Shoulder Dystocia Abnormal Placentation Umbilical Cord
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
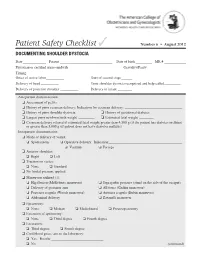
Documenting Shoulder Dystocia
Patient Safety Checklist ✓ Number 6 • August 2012 DOCUMENTING SHOULDER DYSTOCIA Date _____________ Patient _____________________________ Date of birth _________ MR # ____________ Physician or certified nurse–midwife _____________________________ Gravidity/Parity______________________ Timing: Onset of active labor __________ Start of second stage ______ Delivery of head __________ Time shoulder dystocia recognized and help called _________ Delivery of posterior shoulder __________ Delivery of infant ________ Antepartum documentation: ❏ Assessment of pelvis ❏ History of prior cesarean delivery: Indication for cesarean delivery: ________________________________ ❏ History of prior shoulder dystocia ❏ History of gestational diabetes ❏ Largest prior newborn birth weight _________ ❏ Estimated fetal weight ________ ❏ Cesarean delivery offered if estimated fetal weight greater than 4,500 g (if the patient has diabetes mellitus) or greater than 5,000 g (if patient does not have diabetes mellitus) Intrapartum documentation: ❏ Mode of delivery of vertex: ❏ Spontaneous ❏ Operative delivery: Indication: _________________________________________ ❏ Vacuum ❏ Forceps ❏ Anterior shoulder: ❏ Right ❏ Left ❏ Traction on vertex: ❏ None ❏ Standard ❏ No fundal pressure applied ❏ Maneuvers utilized (1): ❏ Hip flexion (McRoberts maneuver) ❏ Suprapubic pressure (stand on the side of the occiput) ❏ Delivery of posterior arm ❏ All fours (Gaskin maneuver) ❏ Posterior scapula (Woods maneuver) ❏ Anterior scapula (Rubin maneuver) ❏ Abdominal delivery ❏ Zavanelli maneuver -

ABCDE Acronym Blood Transfusion 231 Major Trauma 234 Maternal
Cambridge University Press 978-0-521-26827-1 - Obstetric and Intrapartum Emergencies: A Practical Guide to Management Edwin Chandraharan and Sir Sabaratnam Arulkumaran Index More information Index ABCDE acronym albumin, blood plasma levels 7 arterial blood gas (ABG) 188 blood transfusion 231 allergic anaphylaxis 229 arterio-venous occlusions 166–167 major trauma 234 maternal collapse 12, 130–131 amiadarone, overdose 178 aspiration 10, 246 newborn infant 241 amniocentesis 234 aspirin 26, 180–181 resuscitation 127–131 amniotic fluid embolism 48–51 assisted reproduction 93 abdomen caesarean section 257 asthma 4, 150, 151, 152, 185 examination after trauma 234 massive haemorrhage 33 pain in pregnancy 154–160, 161 maternal collapse 10, 13, 128 atracurium, drug reactions 231 accreta, placenta 250, 252, 255 anaemia, physiological 1, 7 atrial fibrillation 205 ACE inhibitors, overdose 178 anaerobic metabolism 242 automated external defibrillator (AED) 12 acid–base analysis 104 anaesthesia. See general anaesthesia awareness under anaesthesia 215, 217 acidosis 94, 180–181, 186, 242 anal incontinence 138–139 ACTH levels 210 analgesia 11, 100, 218 barbiturates, overdose 178 activated charcoal 177, 180–181 anaphylaxis 11, 227–228, 229–231 behaviour/beliefs, psychiatric activated partial thromboplastin time antacid prophylaxis 217 emergencies 172 (APTT) 19, 21 antenatal screening, DVT 16 benign intracranial hypertension 166 activated protein C 46 antepartum haemorrhage 33, 93–94. benzodiazepines, overdose 178 Addison’s disease 208–209 See also massive -

Incidence of Eclampsia with HELLP Syndrome and Associated Mortality in Latin America
International Journal of Gynecology and Obstetrics 129 (2015) 219–222 Contents lists available at ScienceDirect International Journal of Gynecology and Obstetrics journal homepage: www.elsevier.com/locate/ijgo CLINICAL ARTICLE Incidence of eclampsia with HELLP syndrome and associated mortality in Latin America Paulino Vigil-De Gracia a,⁎, José Rojas-Suarez b, Edwin Ramos c, Osvaldo Reyes d, Jorge Collantes e, Arelys Quintero f,ErasmoHuertasg, Andrés Calle h, Eduardo Turcios i,VicenteY.Chonj a Critical Care Unit, Department of Obstetrics and Gynecology, Complejo Hospitalario de la Caja de Seguro Social, Panama City, Panama b Critical Care Unit, Clínica de Maternidad Rafael Calvo, Cartagena, Colombia c Department of Gynecology and Obstetrics, Hospital Universitario Dr Luis Razetti, Barcelona, Venezuela d Unit of Research, Department of Gynecology and Obstetrics, Hospital Santo Tomás, Panama City, Panama e Department of Gynecology and Obstetrics, Hospital Regional de Cojamarca, Cajamarca, Peru f Department of Gynecology and Obstetrics, Hospital José Domingo de Obaldía, David, Panama g Unit of Perinatology, Department of Gynecology and Obstetrics, Instituto Nacional Materno Perinatal, Lima, Peru h Department of Gynecology and Obstetrics, Hospital Carlos Andrade Marín, Quito, Ecuador i Unit of Research, Department of Gynecology and Obstetrics, Hospital Primero de Mayo de Seguridad Social, San Salvador, El Salvador j Department of Gynecology and Obstetrics, Hospital Teodoro Maldonado Carbo, Guayaquil, Ecuador article info abstract Article history: Objective: To describe the maternal outcome among women with eclampsia with and without HELLP syndrome Received 7 July 2014 (hemolysis, elevated liver enzymes, and low platelet count). Methods: A cross-sectional study of women with Received in revised form 14 November 2014 eclampsia was undertaken in 14 maternity units in Latin America between January 1 and December 31, 2012. -

Ask the Experts Amniotic Fluid Embolism Steven L. Clark, MD
Ask the Experts Questions have been written by: Amniotic Fluid Embolism Angela K. Hardyk, MD Mount Nittany Physician Group Ob/Gyn Steven L. Clark, MD State College, PA (Obstet Gynecol 2014;123:337–48) Responses have been written by: Steven L. Clark, MD Hospital Corporation of America Nashville, TN Question 1: How would you counsel a patient about a future pregnancy if she has been lucky enough to survive an amniotic fl uid embolism (AFE)? Would there be any special precautions she would need to take for her next pregnancy? Response from Dr. Clark: The available data in this area consist only of several very small series and case reports. These data suggest that the risks of recurrence are low. In addition, a pathophysiologic mechanism of disease that hinges on a maternal reaction to a specif- ic set of fetal antigens would suggest that recurrence ought to be uncommon. On the other hand, having dodged one bullet, is it really wise to spin the wheel again? My counseling goes something like this: “Available data suggest that the risk of recurrence is low, and there are a number of reports of successful pregnancy outcome after AFE survival. However, given the potential severity of AFE if it does recur, and a lack of really good data regarding risks, I advise you to undertake another pregnancy only if you are willing to accept a small risk of catastrophic outcome including death.” If a patient chooses to undertake pregnancy, I do not alter my management in any way, other than delivery in a tertiary center. -

Vitamin D, Pre-Eclampsia, and Preterm Birth Among Pregnancies at High Risk for Pre-Eclampsia: an Analysis of Data from a Low-Dos
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author BJOG. Author Manuscript Author manuscript; Manuscript Author available in PMC 2021 January 29. Published in final edited form as: BJOG. 2017 November ; 124(12): 1874–1882. doi:10.1111/1471-0528.14372. Vitamin D, pre-eclampsia, and preterm birth among pregnancies at high risk for pre-eclampsia: an analysis of data from a low- dose aspirin trial AD Gernanda, HN Simhanb, KM Bacac, S Caritisd, LM Bodnare aDepartment of Nutritional Sciences, The Pennsylvania State University, University Park, PA, USA bDivision of Maternal-Fetal Medicine, Magee-Women’s Hospital and Department of Obstetrics, Gynecology and Reproductive Sciences, School of Medicine, University of Pittsburgh, Pittsburgh, PA, USA cDepartment of Epidemiology, University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA, USA dDepartment of Obstetrics, Gynecology and Reproductive Sciences and Department of Pediatrics, School of Medicine, University of Pittsburgh, Pittsburgh, PA, USA eDepartments of Epidemiology and Obstetrics, Gynecology and Reproductive Sciences, University of Pittsburgh Graduate School of Public Health and School of Medicine, Pittsburgh, PA, USA Abstract Objective—To examine the relation between maternal vitamin D status and risk of pre-eclampsia and preterm birth in women at high risk for pre-eclampsia. Design—Analysis of prospectively collected data and blood samples from a trial of prenatal low- dose aspirin. Setting—Thirteen sites across the USA. Population—Women at high risk for pre-eclampsia. Methods—We measured 25-hydroxyvitamin D [25(OH)D] concentrations in stored maternal serum samples drawn at 12–26 weeks’ gestation (n = 822). We used mixed effects models to Correspondence: LM Bodnar, University of Pittsburgh Graduate School of Public Health, A742 Crabtree Hall, 130 DeSoto St, Pittsburgh, PA 15261, USA. -

Policy of Interventionist Versus Expectant Management of Severe
WHO recommendations Policy of interventionist versus expectant management of severe pre-eclampsia before term WHO recommendations Policy of interventionist versus expectant management of severe pre-eclampsia before term WHO recommendations: policy of interventionist versus expectant management of severe pre-eclampsia before term ISBN 978-92-4-155044-4 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. WHO recommendations: policy of interventionist versus expectant management of severe pre-eclampsia before term. Geneva: World Health Organization; 2018. -

Management of Prolonged Decelerations ▲
OBG_1106_Dildy.finalREV 10/24/06 10:05 AM Page 30 OBGMANAGEMENT Gary A. Dildy III, MD OBSTETRIC EMERGENCIES Clinical Professor, Department of Obstetrics and Gynecology, Management of Louisiana State University Health Sciences Center New Orleans prolonged decelerations Director of Site Analysis HCA Perinatal Quality Assurance Some are benign, some are pathologic but reversible, Nashville, Tenn and others are the most feared complications in obstetrics Staff Perinatologist Maternal-Fetal Medicine St. Mark’s Hospital prolonged deceleration may signal ed prolonged decelerations is based on bed- Salt Lake City, Utah danger—or reflect a perfectly nor- side clinical judgment, which inevitably will A mal fetal response to maternal sometimes be imperfect given the unpre- pelvic examination.® BecauseDowden of the Healthwide dictability Media of these decelerations.” range of possibilities, this fetal heart rate pattern justifies close attention. For exam- “Fetal bradycardia” and “prolonged ple,Copyright repetitive Forprolonged personal decelerations use may onlydeceleration” are distinct entities indicate cord compression from oligohy- In general parlance, we often use the terms dramnios. Even more troubling, a pro- “fetal bradycardia” and “prolonged decel- longed deceleration may occur for the first eration” loosely. In practice, we must dif- IN THIS ARTICLE time during the evolution of a profound ferentiate these entities because underlying catastrophe, such as amniotic fluid pathophysiologic mechanisms and clinical 3 FHR patterns: embolism or uterine rupture during vagi- management may differ substantially. What would nal birth after cesarean delivery (VBAC). The problem: Since the introduction In some circumstances, a prolonged decel- of electronic fetal monitoring (EFM) in you do? eration may be the terminus of a progres- the 1960s, numerous descriptions of FHR ❙ Complete heart sion of nonreassuring fetal heart rate patterns have been published, each slight- block (FHR) changes, and becomes the immedi- ly different from the others. -

Ante Partum Haemorrhage
Ante Partum Haemorrhage Sara Alhaddab Alanood Asiri Ante Partum Haemorrhage (APH): Bleeding in early pregnancy (first 20 weeks of gestation) causes: Affects 3-5 % of pregnancies. • - Miscarriage • Bleeding from or into the genital tract. - Ectopic pregnancy • Occurring from 20 weeks of pregnancy and prior - Molar pregnancy to the birth of the baby. - Local causes: tumor, trauma etc. Causes: Landmark of fetal viability is 20 weeks. • Placenta previa. • Placenta abruption. • Local causes (cervical or vaginal lesions, lacerations). Trauma, tumor and infections. • Unexplained (SGA, IUGR). SGA: small for gestational age. • Vasa previa. • Uterine rupture. - APH is the leading cause of prenatal and maternal morbidity and prenatal mortality (mainly prematurity). - Obstetrics hemorrhage remains one of the major causes of maternal death in the developing countries. Management: In the hospital maternity unit with facilities for resuscitation such as: Source: Essentials of Obstetrics and Gynecology. § Anesthetic support. § Blood transfusion resources. § Performing emergency operative delivery. § Multidisciplinary team including (midwifery, obstetric staff, neonatal and anesthetic). Investigations: • Tests if suspecting vasa previa are often not applicable • Tocolysis: shouldn’t be used in: v Unstable patient. v Fetal compromise. v Major APH. It’s a decision of a senior obstetrician. Senior (consultant) anesthetic care needed in high-risk hemorrhage. • Risk of PPH: patient should receive active management of 3rd stage of labor using syntometrine (in absence of high BP). Syntometrine → active uterine contraction after delivery to prevent PPH. • AntiD Ig should be given to all non sensitized RH –ve if the have APH, at least 500 IU AntiD Ig followed by a test of FMH if it is more than 40 ml of RBC additional AntiD required. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

Ophthalmic Associations in Pregnancy
CLINICAL Ophthalmic associations in pregnancy Queena Qin, Celia Chen, Sudha Cugati PREGNANCY RESULTS in various physiological variation in pregnancy.2 It normally changes in the female body, including in fades slowly after pregnancy and does the eyes. A typical pregnancy results in not need active intervention. Background A range of ocular pathology exists cardiovascular, pulmonary, metabolic, • Cornea – corneal thickness, curvature during pregnancy. Some pre-existing eye hormonal and immunological changes. and sensitivity may be altered during conditions, such as diabetic retinopathy, Hormonal changes occur, with a rise of pregnancy. Corneal thickness and can be exacerbated during pregnancy. oestrogen and progesterone levels to curvature can increase in pregnancy, Other conditions manifest for the first suppress the menstrual cycle.1 especially in the second and third time during pregnancy as a result of The eye, an end organ, undergoes trimesters, and return to normal in complications such as pre-eclampsia changes during pregnancy. Some of the postpartum period.3 Patients who and eclampsia. Early recognition and understanding of the management of these changes exacerbate pre-existing wear contact lenses may experience ophthalmic conditions is crucial. eye conditions, while other conditions intolerance to the use of contact lenses. manifest for the first time during Pregnant women should be advised Objective pregnancy. Early recognition and to delay obtaining a new prescription The aim of this article is to discuss the understanding of management of for glasses or undergoing a contact physiological and pathological changes in the eyes of pregnant women. ophthalmic conditions during pregnancy lens fitting until after delivery. Laser Pathological changes are sub-divided is crucial for the primary care physician. -

Critical Care Issues in Pregnancy
CriticalCritical CareCare IssuesIssues inin PregnancyPregnancy Miren A. Schinco, MD, FCCS, FCCM Associate Professor of Surgery University of Florida College of Medicine, Jacksonville College of Medicine – Jacksonville Department of Surgery EpidemiologyEpidemiology •Approximately .1% of deliveries result in ICU admission • Generally, 75% - 80 % are during the post- partum period College of Medicine – Jacksonville Department of Surgery TopTop causescauses ofof mortalitymortality inin obstetricobstetric patientspatients admittedadmitted toto thethe ICUICU Etiology N (of 1354) Percentage Hypertension 20 21.5 Pulmonary 20 21.5 Cardiac 11 11.8 Hemorrhage 8 8.6 CNS 8 8.6 Sepsis/Infection 6 6.4 Malignancy 6 6.4 College of Medicine – Jacksonville Department of Surgery CriticalCritical illnessesillnesses inin pregnancypregnancy A. Conditions unique to pregnancy: account for 50-80% admissions to ICU(account for > 50% ICU admissions): • Preeclampsia / Eclampsia • HELLP syndrome • Acute fatty liver of pregnancy • Amniotic fluid embolism • Peri-partum cardiomyopathy • Puerperal sepsis • Thrombotic disease • Obstetric hemorrhage College of Medicine – Jacksonville Department of Surgery CriticalCritical illnessesillnesses inin pregnancypregnancy B. Pre-existing conditions that may worsen during pregnancy (account for 20-50% ICU admissions): • Cardiovascular: valvular disease, Eisenmenger’s syndrome, cyanotic congenital heart disease, coarctation of aorta, PPH • Renal: glomerulonephritis, chronic renal insufficiency • Hematologic: sickle cell disease, -

Pre-Eclampsia and High Blood Pressure During Pregnancy
Pre-eclampsia and High Blood Pressure During Pregnancy What is high blood pressure? A blood pressure measurement is usually recorded as two numbers, Blood pressure is the force that pushes against your blood vessel such as 120 over 80 (120/80). High blood pressure is also called walls each time your heart squeezes and relaxes to pump the blood hypertension. Hypertension is diagnosed when either the top or the through your body. Blood pressure measurement is a very useful bottom number is higher than normal. way to monitor the health of your cardiovascular system (heart and blood vessels). Why is blood pressure important develops, it does not go away until after the baby is born. Women with pre-eclampsia may require an earlier delivery, during pregnancy? either by labour induction or caesarean section, in order to During pregnancy, very high blood pressure (severe hypertension) protect the health of themselves and their baby. In some cases, can cause complications for both you and your baby, including: pre-eclampsia can develop after childbirth and you should • Poor growth of your baby – due to low nutrition and oxygen alert your doctor or midwife of any concerns you may have supply from the placenta after your baby is born. • Prematurity – if early delivery (before 37 weeks) is required to protect the health of you or your baby • Placental abruption – the placenta may prematurely separate from the wall of the uterus (womb), leading to bleeding and the need for an emergency birth in some cases • Pre-eclampsia – a condition involving high blood pressure and abnormal function in one or more organs during pregnancy What are the different types of high blood pressure that affect pregnant women? 1.