1 Measure Up/Pressure Down National Hypertension Campaign
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Acronym Blood Transfusion 231 Major Trauma 234 Maternal
Cambridge University Press 978-0-521-26827-1 - Obstetric and Intrapartum Emergencies: A Practical Guide to Management Edwin Chandraharan and Sir Sabaratnam Arulkumaran Index More information Index ABCDE acronym albumin, blood plasma levels 7 arterial blood gas (ABG) 188 blood transfusion 231 allergic anaphylaxis 229 arterio-venous occlusions 166–167 major trauma 234 maternal collapse 12, 130–131 amiadarone, overdose 178 aspiration 10, 246 newborn infant 241 amniocentesis 234 aspirin 26, 180–181 resuscitation 127–131 amniotic fluid embolism 48–51 assisted reproduction 93 abdomen caesarean section 257 asthma 4, 150, 151, 152, 185 examination after trauma 234 massive haemorrhage 33 pain in pregnancy 154–160, 161 maternal collapse 10, 13, 128 atracurium, drug reactions 231 accreta, placenta 250, 252, 255 anaemia, physiological 1, 7 atrial fibrillation 205 ACE inhibitors, overdose 178 anaerobic metabolism 242 automated external defibrillator (AED) 12 acid–base analysis 104 anaesthesia. See general anaesthesia awareness under anaesthesia 215, 217 acidosis 94, 180–181, 186, 242 anal incontinence 138–139 ACTH levels 210 analgesia 11, 100, 218 barbiturates, overdose 178 activated charcoal 177, 180–181 anaphylaxis 11, 227–228, 229–231 behaviour/beliefs, psychiatric activated partial thromboplastin time antacid prophylaxis 217 emergencies 172 (APTT) 19, 21 antenatal screening, DVT 16 benign intracranial hypertension 166 activated protein C 46 antepartum haemorrhage 33, 93–94. benzodiazepines, overdose 178 Addison’s disease 208–209 See also massive -

Thyroid Disease in the Perinatal Period
Thyroid Thyroid disease in Simon Forehan the perinatal period Background Thyroid dysfunction affects 2–3% of pregnant women and Thyroid hormone plays a critical role in fetal development. In one in 10 women of childbearing age with normal thyroid pregnancy, increased thyroid hormone synthesis is required to function have underlying thyroid autoimmunity, which may meet fetal needs, resulting in increased iodine requirements. indicate reduced functional reserve.1 Up to 18% of women in Objective the first trimester in Australia are thyroid antibody positive.2 This article outlines changes to thyroid physiology and Thyroid hormone plays a critical role in pregnancy and iodine requirements in pregnancy, pregnancy specific understanding the unique changes to thyroid physiology in reference ranges for thyroid function tests and detection and pregnancy has important implications for the definition and management of thyroid conditions in pregnancy. treatment of thyroid disorders in pregnancy. Discussion Thyroid dysfunction affects 2–3% of pregnant women. Pregnancy specific reference ranges are required to define Thyroid physiology and pregnancy thyroid conditions in pregnancy and to guide treatment. The fetus is dependent on transplacental transfer of maternal thyroxine Overt maternal hypothyroidism is associated with adverse (T4). Deiodination of maternal T4 by the fetus results in local fetal pregnancy outcomes; thyroxine treatment should be production of liothyronine (T3), which is particularly important for commenced immediately in this condition. Thyroxine neurological development.3,4 Maternal T3 does not cross the placenta treatment has also been shown to be effective for pregnant and appears to have little, if any, role in development. Other changes in women with subclinical hypothyroidism who are thyroid pregnancy include an increase in thyroid binding globulin (TBG), resulting peroxidase antibody positive. -

Ask the Experts Amniotic Fluid Embolism Steven L. Clark, MD
Ask the Experts Questions have been written by: Amniotic Fluid Embolism Angela K. Hardyk, MD Mount Nittany Physician Group Ob/Gyn Steven L. Clark, MD State College, PA (Obstet Gynecol 2014;123:337–48) Responses have been written by: Steven L. Clark, MD Hospital Corporation of America Nashville, TN Question 1: How would you counsel a patient about a future pregnancy if she has been lucky enough to survive an amniotic fl uid embolism (AFE)? Would there be any special precautions she would need to take for her next pregnancy? Response from Dr. Clark: The available data in this area consist only of several very small series and case reports. These data suggest that the risks of recurrence are low. In addition, a pathophysiologic mechanism of disease that hinges on a maternal reaction to a specif- ic set of fetal antigens would suggest that recurrence ought to be uncommon. On the other hand, having dodged one bullet, is it really wise to spin the wheel again? My counseling goes something like this: “Available data suggest that the risk of recurrence is low, and there are a number of reports of successful pregnancy outcome after AFE survival. However, given the potential severity of AFE if it does recur, and a lack of really good data regarding risks, I advise you to undertake another pregnancy only if you are willing to accept a small risk of catastrophic outcome including death.” If a patient chooses to undertake pregnancy, I do not alter my management in any way, other than delivery in a tertiary center. -

Management of Prolonged Decelerations ▲
OBG_1106_Dildy.finalREV 10/24/06 10:05 AM Page 30 OBGMANAGEMENT Gary A. Dildy III, MD OBSTETRIC EMERGENCIES Clinical Professor, Department of Obstetrics and Gynecology, Management of Louisiana State University Health Sciences Center New Orleans prolonged decelerations Director of Site Analysis HCA Perinatal Quality Assurance Some are benign, some are pathologic but reversible, Nashville, Tenn and others are the most feared complications in obstetrics Staff Perinatologist Maternal-Fetal Medicine St. Mark’s Hospital prolonged deceleration may signal ed prolonged decelerations is based on bed- Salt Lake City, Utah danger—or reflect a perfectly nor- side clinical judgment, which inevitably will A mal fetal response to maternal sometimes be imperfect given the unpre- pelvic examination.® BecauseDowden of the Healthwide dictability Media of these decelerations.” range of possibilities, this fetal heart rate pattern justifies close attention. For exam- “Fetal bradycardia” and “prolonged ple,Copyright repetitive Forprolonged personal decelerations use may onlydeceleration” are distinct entities indicate cord compression from oligohy- In general parlance, we often use the terms dramnios. Even more troubling, a pro- “fetal bradycardia” and “prolonged decel- longed deceleration may occur for the first eration” loosely. In practice, we must dif- IN THIS ARTICLE time during the evolution of a profound ferentiate these entities because underlying catastrophe, such as amniotic fluid pathophysiologic mechanisms and clinical 3 FHR patterns: embolism or uterine rupture during vagi- management may differ substantially. What would nal birth after cesarean delivery (VBAC). The problem: Since the introduction In some circumstances, a prolonged decel- of electronic fetal monitoring (EFM) in you do? eration may be the terminus of a progres- the 1960s, numerous descriptions of FHR ❙ Complete heart sion of nonreassuring fetal heart rate patterns have been published, each slight- block (FHR) changes, and becomes the immedi- ly different from the others. -

Ante Partum Haemorrhage
Ante Partum Haemorrhage Sara Alhaddab Alanood Asiri Ante Partum Haemorrhage (APH): Bleeding in early pregnancy (first 20 weeks of gestation) causes: Affects 3-5 % of pregnancies. • - Miscarriage • Bleeding from or into the genital tract. - Ectopic pregnancy • Occurring from 20 weeks of pregnancy and prior - Molar pregnancy to the birth of the baby. - Local causes: tumor, trauma etc. Causes: Landmark of fetal viability is 20 weeks. • Placenta previa. • Placenta abruption. • Local causes (cervical or vaginal lesions, lacerations). Trauma, tumor and infections. • Unexplained (SGA, IUGR). SGA: small for gestational age. • Vasa previa. • Uterine rupture. - APH is the leading cause of prenatal and maternal morbidity and prenatal mortality (mainly prematurity). - Obstetrics hemorrhage remains one of the major causes of maternal death in the developing countries. Management: In the hospital maternity unit with facilities for resuscitation such as: Source: Essentials of Obstetrics and Gynecology. § Anesthetic support. § Blood transfusion resources. § Performing emergency operative delivery. § Multidisciplinary team including (midwifery, obstetric staff, neonatal and anesthetic). Investigations: • Tests if suspecting vasa previa are often not applicable • Tocolysis: shouldn’t be used in: v Unstable patient. v Fetal compromise. v Major APH. It’s a decision of a senior obstetrician. Senior (consultant) anesthetic care needed in high-risk hemorrhage. • Risk of PPH: patient should receive active management of 3rd stage of labor using syntometrine (in absence of high BP). Syntometrine → active uterine contraction after delivery to prevent PPH. • AntiD Ig should be given to all non sensitized RH –ve if the have APH, at least 500 IU AntiD Ig followed by a test of FMH if it is more than 40 ml of RBC additional AntiD required. -

MFM Clinical Guideline
MFM Clinical Guideline Thyroid Disease in Pregnancy Thyroid disease is the 2nd most common endocrinopathy in pregnancy after diabetes. In pregnancy: thyroid volume ↑ 30%, total/bound T3 and T4 levels ↑, but free/unbound T3 and T4 levels are stable due to ↑ thyroid binding globulin. In the 1st trimester, TSH levels ↓ due to high levels of hCG,which directly stimulates the TSH receptor, but return to baseline in the 2nd trimester. TSH does not cross the placenta. Maternal T4 is transferred to the fetus and is important for fetal brain development, especially before the fetal thyroid gland begins to synthesize thyroid hormone at 12-14 weeks. Screening for Thyroid Disease in Pregnancy Table 1: Screening. Table 2: Pregnancy reference ranges. Who to Screen Trimester TSH FT4* Age > 30 1st 0.1 - 2.5 0.8 - 1.2 BMI > 40 mIU/L ng/dL Current signs/symptoms of thyroid dysfunction 2nd 0.2 - 3 mIU/L 0.6 - 1 ng/dL Known positive thyroid antibodies 3rd 0.3 - 3 mIU/L 0.5 - 0.8 ng.dL Goiter *Due to inaccuracy of thyroid testing in pregnancy, Hx head/neck irradiation or thyroid surgery FT4 goal FHx thyroid disease should be the upper half of the reference range Pregestational diabetes Table 3: Interpreting the results. Autoimmune disorders TSH FT4 Hx of pregnancy loss, PTD, infertility Use of amiodarone or lithium, recent administration of Overt Hyperthyroidism ↓ ↑ iodinated radiologic contrast Subclinical ↓ NL Hyperthyroidism Residing in an area of known iodine deficiency Gestational 1st trim: ↓ UL How to Screen Hyperthyroidism 2nd trim: NL/ Step 1: TSH, -

Critical Care Issues in Pregnancy
CriticalCritical CareCare IssuesIssues inin PregnancyPregnancy Miren A. Schinco, MD, FCCS, FCCM Associate Professor of Surgery University of Florida College of Medicine, Jacksonville College of Medicine – Jacksonville Department of Surgery EpidemiologyEpidemiology •Approximately .1% of deliveries result in ICU admission • Generally, 75% - 80 % are during the post- partum period College of Medicine – Jacksonville Department of Surgery TopTop causescauses ofof mortalitymortality inin obstetricobstetric patientspatients admittedadmitted toto thethe ICUICU Etiology N (of 1354) Percentage Hypertension 20 21.5 Pulmonary 20 21.5 Cardiac 11 11.8 Hemorrhage 8 8.6 CNS 8 8.6 Sepsis/Infection 6 6.4 Malignancy 6 6.4 College of Medicine – Jacksonville Department of Surgery CriticalCritical illnessesillnesses inin pregnancypregnancy A. Conditions unique to pregnancy: account for 50-80% admissions to ICU(account for > 50% ICU admissions): • Preeclampsia / Eclampsia • HELLP syndrome • Acute fatty liver of pregnancy • Amniotic fluid embolism • Peri-partum cardiomyopathy • Puerperal sepsis • Thrombotic disease • Obstetric hemorrhage College of Medicine – Jacksonville Department of Surgery CriticalCritical illnessesillnesses inin pregnancypregnancy B. Pre-existing conditions that may worsen during pregnancy (account for 20-50% ICU admissions): • Cardiovascular: valvular disease, Eisenmenger’s syndrome, cyanotic congenital heart disease, coarctation of aorta, PPH • Renal: glomerulonephritis, chronic renal insufficiency • Hematologic: sickle cell disease, -

Management of Endocrinopathies in Pregnancy: a Review of Current Evidence
International Journal of Environmental Research and Public Health Review Management of Endocrinopathies in Pregnancy: A Review of Current Evidence Daniela Calina 1,† , Anca Oana Docea 2,*,†, Kirill Sergeyevich Golokhvast 3,†, Stavros Sifakis 4, Aristides Tsatsakis 5 and Antonis Makrigiannakis 6 1 Department of Clinical Pharmacy, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania; [email protected] 2 Department of Toxicology, University of Medicine and Pharmacy of Craiova, 200349 Craiova, Romania 3 Scientific Education Center of Nanotechnology, Far Eastern Federal University, Vladivostok 690950, Russia; [email protected] 4 Department of Obstetrics and Gynecology, Mitera Maternity Hospital, 71110 Heraklion, Crete, Greece; [email protected] 5 Department of Forensic Sciences and Toxicology, Faculty of Medicine, University of Crete, 71110 Heraklion, Crete, Greece; [email protected] 6 Department of Obstetrics and Gynecology, Medical School, University of Crete, 71110 Heraklion, Crete, Greece; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Received: 28 January 2019; Accepted: 27 February 2019; Published: 4 March 2019 Abstract: Pregnancy in women with associated endocrine conditions is a therapeutic challenge for clinicians. These disorders may be common, such us thyroid disorders and diabetes, or rare, including adrenal and parathyroid disease and pituitary dysfunction. With the development of assisted reproductive techniques, the number of pregnancies with these conditions has increased. It is necessary to recognize symptoms and correct diagnosis for a proper pharmacotherapeutic management in order to avoid adverse side effects both in mother and fetus. This review summarizes the pharmacotherapy of these clinical situations in order to reduce maternal and fetal morbidity. -

Amnioinfusion
Review Article Indian Journal of Obstetrics and Gynecology Volume 7 Number 4 (Part - II), October – December 2019 DOI: http://dx.doi.org/10.21088/ijog.2321.1636.7419.12 Amnioinfusion Alka Patil1, Sayli Thavare2, Bhagyashree Badade3 How to cite this article: Alka Patil, Sayli Thavare, Bhagyashree Badade. Amnioinfusion. Indian J Obstet Gynecol. 2019;7(4)(Part-II):641–644. 1Professor and Head, 2,3Junior Resident, Department of Obstetrics and Gynaecology, ACPM Medical College, Dhule, Maharashtra 424002, India. Corresponding Author: Alka Patil, Professor and Head, Department of Obstetrics and Gynaecology, ACPM Medical College, Dhule, Maharashtra 424002, India. E-mail: [email protected] Received on 20.11.2019; Accepted on 16.12.2019 Abstract potentially at risk. Oligohydramnios is one of the high-risk pregnancy, posing diagnostic challenge Amniotic fluid is a dynamic medium that plays and dilemma in management. These high-risk a significant role in fetal well-being. It is essential pregnancies should be monitored, managed during pregnancy for normal fetal growth and organ and delivered at a tertiary care center for good development. About 4% of pregnancies are complicated pregnancy outcome. by oligohydramnios. It is associated with an increased incidence of perinatal morbidity and mortality due to its Amniotic fl uid is essential for the continued well antepartum and intrapartum complications. Gerbruch being of the fetus and has following functions: and Hansman described a technique of Amnioinfusion • Shock absorber preventing hazardous to overcome these difficulties to prevent the occurrence pressure on the fetal parts of fetal lung hypoplasia in pregnancies complicated by oligohydramnios. Amnioinfusion reduces both • Prevents adhesion formation between fetal the frequency and depth of FHR deceleration. -
Postpartum Thyroiditis
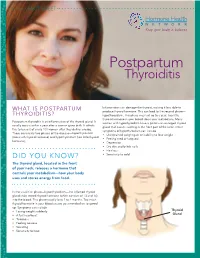
FACT SHEET Postpartum Thyroiditis Inflammation can damage the thyroid, making it less able to WHAT IS POSTPARTUM produce thyroid hormone. This can lead to the second phase— THYROIDITIS? hypothyroidism. This phase may last up to a year. Too little thyroid hormone in your blood slows your metabolism. Many Postpartum thyroiditis is an inflammation of the thyroid gland. It women with hypothyroidism have a goiter—an enlarged thyroid usually occurs within a year after a woman gives birth. It affects gland that causes swelling in the front part of the neck. Other five to ten out of every 100 women after they deliver a baby. symptoms of hypothyroidism can include There are usually two phases of the disease—hyperthyroidism • Unexplained weight gain or inability to lose weight (too much thyroid hormone) and hypothyroidism (too little thyroid • Feeling tired or fatigued hormone). • Depression • Dry skin and brittle nails • Hair loss DID YOU KNOW? • Sensitivity to cold The thyroid gland, located in the front of your neck, releases a hormone that controls your metabolism—how your body uses and stores energy from food. In the usual first phase—hyperthyroidism—the inflamed thyroid gland leaks stored thyroid hormone (which consists of T3 and T4) into the blood. This phase usually lasts 2 to 4 months. Too much thyroid hormone in your blood causes your metabolism to speed up. Symptoms can include • Losing weight suddenly Thyroid • A fast heartbeat Gland • Tiredness • Feeling nervous • Sweating • Sensitivity to heat WHAT ARE THE RISKS OF POSTPARTUM THYROIDITIS? Questions to ask your doctor You are at greater risk of developing postpartum thyroiditis if you have an immune system disorder such as type 1 diabetes, a • Do my symptoms mean I might have personal or family history of thyroid disease, or had postpartum postpartum thyroiditis? thyroiditis before. -

High Risk L&D
High Risk L&D, pg 1 of 12 Taking care of patients who have non-reasurring pattern • A non-reassuring pattern is: • no variability • less than 2 accelerations • decelerations • In antepartum setting, you are looking at variable and accelerations • Parameters for 28-32 weeks is different than 32 weeks or greater • What about in labor? • looking for late decels (these are bad) • variability is THE most important thing! • moderate variability shows the CNS is intact • absent variability is no bueno...this would be a big issue if it was moderate before and now has become absent. If pt had medication, then this may not be so much of a concern b/c the meds affects the baby. • minimal may be bad (probably is) • marked is also not good • Category 1: has variablity, maybe a random decel (but most likely none), has accelerations • Category 2: starting to get into a little gray area; physician can proceed forward with usual plan of care; moderate or minimal variability; may have recurring decels (of any type); • Category3 : absent or minimal variability with repetitive late decels; baby is not coping • What’s the first thing you would do if pt had repetitive variable decels? • reposition, increase IV, put Oxygen on mom, call doc (You will reposition b/c the variable decels are d/t cord compression). • You would give O2 if she had decreased variability (according to Dr. Ferguson) • Baby can get late decels from mom lying on her back (so position change), or from having low BP (so give IV bolus). Things you need for precipitous birth • IV • Oxygen • BOA kit (Birth on Arrival kit) What kind of risks are involved with precipitous birth? • Tearing at perineum • Hemorrhage d/t lacerations and such • Pneumothorax (not in boook!). -

Shoulder Dystocia Abnormal Placentation Umbilical Cord
Obstetric Emergencies Shoulder Dystocia Abnormal Placentation Umbilical Cord Prolapse Uterine Rupture TOLAC Diabetic Ketoacidosis Valerie Huwe, RNC-OB, MS, CNS & Meghan Duck RNC-OB, MS, CNS UCSF Benioff Children’s Hospital Outreach Services, Mission Bay Objectives .Highlight abnormal conditions that contribute to the severity of obstetric emergencies .Describe how nurses can implement recommended protocols, procedures, and guidelines during an OB emergency aimed to reduce patient harm .Identify safe-guards within hospital systems aimed to provide safe obstetric care .Identify triggers during childbirth that increase a women’s risk for Post Traumatic Stress Disorder and Postpartum Depression . Incorporate a multidisciplinary plan of care to optimize care for women with postpartum emergencies Obstetric Emergencies • Shoulder Dystocia • Abnormal Placentation • Umbilical Cord Prolapse • Uterine Rupture • TOLAC • Diabetic Ketoacidosis Risk-benefit analysis Balancing 2 Principles 1. Maternal ‒ Benefit should outweigh risk 2. Fetal ‒ Optimal outcome Case Presentation . 36 yo Hispanic woman G4 P3 to L&D for IOL .IVF Pregnancy .3 Prior vaginal births: 7.12, 8.1, 8.5 (NCB) .Late to care – EDC ~ 40-41 weeks .GDM Type A2 – somewhat uncontrolled .4’11’’ .Hx of Lupus .BMI 40 .Gained ~ 40 lbs during pregnancy Question: What complication is she a risk for? a) Placental abruption b) Thyroid Storm c) Preeclampsia with severe features d) Shoulder dystocia e) Uterine prolapse Case Presentation . 36 yo Hispanic woman G4 P3 to L&D for IOL .IVF Pregnancy .3