatitis (in Japanese). Shonika Rinsho 1975; 28:1303-6. Received 26 November 1979 Disseminated eosinophilic infiltration of a newborn infant, with perforation of the terminal ileum and bile duct obstruction S M MURRAY AND C J WOODS Department ofPathology and Department ofPaediatrics, Victoria Hospital, Blackpool Case report SUMMARY A preterm boy died 4 days after delivery from septicaemia which at necropsy was found to be A white boy, weighing 1490 g, was born by spon- due to perforation of an eosinophilic lesion of the taneous vertex delivery at 35 weeks' gestation to a copyright. terminal ileum. -
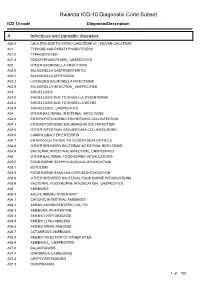
Rwanda ICD-10 Diagnostic Code Subset
Rwanda ICD-10 Diagnostic Code Subset ICD 10 code Diagnosis/Description A Infectious and parasitic diseases A00.0 CHOLERA DUE TO VIBRIO CHOLERAE 01_ BIOVAR CHOLERAE A01 TYPHOID AND PARATYPHOID FEVERS A01.0 TYPHOID FEVER A01.4 PARATYPHOID FEVER_ UNSPECIFIED A02 OTHER SALMONELLA INFECTIONS A02.0 SALMONELLA GASTROENTERITIS A02.1 SALMONELLA SEPTICEMIA A02.2 LOCALIZED SALMONELLA INFECTIONS A02.9 SALMONELLA INFECTION_ UNSPECIFIED A03 SHIGELLOSIS A03.0 SHIGELLOSIS DUE TO SHIGELLA DYSENTERIAE A03.2 SHIGELLOSIS DUE TO SHIGELLA BOYDII A03.9 SHIGELLOSIS_ UNSPECIFIED A04 OTHER BACTERIAL INTESTINAL INFECTIONS A04.0 ENTEROPATHOGENIC ESCHERICHIA COLI INFECTION A04.1 ENTEROTOXIGENIC ESCHERICHIA COLI INFECTION A04.4 OTHER INTESTINAL ESCHERICHIA COLI INFECTIONS A04.5 CAMPYLOBACTER ENTERITIS A04.7 ENTEROCOLITIS DUE TO CLOSTRIDIUM DIFFICILE A04.8 OTHER SPECIFIED BACTERIAL INTESTINAL INFECTIONS A04.9 BACTERIAL INTESTINAL INFECTION_ UNSPECIFIED A05 OTHER BACTERIAL FOOD-BORNE INTOXICATIONS A05.0 FOOD-BORNE STAPHYLOCOCCAL INTOXICATION A05.1 BOTULISM A05.4 FOOD-BORNE BACILLUS CEREUS INTOXICATION A05.8 OTHER SPECIFIED BACTERIAL FOOD-BORNE INTOXICATIONS A05.9 BACTERIAL FOOD-BORNE INTOXICATION_ UNSPECIFIED A06 AMEBIASIS A06.0 ACUTE AMEBIC DYSENTERY A06.1 CHRONIC INTESTINAL AMEBIASIS A06.2 AMEBIC NONDYSENTERIC COLITIS A06.3 AMEBOMA OF INTESTINE A06.4 AMEBIC LIVER ABSCESS A06.5 AMEBIC LUNG ABSCESS A06.6 AMEBIC BRAIN ABSCESS A06.7 CUTANEOUS AMEBIASIS A06.8 AMEBIC INFECTION OF OTHER SITES A06.9 AMEBIASIS_ UNSPECIFIED A07.0 BALANTIDIASIS A07.1 GIARDIASIS [LAMBLIASIS] -

MFM Clinical Guideline
MFM Clinical Guideline Thyroid Disease in Pregnancy Thyroid disease is the 2nd most common endocrinopathy in pregnancy after diabetes. In pregnancy: thyroid volume ↑ 30%, total/bound T3 and T4 levels ↑, but free/unbound T3 and T4 levels are stable due to ↑ thyroid binding globulin. In the 1st trimester, TSH levels ↓ due to high levels of hCG,which directly stimulates the TSH receptor, but return to baseline in the 2nd trimester. TSH does not cross the placenta. Maternal T4 is transferred to the fetus and is important for fetal brain development, especially before the fetal thyroid gland begins to synthesize thyroid hormone at 12-14 weeks. Screening for Thyroid Disease in Pregnancy Table 1: Screening. Table 2: Pregnancy reference ranges. Who to Screen Trimester TSH FT4* Age > 30 1st 0.1 - 2.5 0.8 - 1.2 BMI > 40 mIU/L ng/dL Current signs/symptoms of thyroid dysfunction 2nd 0.2 - 3 mIU/L 0.6 - 1 ng/dL Known positive thyroid antibodies 3rd 0.3 - 3 mIU/L 0.5 - 0.8 ng.dL Goiter *Due to inaccuracy of thyroid testing in pregnancy, Hx head/neck irradiation or thyroid surgery FT4 goal FHx thyroid disease should be the upper half of the reference range Pregestational diabetes Table 3: Interpreting the results. Autoimmune disorders TSH FT4 Hx of pregnancy loss, PTD, infertility Use of amiodarone or lithium, recent administration of Overt Hyperthyroidism ↓ ↑ iodinated radiologic contrast Subclinical ↓ NL Hyperthyroidism Residing in an area of known iodine deficiency Gestational 1st trim: ↓ UL How to Screen Hyperthyroidism 2nd trim: NL/ Step 1: TSH, -
Diagnostic Tests for Vaginosis/Vaginitis
Alberta Heritage Foundation for Medical Research Diagnostic tests for vaginosis/vaginitis Christa Harstall and Paula Corabian October 1998 HTA12 Diagnostic tests for vaginosis/vaginitis Christa Harstall and Paula Corabian October 1998 © Copyight Alberta Heritage Foundation for Medical Research, 1998 This Health Technology Assessment Report has been prepared on the basis of available information of which the Foundation is aware from public literature and expert opinion, and attempts to be current to the date of publication. The report has been externally reviewed. Additional information and comments relative to the Report are welcome, and should be sent to: Director, Health Technology Assessment Alberta Heritage Foundation for Medical Research 3125 Manulife Place, 10180 - 101 Street Edmonton Alberta T5J 3S4 CANADA Tel: 403-423-5727, Fax: 403-429-3509 This study is based, in part, on data provided by Alberta Health. The interpretation of the data in the report is that of the authors and does not necessarily represent the views of the Government of Alberta. ISBN 1-896956-15-7 Alberta's health technology assessment program has been established under the Health Research Collaboration Agreement between the Alberta Heritage Foundation for Medical Research and the Alberta Health Ministry. Acknowledgements The Alberta Heritage Foundation for Medical Research is most grateful to the following persons for their comments on the draft report and for provision of information. The views expressed in the final report are those of the Foundation. Dr. Jane Ballantine, Section of General Practice, Calgary Dr. Deirdre L. Church, Microbiology, Calgary Laboratory Services, Calgary Dr. Nestor N. Demianczuk, Royal Alexandra Hospital, Edmonton Dr. -

Management of Endocrinopathies in Pregnancy: a Review of Current Evidence
International Journal of Environmental Research and Public Health Review Management of Endocrinopathies in Pregnancy: A Review of Current Evidence Daniela Calina 1,† , Anca Oana Docea 2,*,†, Kirill Sergeyevich Golokhvast 3,†, Stavros Sifakis 4, Aristides Tsatsakis 5 and Antonis Makrigiannakis 6 1 Department of Clinical Pharmacy, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania; [email protected] 2 Department of Toxicology, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania 3 Scientific Education Center of Nanotechnology, Far Eastern Federal University, Vladivostok 690950, Russia; [email protected] 4 Department of Obstetrics and Gynecology, Mitera Maternity Hospital, 71110 Heraklion, Crete, Greece; [email protected] 5 Department of Forensic Sciences and Toxicology, Faculty of Medicine, University of Crete, 71110 Heraklion, Crete, Greece; [email protected] 6 Department of Obstetrics and Gynecology, Medical School, University of Crete, 71110 Heraklion, Crete, Greece; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Received: 28 January 2019; Accepted: 27 February 2019; Published: 4 March 2019 Abstract: Pregnancy in women with associated endocrine conditions is a therapeutic challenge for clinicians. These disorders may be common, such us thyroid disorders and diabetes, or rare, including adrenal and parathyroid disease and pituitary dysfunction. With the development of assisted reproductive techniques, the number of pregnancies with these conditions has increased. It is necessary to recognize symptoms and correct diagnosis for a proper pharmacotherapeutic management in order to avoid adverse side effects both in mother and fetus. This review summarizes the pharmacotherapy of these clinical situations in order to reduce maternal and fetal morbidity. -
Postpartum Thyroiditis
FACT SHEET Postpartum Thyroiditis Inflammation can damage the thyroid, making it less able to WHAT IS POSTPARTUM produce thyroid hormone. This can lead to the second phase— THYROIDITIS? hypothyroidism. This phase may last up to a year. Too little thyroid hormone in your blood slows your metabolism. Many Postpartum thyroiditis is an inflammation of the thyroid gland. It women with hypothyroidism have a goiter—an enlarged thyroid usually occurs within a year after a woman gives birth. It affects gland that causes swelling in the front part of the neck. Other five to ten out of every 100 women after they deliver a baby. symptoms of hypothyroidism can include There are usually two phases of the disease—hyperthyroidism • Unexplained weight gain or inability to lose weight (too much thyroid hormone) and hypothyroidism (too little thyroid • Feeling tired or fatigued hormone). • Depression • Dry skin and brittle nails • Hair loss DID YOU KNOW? • Sensitivity to cold The thyroid gland, located in the front of your neck, releases a hormone that controls your metabolism—how your body uses and stores energy from food. In the usual first phase—hyperthyroidism—the inflamed thyroid gland leaks stored thyroid hormone (which consists of T3 and T4) into the blood. This phase usually lasts 2 to 4 months. Too much thyroid hormone in your blood causes your metabolism to speed up. Symptoms can include • Losing weight suddenly Thyroid • A fast heartbeat Gland • Tiredness • Feeling nervous • Sweating • Sensitivity to heat WHAT ARE THE RISKS OF POSTPARTUM THYROIDITIS? Questions to ask your doctor You are at greater risk of developing postpartum thyroiditis if you have an immune system disorder such as type 1 diabetes, a • Do my symptoms mean I might have personal or family history of thyroid disease, or had postpartum postpartum thyroiditis? thyroiditis before.