MFM Clinical Guideline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thyroid Disease in the Perinatal Period
Thyroid Thyroid disease in Simon Forehan the perinatal period Background Thyroid dysfunction affects 2–3% of pregnant women and Thyroid hormone plays a critical role in fetal development. In one in 10 women of childbearing age with normal thyroid pregnancy, increased thyroid hormone synthesis is required to function have underlying thyroid autoimmunity, which may meet fetal needs, resulting in increased iodine requirements. indicate reduced functional reserve.1 Up to 18% of women in Objective the first trimester in Australia are thyroid antibody positive.2 This article outlines changes to thyroid physiology and Thyroid hormone plays a critical role in pregnancy and iodine requirements in pregnancy, pregnancy specific understanding the unique changes to thyroid physiology in reference ranges for thyroid function tests and detection and pregnancy has important implications for the definition and management of thyroid conditions in pregnancy. treatment of thyroid disorders in pregnancy. Discussion Thyroid dysfunction affects 2–3% of pregnant women. Pregnancy specific reference ranges are required to define Thyroid physiology and pregnancy thyroid conditions in pregnancy and to guide treatment. The fetus is dependent on transplacental transfer of maternal thyroxine Overt maternal hypothyroidism is associated with adverse (T4). Deiodination of maternal T4 by the fetus results in local fetal pregnancy outcomes; thyroxine treatment should be production of liothyronine (T3), which is particularly important for commenced immediately in this condition. Thyroxine neurological development.3,4 Maternal T3 does not cross the placenta treatment has also been shown to be effective for pregnant and appears to have little, if any, role in development. Other changes in women with subclinical hypothyroidism who are thyroid pregnancy include an increase in thyroid binding globulin (TBG), resulting peroxidase antibody positive. -

Management of Endocrinopathies in Pregnancy: a Review of Current Evidence
International Journal of Environmental Research and Public Health Review Management of Endocrinopathies in Pregnancy: A Review of Current Evidence Daniela Calina 1,† , Anca Oana Docea 2,*,†, Kirill Sergeyevich Golokhvast 3,†, Stavros Sifakis 4, Aristides Tsatsakis 5 and Antonis Makrigiannakis 6 1 Department of Clinical Pharmacy, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania; [email protected] 2 Department of Toxicology, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania 3 Scientific Education Center of Nanotechnology, Far Eastern Federal University, Vladivostok 690950, Russia; [email protected] 4 Department of Obstetrics and Gynecology, Mitera Maternity Hospital, 71110 Heraklion, Crete, Greece; [email protected] 5 Department of Forensic Sciences and Toxicology, Faculty of Medicine, University of Crete, 71110 Heraklion, Crete, Greece; [email protected] 6 Department of Obstetrics and Gynecology, Medical School, University of Crete, 71110 Heraklion, Crete, Greece; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Received: 28 January 2019; Accepted: 27 February 2019; Published: 4 March 2019 Abstract: Pregnancy in women with associated endocrine conditions is a therapeutic challenge for clinicians. These disorders may be common, such us thyroid disorders and diabetes, or rare, including adrenal and parathyroid disease and pituitary dysfunction. With the development of assisted reproductive techniques, the number of pregnancies with these conditions has increased. It is necessary to recognize symptoms and correct diagnosis for a proper pharmacotherapeutic management in order to avoid adverse side effects both in mother and fetus. This review summarizes the pharmacotherapy of these clinical situations in order to reduce maternal and fetal morbidity. -
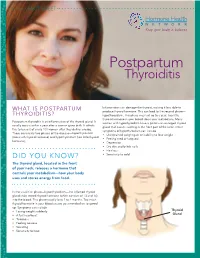
Postpartum Thyroiditis
FACT SHEET Postpartum Thyroiditis Inflammation can damage the thyroid, making it less able to WHAT IS POSTPARTUM produce thyroid hormone. This can lead to the second phase— THYROIDITIS? hypothyroidism. This phase may last up to a year. Too little thyroid hormone in your blood slows your metabolism. Many Postpartum thyroiditis is an inflammation of the thyroid gland. It women with hypothyroidism have a goiter—an enlarged thyroid usually occurs within a year after a woman gives birth. It affects gland that causes swelling in the front part of the neck. Other five to ten out of every 100 women after they deliver a baby. symptoms of hypothyroidism can include There are usually two phases of the disease—hyperthyroidism • Unexplained weight gain or inability to lose weight (too much thyroid hormone) and hypothyroidism (too little thyroid • Feeling tired or fatigued hormone). • Depression • Dry skin and brittle nails • Hair loss DID YOU KNOW? • Sensitivity to cold The thyroid gland, located in the front of your neck, releases a hormone that controls your metabolism—how your body uses and stores energy from food. In the usual first phase—hyperthyroidism—the inflamed thyroid gland leaks stored thyroid hormone (which consists of T3 and T4) into the blood. This phase usually lasts 2 to 4 months. Too much thyroid hormone in your blood causes your metabolism to speed up. Symptoms can include • Losing weight suddenly Thyroid • A fast heartbeat Gland • Tiredness • Feeling nervous • Sweating • Sensitivity to heat WHAT ARE THE RISKS OF POSTPARTUM THYROIDITIS? Questions to ask your doctor You are at greater risk of developing postpartum thyroiditis if you have an immune system disorder such as type 1 diabetes, a • Do my symptoms mean I might have personal or family history of thyroid disease, or had postpartum postpartum thyroiditis? thyroiditis before. -

Thyroid Disease in Pregnancy
Clinical Expert Series Continuing medical education is available online at www.greenjournal.org Thyroid Disease in Pregnancy Brian M. Casey, MD, and Kenneth J. Leveno, MD Thyroid testing during pregnancy should be performed on symptomatic women or those with a personal history of thyroid disease. Overt hypothyroidism complicates up to 3 of 1,000 pregnancies and is characterized by nonspecific signs or symptoms that are easily confused with complaints common to pregnancy itself. Physiologic changes in serum thyroid-stimulating hormone (TSH) and free thyroxine (T4) related to pregnancy also confound the diagnosis of hypothyroidism during pregnancy. If the TSH is abnormal, then evaluation of free T4 is recommended. The diagnosis of overt hypothyroidism is established by an elevated TSH and a low free T4. The goal of treatment with levothyroxine is to return TSH to the normal range. Overt hyperthyroidism complicates approximately 2 of 1,000 pregnancies. Clinical features of hyper- thyroidism can also be confused with those typical of pregnancy. Clinical hyperthyroidism is confirmed by a low TSH and elevation in free T4 concentration. The goal of treatment with thioamide drugs is to maintain free T4 in the upper normal range using the lowest possible dosage. Postpartum thyroiditis requiring thyroxine replacement has been reported in 2% to 5% of women. Most women will return to the euthyroid state within 12 months. (Obstet Gynecol 2006;108:1283–92) nterest in thyroid dysfunction complicating preg- would be identified if universal screening during Inancy has increased greatly during the past decade. pregnancy was adopted in the United States would This increased interest has been largely fueled by two have subclinical hypothyroidism.3 However, one of reports in 1999 that suggested offspring of women the most important U.S. -

344 Thyroid Disorders Definition/Cut-Off Value
05/2011 344 Thyroid Disorders Definition/Cut-Off Value Thyroid dysfunctions that occur in pregnant and postpartum women, during fetal development, and in childhood are caused by the abnormal secretion of thyroid hormones. The medical conditions include, but are not limited to, the following: Thyroid Dysfunction Definition Hyperthyroidism Excessive thyroid hormone production (most commonly known as Graves’ disease and toxic multinodular goiter). Hypothyroidism Low secretion levels of thyroid hormone (can be overt or mild/subclinical). Most commonly seen as chronic autoimmune thyroiditis (Hashimoto’s thyroiditis or autoimmune thyroid disease). It can also be caused by severe iodine deficiency. Congenital Hyperthyroidism Excessive thyroid hormone levels at birth, either transient (due to maternal Grave’s disease) or persistent (due to genetic mutation). Congenital Hypothyroidism Infants born with an under active thyroid gland and presumed to have had hypothyroidism in-utero. Postpartum Thyroiditis Transient or permanent thyroid dysfunction occurring in the first year after delivery based on an autoimmune inflammation of the thyroid. Frequently, the resolution is spontaneous. Presence of condition diagnosed, documented, or reported by a physician or someone working under physician’s orders, or as self reported by applicant/participant/caregiver. See Clarification for more information about self-reporting a diagnosis. Participant Category and Priority Level Category Priority Pregnant Women 1 Breastfeeding Women 1 Non-Breastfeeding Women 6 Infants 1 Children 3 1 of 5 Clinical/Health/Medical: Thyroid Disorders 344 05/2011 Justification The thyroid gland manufactures three thyroid hormones: thyroxine (T4), triiodothyronine (T3), and calcitonin. The thyroid hormones regulate how the body gets energy from food (metabolism). Iodine is an essential component of the T4 and T3 hormones (1) and must come from the diet. -

Thyrotoxicosis of Pregnancyq
Journal of Clinical & Translational Endocrinology 1 (2014) 140e144 Contents lists available at ScienceDirect Journal of Clinical & Translational Endocrinology journal homepage: www.elsevier.com/locate/jcte Review Thyrotoxicosis of pregnancyq Artak Labadzhyan, MD a,b, Gregory A. Brent, MD c, Jerome M. Hershman, MD d, Angela M. Leung, MD, MSc d,* a Division of Endocrinology, Cedars-Sinai Medical Center, Los Angeles, CA, USA b Division of Endocrinology, VA Greater Los Angeles Healthcare System, Los Angeles, CA, USA c Department of Medicine, David Geffen School of Medicine, University of California Los Angeles, USA d Division of Endocrinology, David Geffen School of Medicine, University of California Los Angeles, USA article info abstract Article history: Thyrotoxicosis presenting during pregnancy is a common clinical problem and can be challenging to Received 2 July 2014 differentiate between physiologic patterns of thyroid dysfunction during gestation and intrinsic hyper- Received in revised form thyroidism. This review provides a summary of the differential diagnosis, clinical presentation, diagnostic 21 July 2014 options, potential adverse effects of maternal thyrotoxicosis to the fetus, and treatment recommenda- Accepted 31 July 2014 tions for thyrotoxicosis arising in pregnancy. Ó 2014 The Authors. Published by Elsevier Inc. Open access under CC BY-NC-ND license. Keywords: Thyrotoxicosis Hyperthyroidism Pregnancy Introduction defined as TSH concentration below the lower limit of the reference range and elevated concentrations of serum T4 and T3 [2]. The most Metabolic disorders, including thyroid dysfunction, are among common cause of thyrotoxicosis in pregnancy is gestational tran- the most common pre-pregnancy diseases in pregnant women [1]. sient thyrotoxicosis (GTT), which occurs from the stimulatory ac- Thyrotoxicosis presenting in pregnancy can be particularly chal- tion of human chorionic gonadotropin (HCG) on the TSH receptor. -

Thyroid Disease in Pregnancy Uncontrolled Thyrotoxicosis and Hypothyroidism Are Associated with Adverse Pregnancy Outcomes
The American College of Obstetricians and Gynecologists WOMEN’S HEALTH CARE PHYSICIANS PRACTICE BULLETIN CLINICAL MANAGEMENT GUIDELINES FOR OBSTETRICIAN–GYNECOLOGISTS NUMBER 148, APRIL 2015 (Replaces Practice Bulletin Number 37, August 2002 and Committee Opinion Number 381, October 2007) Thyroid Disease in Pregnancy Uncontrolled thyrotoxicosis and hypothyroidism are associated with adverse pregnancy outcomes. There also is concern about the effect of overt maternal thyroid disease and even subclinical maternal thyroid disease on fetal development. In addition, medications that affect the maternal thyroid gland can cross the placenta and affect the fetal thyroid gland. This document reviews the thyroid-related pathophysiologic changes that occur during pregnancy and the effects of overt and subclinical maternal thyroid disease on maternal and fetal outcomes. thyroxine (T4) levels suppress hypothalamic thyrotropin- Background releasing hormone, which in turn limits pituitary TSH Changes in Thyroid Function During secretion. After the first trimester, TSH levels return to Pregnancy baseline values and progressively increase in the third trimester related to placental growth and production of Physiologic thyroid changes during pregnancy are con- placental deiodinase (2). These physiologic changes siderable and may be confused with maternal thyroid should be considered when interpreting thyroid function abnormalities. Maternal thyroid volume is 30% larger in test results during pregnancy (Table 1). the third trimester than in the first trimester (1). In addi- tion, there are changes to thyroid hormone levels and Table 1. Changes in Thyroid Function Test Results in Normal thyroid function throughout pregnancy. Table 1 depicts Pregnancy and in Thyroid Disease ^ how thyroid function test results change in normal preg- Maternal Status TSH Free T nancy and in overt and subclinical thyroid disease. -

Thyroid Disease in Pregnancy
Kung Thyroiddiseaseinpregnancy AWCKung It has long been known that there is a close relationship between pregnancy and the thyroid gland— iodine insufficiency, goitre development, and abnormal thyroid function are common during pregnancy. Autoimmune thyroid disease and thyrotoxicosis may also affect pregnant women, and their management requires the understanding of the interaction between the neuroendocrine and immune systems. In this article, the physiology of the thyroid gland during pregnancy and the interrelationship between pregnancy and autoimmune thyroid disease are discussed. HKMJ 1997;3:388-90 Key words: Autoimmune, diseases; Pregnancy complications; Thyroid gland; Thyroiditis; Thyrotoxicosis Introduction Increased iodine requirement During pregnancy, additional iodine is lost through Pregnancy poses an important challenge to the mater- the increased renal clearance of iodide.2 This loss is nal thyroid gland as hormone requirements are in- further aggravated during the second half of gestation creased during gestation. Understanding the normal because a fraction of the maternal inorganic iodide pool physio-logical adaptation of the pituitary-thyroidal axis is diverted towards the foetal-placental complex, in pregnancy enables us to manage cases of thyroid thereby further depriving the maternal thyroid from dysfunction. Autoimmune thyroid disease usually af- available iodine. It has been shown that in areas of fects females of the reproductive age group and caring borderline iodine intake, goitre develops with relative for these women during pregnancy requires careful hypothyroxinaemia, higher T3/T4 ratios indicate monitoring of both the mother and the foetus. This preferential T3 secretion, and higher, although normal, review summarises the physiological adaptation of serum TSH concentrations arise.3 Thus in places of the thyroid gland and the management of thyroid borderline iodine intake, iodine supplementation is disease during pregnancy. -

Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and Postpartum
THYROID PREGNANCY AND FETAL DEVELOPMENT Volume 21, Number 10, 2011 ª Mary Ann Liebert, Inc. DOI: 10.1089/thy.2011.0087 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and Postpartum The American Thyroid Association Taskforce on Thyroid Disease During Pregnancy and Postpartum Alex Stagnaro-Green (Chair),1 Marcos Abalovich,2 Erik Alexander,3 Fereidoun Azizi,4 Jorge Mestman,5 Roberto Negro,6 Angelita Nixon,7 Elizabeth N. Pearce,8 Offie P. Soldin,9 Scott Sullivan,10 and Wilmar Wiersinga11 INTRODUCTION Knowledge regarding the interaction between the thyroid and pregnancy/the postpartum period is advancing at a regnancy has a profound impact on the thyroid gland rapid pace. Only recently has a TSH of 2.5 mIU/L been ac- Pand thyroid function. The gland increases 10% in size cepted as the upper limit of normal for TSH in the first tri- during pregnancy in iodine-replete countries and by 20%– mester. This has important implications in regards to 40% in areas of iodine deficiency. Production of thyroxine interpretation of the literature as well as a critical impact for (T4) and triiodothyronine (T3) increases by 50%, along with a the clinical diagnosis of hypothyroidism. Although it is well 50% increase in the daily iodine requirement. These physi- accepted that overt hypothyroidism and overt hyperthy- ological changes may result in hypothyroidism in the later roidism have a deleterious impact on pregnancy, studies are stages of pregnancy in iodine-deficient women who were now focusing on the potential impact of subclinical hypo- euthyroid in the first trimester. -

Thyroid Hormone Dysfunction During Pregnancy: a Review
Int J Reprod BioMed Vol. 14. No. 11. pp: 677-686, November 2016 Review article Thyroid hormone dysfunction during pregnancy: A review 1 2 2 2 Aynadis AlemuP P M.Sc., Betelihem TerefeP P M.Sc., Molla AbebeP P M.Sc., Belete BiadgoP P M.Sc. 1. Amhara Regional Health Abstract Bureau, Dessie Regional Health Research Laboratory, Dessie, Thyroid dysfunctions such as hypothyroidism, thyrotoxicosis and thyroid nodules Ethiopia may develop during pregnancy leading to abortion, placental abruptions, 2. School of Biomedical and preeclampsia, preterm delivery and reduced intellectual function in the offspring. Laboratory Sciences, College of Epidemiological data have shown the significant role of maternal thyroid hormone Medicine and Health Sciences, University of Gondar, Ethiopia. in fetal neurologic development and maternal health. It has been suggested that the deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neuro-intellectual development in the early life of the child. Pregnancy poses an important challenge to the maternal thyroid gland as hormone requirements are increased during gestation as a result of an increase in thyroid- binding globulin, the stimulatory effect of HCG on TSH receptors, and increased peripheral thyroid hormone requirements. Maternal thyroid dysfunction is associated with increased risk for early abortion, preterm delivery, neonatal morbidity and other obstetrical complications. Early diagnosis for thyroid dysfunction of pregnant Corresponding Author: Belete Biadgo, School of women and treatment of thyroid dysfunction during pregnancy is important and cost Biomedical and Laboratory effective to avoid both fetal and maternal complications secondary to thyroid Sciences, College of Medicine and dysfunction. Therefore the aim of this review was to assess the thyroid function Health Sciences, University of changes occurring during pregnancy, the different disorders with their maternal and Gondar, Ethiopia. -

Complications of Pregnancy, Childbirth and the Puerperium Diagnosis Codes
Complications of Pregnancy, Childbirth and the Puerperium Diagnosis Codes 10058006 Miscarriage with amniotic fluid embolism (disorder) SNOMEDCT 10217006 Third degree perineal laceration (disorder) SNOMEDCT 102872000 Pregnancy on oral contraceptive (finding) SNOMEDCT 102873005 Pregnancy on intrauterine device (finding) SNOMEDCT 102875003 Surrogate pregnancy (finding) SNOMEDCT 102876002 Multigravida (finding) SNOMEDCT 106004004 Hemorrhagic complication of pregnancy (disorder) SNOMEDCT 106007006 Maternal AND/OR fetal condition affecting labor AND/OR delivery SNOMEDCT (disorder) 106008001 Delivery AND/OR maternal condition affecting management (disorder) SNOMEDCT 106009009 Fetal condition affecting obstetrical care of mother (disorder) SNOMEDCT 106010004 Pelvic dystocia AND/OR uterine disorder (disorder) SNOMEDCT 10853001 Obstetrical complication of general anesthesia (disorder) SNOMEDCT 111451002 Obstetrical injury to pelvic organ (disorder) SNOMEDCT 111452009 Postpartum afibrinogenemia with hemorrhage (disorder) SNOMEDCT 111453004 Retained placenta, without hemorrhage (disorder) SNOMEDCT 111454005 Retained portions of placenta AND/OR membranes without SNOMEDCT hemorrhage (disorder) 111458008 Postpartum venous thrombosis (disorder) SNOMEDCT 11209007 Cord entanglement without compression (disorder) SNOMEDCT 1125006 Sepsis during labor (disorder) SNOMEDCT 11454006 Failed attempted abortion with amniotic fluid embolism (disorder) SNOMEDCT 11687002 Gestational diabetes mellitus (disorder) SNOMEDCT 11942004 Perineal laceration involving pelvic -

Hyperthyroidism Management During Pregnancy and Lactation (Review)
EXPERIMENTAL AND THERAPEUTIC MEDICINE 22: 960, 2021 Hyperthyroidism management during pregnancy and lactation (Review) MIHAI CRISTIAN DUMITRASCU1,2*, ADINA‑ELENA NENCIU2*, SANDRU FLORICA3,4, CATALIN GEORGE NENCIU1,5, AIDA PETCA1,6, RĂZVAN‑COSMIN PETCA1,7 and ADRIAN VASILE COMĂNICI8,9 1Department of Obstetrics and Gynecology, ‘Carol Davila’ University of Medicine and Pharmacy, 050474 Bucharest; 2Department of Obstetrics and Gynecology, University Emergency Hospital, 050098 Bucharest; 3Department of Dermatology, ‘Carol Davila’ University of Medicine and Pharmacy, 050474 Bucharest; 4Department of Dermatology, Elias Emergency University Hospital, 011461 Bucharest; 5Department of Obstetrics and Gynecology, ‘Bucur’ Maternity, 040294 Bucharest; 6Department of Obstetrics and Gynecology, Elias Emergency Hospital, 011461 Bucharest; 7Department of Urology, ‘Prof. Dr. Th. Burghele’ Clinical Hospital, 050659 Bucharest; 8Department of Endocrinology ‘Titu Maiorescu’ University, University of Medicine and Pharmacy, 031593 Bucharest; 9Department of Endocrinology, ‘C.F. 2’ Clinical Hospital, 011464 Bucharest, Romania Received April 14, 2021; Accepted May 14, 2021 DOI: 10.3892/etm.2021.10392 Abstract. Thyroid dysfunction is a significant public health Contents issue, affecting 5‑10 more women compared to men. The estimated incidence is up to 12% and only for women the treat‑ 1. Introduction ment rises up to 4.3 billion dollars annually. Thyroid pathology 2. Clinical features of pregnant patients with hyperthyroidism can have a major impact on female fertility and it can only be 3. Fetal development in pregnancies with hyperthyroidism detected when preconception tests are performed. Untreated or 4. Treatment options in pregnancy poorly treated hyperthyroidism in a mother can affect the fetal 5. Thyroid dysfunction treatment in lactation period development and pregnancy outcome. Between 0.1 and 0.4% of 6.