Report on Mapping of Healthcare Sector in India
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
How Does Eye Care Seeking Behaviour Change with Increasing Age and Visual Impairment? Intersectional Analysis of Older Adults In
Barman and Mishra BMC Geriatrics (2020) 20:71 https://doi.org/10.1186/s12877-020-1438-y RESEARCH ARTICLE Open Access How does eye care seeking behaviour change with increasing age and visual impairment? Intersectional analysis of older adults in the Indian Sundarbans Debjani Barman* and Manasee Mishra Abstract Background: Visual impairment disproportionately affects people in the low-income countries. A high proportion of visual impairment can be prevented or cured. Yet, care seeking for eye health is restricted for women and older adults. This article uses the intersectionality approach to understand how eye care seeking behaviour changes in men and women with increase in age and visual impairment in a poor and underserved region of India. It brings forth the commonalities and differences between the various groups. Methods: The article is based on qualitative data. Persons aged 50 years and more are categorized into young-old, middle-old and old-old. Men and women with low vision/ high visual impairment have been selected from each of the three age groups. In-depth interviews have been carried out with 24 study participants. Data saturation has been attained. The JHPIEGO Gender Analysis Framework underpins the study. The narrative data has been coded in NVivo 10 software. Results: Various symptoms are associated with visual impairment. The young-old with low vision do not report much difficulty due to visual impairment. Study participants with high visual impairment, and in the older age groups do. Difficulty in the discharge of regular chores due to visual impairment is rarely reported. Impaired vision is considered to be inevitable with advancing age. -

India's Health Under Modi: Agenda for the Next Two Years
India’s Health Under Modi: Agenda for the Next Two Years Aparna Pande November 2016 Husain Haqqani Briefing Paper South Asia Program India's Health Under Modi: Agenda for the next Two Years Aparna Pande, Director, India Initiative Husain Haqqani, Director, South and Central Asia South Asia Program © 2016 Hudson Institute, Inc. All rights reserved. For more information about obtaining additional copies of this or other Hudson Institute publications, please visit Hudson’s website, www.hudson.org ABOUT HUDSON INSTITUTE Hudson Institute is a research organization promoting American leadership and global engagement for a secure, free, and prosperous future. Founded in 1961 by strategist Herman Kahn, Hudson Institute challenges conventional thinking and helps manage strategic transitions to the future through interdisciplinary studies in defense, international relations, economics, health care, technology, culture, and law. Hudson seeks to guide public policy makers and global leaders in government and business through a vigorous program of publications, conferences, policy briefings and recommendations. Visit www.hudson.org for more information. Hudson Institute 1201 Pennsylvania Avenue, N.W. Suite 400 Washington, D.C. 20004 P: 202.974.2400 [email protected] www.hudson.org Table of Contents Overview 5 India’s Healthcare Trends 8 India’s Statistical Healthcare Profile 8 India’s Health Compared with Other Nations 13 Modi Government’s Two Year Performance 25 National Health Policy 25 Swaach Bharat (Clean India) 28 Infrastructure and Services 32 The Private Sector 34 Challenges & Opportunities: The Next Two Years 37 Accessibility 37 Affordability and Innovation 40 Challenges and Opportunities 43 India’s Health Under Modi 4 India’s Health Under Modi Overview rime Minister Narendra Modi came to power in May 2014 promising changes in a number of areas, including healthcare. -
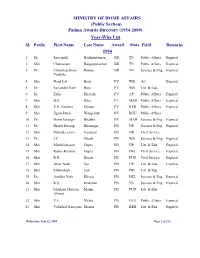
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -

10. Committee Section (H&Fw)
10. COMMITTEE SECTION (H&FW) 10.1 Functions of the Committee - The Committee Section (H&FW) is entrusted with the task of providing secretarial assistance to the Department-related Parliamentary Standing Committee on Health & Family Welfare. Like other Department-related Parliamentary Standing Committees serviced by Rajya Sabha Secretariat, the Committee on Health & Family Welfare is governed by Rules 268 to 277 of the Rules of Procedure and Conduct of Business in the Council of States. Further, Rules 74 to 92 of the said Rules relating to Select Committees on Bills also apply mutatis mutandis to the Committee. The Committee on Health & Family Welfare deals with Ministry of Health & Family Welfare which consists of four Departments namely: - (i) Department of Health & Family Welfare; (ii) Department of AYUSH; (iii) Department of Health Research; and (iv) Department of AIDS Control The functions assigned to the Committee, as enumerated in Rule 270 of the Rules of Procedure and Conduct of Business in the Council of States are (i) consideration of Demands-for- Grants of the Ministry of Health and Family Welfare, (ii) examination of Bills pertaining to the Ministry when referred to the Committee by the Hon’ble Chairman or Speaker, as the case may be, (iii) consideration of Annual Reports of the Ministry, and (iv) consideration of national basic long- term policy documents presented to both the Houses and referred to the Committee by the Hon’ble Chairman or the Speaker, as the case may be, and report thereon. 10.2 Tenure of the Committee: The Committee was reconstituted on the 31st August, 2010 under the chairmanship of Shri Brajesh Pathak, M.P. -

Sustainable Strategies for a Healthy India: Imperatives for Consolidating the Healthcare Management Ecosystem
Sustainable Strategies for a Healthy India: Imperatives for Consolidating the Healthcare Management Ecosystem For private circulation only June 2013 www.deloitte.com/in Contents Health in India 1 Emerging trends and imperatives 3 Collaborate to Innovate 6 Creating and facilitating a collaborative environment 13 References 14 Contacts 16 2 Health in India – Status and successes India rightly brands itself as incredible. in-patient treatment, possibly making The country’s remarkable political, quality healthcare and private sector economic and cultural transformation facilities accessible to the poor. over the past few decades has made it a geopolitical force. Healthcare is However, these exciting opportunities one of the industries that marks this often mask certain urgent predicaments. strengthened global presence. The healthcare sector in India is As per industry reports, healthcare is currently at a cusp. Issues of access, poised to grow at an estimated annual affordability, quality of care and rate of 19 per cent to reach USD efficiency remain significant. A number 280 billion by 20201 with India being of reports have been published about recognized as a destination for world the poor health status of India, class healthcare. During the last decade compared to its Low and Middle the private sector grew to become the Income Country (LMIC) peers. In terms major provider of healthcare services. of vital statistics like infant mortality Its share of beds increased from 49 (IMR) and maternal mortality, India has per cent in 2002 to 63 per cent in lagged behind significantly. Even life 20102. As per NSSO 2008, the private expectancy, at 62 years, is three years sector accounted for 60 percent of all below the LMIC average. -
S.No. Sector Core Group Constituted?
APPENDIX I List of Sectors S.No. Sector Core Group Constituted? 1 Automobile Yes 2 Beauty and Wellness Yes 3 Construction, Construction Material, and Real Estate Yes 4 Electronics & Hardware Yes 5 Fabrication Yes 6 Food Processing & Preservation Yes 7 IT & ITES Yes 8 Power Generation, Transmission, Distribution, Wiring, and Yes Electrical Equipments 9 Production & Manufacturing Yes 10 Textiles and Apparel Yes 11 Travel, Tourism, and Hospitality Yes 12 Organized Retail No 13 Telecommunications No 14 Industrial Automation & Instrumentation No 15 Handicrafts No 16 Mining & Mineral Processing No 17 Plastics No 18 Leather & Leather Goods No 19 Gems And Jewellery No 20 Agriculture, Horticulture, Floriculture No 21 Dairy, Meat, Poultry, Fisheries No 22 Rubber No 23 Health Care No 24 Entertainment, Media, Advertising, Event Management No 25 Banking Financial Service & Insurance (BFSI) No ANNEXURE I List of Sectors S.No. Sector 1 Automobile 2 Beauty and Wellness 3 Construction, Construction Material, and Real Estate 4 Electronics & Hardware 5 Fabrication 6 Food Processing & Preservation 7 IT & ITES 8 Power Generation, Transmission, Distribution, Wiring, and Electrical Equipments 9 Production & Manufacturing 10 Textiles and Apparel 11 Travel, Tourism, and Hospitality ANNEXURE II CORE GROUP FOR AUTOMOBILE SECTOR S.No. Name and Designation Contribution in Core Group 1 Shri T.C. Saravanabava, DDG(AT), DGET Mentor Headquarters 2 Mr. K.S. Rao, JDT, CSTARI, Kolkata Representative of CSTARI 3 Mr. Ravichandran, DDT, NIMI Chennai Representative of NIMI 4 Mr. R.K. Gowda, DDT, ATI Hyderabad Champion Master Trainer 5 Mr. Yuvraj, DDT, ATI Chennai Member 6 Mr. G. Venktesh, ADT, ATI Hyderabad Member 7 Mr. -

King's Research Portal
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by King's Research Portal King’s Research Portal DOI: 10.1016/j.healthplace.2016.08.004 Document Version Peer reviewed version Link to publication record in King's Research Portal Citation for published version (APA): Murray, S. F., Bisht, R., & Pitchforth, E. (2016). Emplacing India's “medicities”. HEALTH AND PLACE, 42, 69-78. https://doi.org/10.1016/j.healthplace.2016.08.004 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Healthcare Tourism in India
C M Y K 3 Healthcare Tourism In India 3.1 HEALTHCARE SCENARIO IN INDIA 3.1.1 Overview India’s health system can be categorized into three distinct phases31: a) In the initial phase of 1947-1983, health policy was assumed to be based on two broad principles: (i) that none should be denied healthcare for want of ability to pay, and (ii) that it was the responsibility of the state to provide healthcare to the people. This phase saw moderate achievements. b) In the second phase of 1983-2000, a National Health Policy was announced for the first time in 1983, which articulated the need to encourage private initiative in healthcare service delivery and encouraged the private sector to invest in healthcare infrastructure through subsidies. The policy also enhanced the access to publicly funded primary healthcare, facilitating expansion of health facilities in rural areas through National Health Programmes (NHPs). c) The third phase, post-2000, is witnessing a further shift and broadening of focus; the current phase addresses key issues such as public-private partnership, liberalization of insurance sector, and the government as a financier. 31 Report of the National Commission on Macroeconomics and Health, Ministry of Health and Family Welfare, Government of India, August 2005 77 C M Y K C M Y K Healthcare Tourism: Opportunities for India The National Health Policy, 200232 outlines improvement in the health status of the population as one of the major thrust areas in social development programme. It focuses on the need for enhanced funding and an organizational restructuring of the national public health initiatives in order to facilitate more equitable access to the health facilities. -

Emplacing India's Medicities MURRAY Firstonline28september2016 GREEN
King’s Research Portal DOI: 10.1016/j.healthplace.2016.08.004 Document Version Peer reviewed version Link to publication record in King's Research Portal Citation for published version (APA): Murray, S. F., Bisht, R., & Pitchforth, E. (2016). Emplacing India's “medicities”. HEALTH AND PLACE, 42, 69-78. https://doi.org/10.1016/j.healthplace.2016.08.004 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Dr. Devi Shetty - Doctor of Science
Dr. Devi Shetty - Doctor of Science Dr. Devi Shetty, Chairman, Narayana Health Group was awarded today with an honorary doctorate degree of Doctor of Science for his contributions and commitment to the field of Medical Science. The Doctorate was conferred upon him with the consent of the President of India Pranab Mukherjee to the proposal made by Indian Institute of Technology Madras (IIT-M). The Honorary Degree was bestowed by Prof. Bhaskar Rammurthi – Director, IIT- M as part of 51st convocation at a ceremony in Chennai. Receiving the award, Dr. Devi Shetty, Chairman, Narayana Health, said, A tribute to a person is always an acknowledgment of his ideologies, efforts and the purpose to which that person has devoted his life. It has been our constant endeavor at Narayana Health to bring down the cost of healthcare and make quality healthcare accessible to all sections of society. Thus, I share this award with all those who have also dedicated themselves for this cause. He also added, Consolidation is the only way to reach out to a larger level, for which it s important to partner with multiple stakeholders, including academia. Dr. Devi Shetty is also the recipient of the prestigious civilian award, Padma Bhushan for his contributions in the field of healthcare, especially heart care After completing his graduate degree in Medicine and post-graduate work in General Surgery from Kasturba Medical College, Mangalore, he trained in cardiac surgery at Guys Hospital in the United Kingdom. He performed the first neonatal heart surgery in the country on a 9-day-old baby. -

International Profiles of Health Care Systems
EDITED BY Elias Mossialos and Ana Djordjevic London School of Economics and Political Science MAY 2017 MAY Robin Osborn and Dana Sarnak The Commonwealth Fund International Profiles of Health Care Systems Australia, Canada, China, Denmark, England, France, Germany, India, Israel, Italy, Japan, the Netherlands, New Zealand, Norway, Singapore, Sweden, Switzerland, Taiwan, and the United States THE COMMONWEALTH FUND is a private foundation that promotes a high performance health care system providing better access, improved quality, and greater efficiency. The Fund’s work focuses particularly on society’s most vulnerable, including low-income people, the uninsured, minority Americans, young children, and elderly adults. The Fund carries out this mandate by supporting independent research on health care issues and making grants to improve health care practice and policy. An international program in health policy is designed to stimulate innovative policies and practices in the United States and other industrialized countries. MAY 2017 International Profiles of Health Care Systems Australia EDITED BY Canada Elias Mossialos and Ana Djordjevic London School of Economics and Political Science China Denmark Robin Osborn and Dana Sarnak The Commonwealth Fund England France To learn more about new publications when they become available, Germany visit the Fund’s website and register to receive email alerts. India Israel Italy Japan The Netherlands New Zealand Norway Singapore Sweden Switzerland Taiwan United States CONTENTS Table 1. Health Care System Financing and Coverage in 19 Countries . 6 Table 2. Selected Health Care System Indicators for 18 Countries . 7 Table 3. Selected Health System Performance Indicators for 17 Countries. 8 Table 4. Provider Organization and Payment in 19 Countries . -

Bangalore Faculty of Art and Design
List of Alumni of M. S. Ramaiah University of Applied Sciences (SAMPARK), Bangalore Faculty of Art and Design Sl. Programme Year of Name Contact Address Photograph e-mail id No. Completed Admission Mobile no. 650 M. Des. (Product 2015 E SUMANTH H NO.43/233, N R 7075990455 Design) PET, KURNOOL, SUMANTHZ ANDHRA PRADESH- @LIVE.IN 518004 649 M. Des. (Product 2015 JAYANT G 27,"SHREE 8147999872 Design) ANKOLEKAR SHARVARI, C- jayantga@y BLOCK, APOORVA ahoo.in NAGAR, GOKUL ROAD, HUBLI- 580030 648 M. Des. (Product 2015 PRANATI AMITHORE 9609951821 Design) MAHANTY VILLAGE, 09199312p SUKHADALLI POST, [email protected] ANKURA DISTRICT, m WEST BENGAL- 722150 647 M. Des. (Product 2015 SACHIN 6586, GUBBI 9036075886 Design) JAYAPRAKASH HUCHAPPA sachinjayapr LAYOUT, SUBHASH akash26@g NAGAR, mail.com NELAMANGALA- 562123 646 M. Des. (Product 2015 SHASHANK U K 5, 5TH CROSS, 80FT 8951273001 Design) ROAD, shashankuk MAHALAKSHMI [email protected] NAGAR, BATWADI, om TUMKUR-572103 645 M. Des. (Product 2015 ROSHITH K P RESHMALAUYAM 9596164633 Design) (H),VATAKARA, designs.spe KOZHIKODE, [email protected] KERALA-673104 om 644 M. Des. (Product 2015 GOVARTHANAM 23, OLD BAZER 9566752210 Design) V STREET, TIRUTANI, govaa082@ TIRUVALLUR gmail.com DISTRICT, TAMIL NADU-631209 List of Alumni of M. S. Ramaiah University of Applied Sciences (SAMPARK), Bangalore Faculty of Art and Design Sl. No. Programme Year of Name Contact Address Photograph e-mail id/Mobile no. Completed Admission 643 M.Des CAGD 2014 Arjun Nedungadi SWAPNAM HOUSE, NO-94, OPP. 9633940649 KENDRIYA VIDYALAYA, KADAVANTHRA. KOCHI-682020