Division of Community and Population Health Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

New York Society for Gastrointestinal Endoscopy the Spring Course
New York Society for Gastrointestinal Endoscopy The Spring Course: Best of DDW 2021 Saturday, June 5, 2021 8:00 am – 3:15 pm Virtual Event The Spring Course: Best of DDW 2021 is jointly provided by the Albert Einstein College of Medicine – Montefiore Medical Center and the New York Society for Gastrointestinal Endoscopy Page 1 of 10 Course Description The Spring Course is devoted to a review of the most compelling topics discussed during Digestive Disease Week® 2021. Faculty will present critically important information on new drugs, the etiology and pathophysiology of disease states, the epidemiology of diseases, the medical, surgical and endoscopic treatment of disease, and the social impact of disease states pertaining to gastroenterology, endoscopy, and liver disease. The program includes a video forum of new endoscopic techniques as well as a summary of the major topics presented at the most important academic forum in gastroenterology, making for an invaluable educational experience for those who were unable to attend Digestive Disease Week® and an excellent summary review for all others. Learning Objectives • Discuss the spectrum of gastrointestinal diseases such as motility disorders and colorectal cancer and outline the enhancement and effectiveness of related treatment options such as the use of artificial intelligence in the detection and resection of polyps during colonoscopy • Evaluate advances in the methods of assessing disease status in patients with inflammatory bowel disease and discuss the application of these techniques -
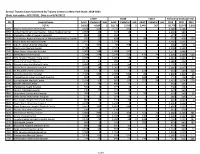
Annual Trauma Cases Submitted by Trauma Centers in New York State
Annual Trauma Cases Submitted by Trauma Centers in New York State: 2018-2021 (Date last update: 8/17/2021, Data as of 8/3/2021) Y2019 Y2020 Y2021 TOTALS by Discharge Year PFI Hospital Name Adult Pediatric Unk Adult Pediatric Unk Adult Pediatric Unk 2019 2020 2021 TOTAL 54,562 4,209 1 50,176 3,793 3 5,443 367 - 58,772 53,972 5,810 0001 Albany Medical Center Hospital 3,168 320 . 3,772 392 . 3,488 4,164 - 0058 United Health Services Hospital - Wilson Medical Center 1,067 23 . 934 13 . 1,090 947 - 0135 Champlain Valley Physicians Hospital 465 12 . 314 2 . 477 316 - 0180 Mid Hudson Regional Hospital of Westchester Medical Center 745 22 . 428 . 98 2 767 428 100 0181 Vassar Brothers Medical Center 1,141 15 . 1,029 2 . 1,156 1,031 - 0208 John R. Oishei Children's Hospital 64 335 . 68 258 2 4 399 326 6 0210 Erie County Medical Center 2,598 1 . 2,525 . 2,599 2,525 - 0245 Stony Brook University Hospital 2,003 168 . 1,686 162 . 2,171 1,848 - 0413 Strong Memorial Hospital 2,244 254 . 2,246 223 470 74 2,498 2,469 544 0511 NYU Langone Hospital-Long Island 1,288 77 . 1,305 56 26 8 1,365 1,361 34 0527 Mount Sinai South Nassau 1,171 17 . 989 4 . 1,188 993 - 0528 Nassau University Medical Center 1,384 34 . 1,187 25 . 1,418 1,212 - 0541 North Shore University Hospital 2,150 16 . 1,907 10 . -

1 a Letter from Hospital Providers
A Letter from Hospital Providers Regarding COVID-19 and Homelessness in New York City April 15, 2020 Dear Mayor Bill de Blasio, Governor Andrew Cuomo, NYC Department of Social Services Commissioner Steven Banks, New York City Emergency Management Commissioner Deanne Criswell, City Council Speaker Corey Johnson, and City Council Member Stephen Levin: We are frontline workers—physicians, nurses, social workers, and others—from hospitals across New York City writing to express our concerns and recommendations specific to the thousands of New Yorkers who are homeless during the COVID-19 pandemic. These individuals cannot stay home, because they have no home. They are at high risk for contracting and dying from COVID-19. Homeless New Yorkers are our patients and our neighbors. We commend you for steps you have taken to protect them and to preserve the capacity of our hospitals, such as creating isolation sites for people experiencing homelessness who have symptoms of COVID-19 and developing protocols to keep people with only mild symptoms out of emergency departments. Many of us have expressed our concerns publicly and privately, and are appreciative that several of these concerns have been addressed. We remain troubled, however, at the slow and still inadequate response to protect homeless New Yorkers. As of April 12, there were already 421 homeless New Yorkers known to be infected with COVID-19 and 23 had died from the disease. Black and Latinx New Yorkers are disproportionately affected by homelessness and incarceration (itself associated with both homelessness and risk of exposure to coronavirus), layering health inequity upon health inequity. -

Name Graduation Year Current Status/Employment Lindsey Reese, MD
Name Graduation Year Current Status/Employment Lindsey Reese, MD 2011 Associate Vice Chair of Clinical Affairs, Assistant Professor, Indiana University School of Medicine, Indiana, IN Keith Sigel, MD 2011 Associate Professor, Department of Medicine, Icahn School of Medicine at Mount Sinai, New York, NY Meenakshi Rana, MD 2011 Assistant Professor, Department of Medicine, Icahn School of Medicine at Mount Sinai, New York, NY Nicole Bouvier, MD 2011 Associate Professor, Department of Medicine, Department of Microbiology, Icahn School of Medicine at Mount Sinai, New York, NY Alison Brodginski, DO 2011 Physician, Infectious Diseases Geisinger, Danville, PA Rupa Patel, MD 2011 Assistant Professor, Department of Medicine, Director, Global Health Scholars in Medicine Program, Washington University, St Louis, MO Luciano Kapelusznik, MD 2011 Infectious Disease Physician, Main Line Health, Bryn Mawr, PA Rachel Chasan, MD 2012 Assistant Professor, Department of Medicine, Icahn School of Medicine at Mount Sinai, New York, NY David Banach, MD/MPH/MS 2012 Assistant Professor, Department of Medicine, Head of Infection Prevention, Hospital, Epidemiologist, University of Connecticut, Farmington, CT Melissa Gitman, MD/MPH 2012 Director, Clinical Microbiology Icahn School of Medicine at Mount Sinai, New York, NY Talia Swartz, MD/PhD 2013 Assistant Professor, Department of Medicine, Associate Director of the MD PhD Program, Icahn School of Medicine at Mount Sinai, New York, NY Catherine Smith, MD 2013 Physician, Infectious Diseases St. Vincent’s Healthcare, -

On Restructuring the Nyc Health+Hospitals Corporation
ON RESTRUCTURING THE NYC HEALTH+HOSPITALS CORPORATION PRESERVING AND EXPANDING ACCESS TO CARE FOR ALL NEW YORKERS A report by Barbara Caress and James Parrott to the New York State Nurses Association (NYSNA) October 2017 TABLE OF CONTENTS Executive Summary ..................................................................................................................... p. 1 Recommendations ...........................................................................................................................................p. 3 Key Findings .......................................................................................................................................................p. 5 Background ..................................................................................................................................... p. 9 New York’s health system .............................................................................................................................p. 9 A health system evolving—private system growth—public system losses ...............................p. 10 NYCHH-Public Hospitals ............................................................................................................ p. 14 A little history .....................................................................................................................................................p. 14 Taking care of the community ....................................................................................................................p. -

Montefiore Liver Disease and Transplantation Program Staff
Montefiore Liver Disease and Transplantation Program Staff Milan Kinkhabwala, MD Paul J. Gaglio, MD Chief, Division of Transplantation Medical Director Professor of Surgery Adult Liver Transplantation Albert Einstein College of Medicine Professor of Clinical Medicine Specialty Interests: liver transplantation, Albert Einstein College of Medicine hepatobiliary surgery Specialty Interests: viral hepatitis following Medical Degree: Cornell University liver transplantation, novel treatments of Medical College, New York, NY hepatitis B and C, NASH, acute liver failure Residency: Cornell Medical Center, Medical Degree: University of Medicine New York, NY & Dentistry of New Jersey, Newark, NJ Fellowship: University of California at Residency: Mount Sinai Medical Center, Los Angeles Medical Center New York, NY Fellowship: University of Medicine & Sarah Bellemare, MD Dentistry of New Jersey, Newark, NJ Assistant Professor of Surgery Albert Einstein College of Medicine Dominique Jan, MD Chief, Division of Pediatric Surgery Specialty Interests: liver transplantation, hepatobiliary surgery Director, Pediatric Transplantation Medical Degree: Faculté de Médecine, The Children’s Hospital at Montefiore Université Laval, Québec, Canada Professor of Surgery Residency: Université de Montréal, Albert Einstein College of Medicine Montréal, Québec, Canada Fellowship: Columbia-Presbyterian Medical Specialty Interests: pediatric liver Center, New York, NY transplantation, hepatobiliary surgery, intestinal failure Medical Degree: Université Pierre et Marie Javier -

The World Trade Center Environmental Health
The World Trade Center Environmental Health Center at Bellevue Hospital of the New York City Health and Hospitals Corporation (HHC) is a program to treat people with WTC-related illness. The Center, which works in partnership with community organizations and people affected by 9/11, has added two other sites: Gouverneur Healthcare Services in Lower Manhattan and Elmhurst Hospital in Queens. Bellevue Hospital Center 462 First Avenue New York, New York 10016 Gouverneur Healthcare Services 227 Madison Street New York, New York 10002 Elmhurst Hospital Center 79-01 Broadway Elmhurst, New York 11373 For information about WTC health services, or to make an appointment for treatment, call toll free 1-877-WTC-0107 (1-877-982-0107). The WTC Environmental Health Center at Bellevue, and now at Gouverneur Health Services and Elmhurst Hospital, offers treatment to people who have health problems as a result of 9/11. You can get treatment even if you can’t pay or have no insurance. You can come for treatment if, on or after 9/11, you: • Were a resident who lived in Lower Manhattan • Were a student in a school in the area • Worked in or around area offices, stores, schools, or apartment buildings • Helped in the clean-up of buildings in the affected area How would I know if my health problems are related to 9/11? It is hard to know if your health problems are due to 9/11. Some problems might include: • Shortness of breath • Stomach problems • Skin problems • Depression, anxiety, nervousness If you think you have a health problem related to 9/11, call toll free 1-877-WTC-0107. -

The New York City Health and Hospitals Corporation: TRANSFORMING a Public Safety Net Delivery System to ACHIEVE Higher PERFORMANCE
THE COMMONWEALTH FUND COMMISSION ON A HIGH PERFORMANCE HEALTH SYSTEM THE NEW YORK CITY HEALTH AND HOSPITALS CORPORATION: TRANSFORMING A PUBLIC SAFETY NET DELIVERY SYSTEM TO ACHIEVE HIGHER PERFORMANCE Douglas McCarthy and Kimberly Mueller Issues Research, Inc. October 2008 ABSTRACT: The New York City Health and Hospitals Corporation (HHC) is a mission-driven, $5.4 billion, public benefit corporation serving 1.3 million New York City residents—the largest municipal hospital and health care system in the United States. In response to external pressures, HHC has undertaken a series of improvement initiatives that appear to be transforming its organizational culture, systems, and care processes. This case study describes how HHC is achieving higher levels of performance through a common clinical information system that promotes information continuity across care settings, care coordination to improve chronic disease management, teamwork and continuous innovation to improve the quality and value of care, and access to appropriate care that is responsive to patients’ needs. Factors that the organization’s leaders identify as critical to successful change include strategic use of information technology, leadership to promote collaborative learning and staff initiative, spread of best practices, alignment of financial incentives, and transparency of results. Support for this research was provided by The Commonwealth Fund. The views presented here are those of the authors and not necessarily those of The Commonwealth Fund or its directors, officers, or staff, or of The Commonwealth Fund Commission on a High Performance Health System or its members. This and other Fund publications are available online at www.commonwealthfund.org. To learn more about new publications when they become available, visit the Fund’s Web site and register to receive e-mail alerts. -

An Organization That Is Delegated for Credentialing
Organizations Delegated for Credentialing Delegate Name • AdvantageCare Physicians • New York - Presbyterian Queens • Albany Medical Center • New York Eye and Ear Infirmary of Mount Sinai • Allied Pediatrics • Northwell Health • American Specialty Health (ASH) • NYC Health + Hospitals - Bellevue Hospital Center • Atlas IPA/Essen Medical Associates • NYC Health + Hospitals - Coney Island Hospital Center • Balance ACO/Corinthian IPA • NYC Health + Hospitals - Elmhurst Hospital Center • Bassett Healthcare Network • NYC Health + Hospitals - Gouverneur Health Services • Beacon Health Options • NYC Health + Hospitals - Harlem Hospital Center • BronxCare Health Systems • NYC Health + Hospitals - Kings County Hospital Center (Bronx Lebanon Hospital Center) • NYC Health + Hospitals - Lincoln Medical and Mental • Brookdale Hospital Medical Center Health Center • Brooklyn Hospital Center • NYC Health + Hospitals - Metropolitan Hospital Center • Care Management Organization (CMO Montefiore) • NYC Health + Hospitals - North Bronx Healthcare • Cayuga Medical Center Network • Charles B. Wang Community Health Center • NYC Health + Hospitals - Queens Hospital Center • Coalition of Asian-American IPA (CAIPA) • NYC Health + Hospitals -Woodhull Medical and Mental • Columbia Affiliated Physicians (CAP) Health Center • ColumbiaDoctors • NYU Langone Health • Community Health Care Network • OptumHealth - Managed Transplant Program • Cornell Medical Center IPA • Palladian Health • Crystal Run Healthcare • PHCS/Multiplan • DentaQuest • ProHEALTH Physicians • eviCore -
Finding Your Way Around Bellevue Hospital Center
Finding your way around DEPARTMENTS Departments are identified by Clinical Research Center 8 Hearing & Speech Clinic 3B Network Support Services 14 Patient Investigations 9 Radiography (X-ray) School 5 Bellevue Hospital Center their internal addresses. Each Bellevue Hospital Center department address is represented Coffee Shop G Hematology Clinic M Neuro Oncology Clinic M Patient Library 6 Radiology (General) 1E by a building symbol and room Colonoscopy 4D HIV Services Administrative Neuro Surgery Clinic 1D Payroll Department 4 Radiology Services 3 VISITING HOURS Offices 12 number ( 000). Community Outreach Neurology Clinic 1D Pediatric Department 8 Receiving B & Wellness 7 Hospital Police G MEDICAL / SURGICAL 20 West & 20 South Neurology Department 7 Pediatric NICU 8 Recovery Program 2 Accounts Payable 4 Community Advisory Board M Hospital Police Administration G 7 East & 7 North 20 North New Patient Services G Pediatric Radiology 3 Recovery Room 1 15 East, 15 West & 15 North Activity Therapy Services 6 Conference Center 8 Hospital Staff Dining Room 12 21 North Newborn Nursery 7 Pediatrics Clinic 3D Rectal Clinic 1D 16 East, 16 West & 16 North Activity Therapy (Psychiatry) 21 Coumadin Clinic 2D Hospitalist Program 16 2:00pm–4:00pm & 7:00pm–8:00pm NICU 8 Pediatrics Eye Clinic 3A Referral Office G 17 East, 17 West & 17 North ACTU (AIDS Clinical Trial Unit) 5 CSS Supportive Case HRA-Medicaid Office G Monday-Sunday Non-Invasive Cardiology 3 Pediatrics Dental Clinic 3E Rehab Clinic 6 11:00am–8:00pm Monday-Sunday Admission Services G Management -

Adult Primary Care Center Ambulatory Care Building, Floor 2
Adult Primary Care Center Ambulatory Care Building, Floor 2 To make an appointment, call (212) 562-5555 If you have any questions, call: ☐ Firm A ☐ Firm B ☐ Firm C ☐ Firm D (212) 562-1703 (212) 562-1703 (212) 562-1686 (212) 562-1686 My Service Coordinator’s name is _____________________________________ My Doctor’s name is ________________________________________________ My Nurse’s name is _________________________________________________ Please arrive to the clinic 30 minutes before your appointment to register. If you are late for your appointment you risk not being seen or being seen later in the day, if an appointment becomes available. To reschedule or cancel your appointment, please call (212) 562-5555. On the day of your appointment, please bring: ☐ Your clinic card (red card) If you are a new patient or you do not have a clinic card, you must register at the Bellevue Business Office at least one hour before your appointment. The Business Office is located on the Ground Floor of the Ambulatory Care Building. Hours are Monday - Thursday 7:30 am - 6:00 pm, and Friday 7:30 am - 5:00 pm. For information, call (212) 562-6264. ☐ Your insurance card (if you have one) ☐ All of the medicines that you take Clinic patients can be seen in the Walk-In Clinic for urgent issues • Hours are 8:00 am - 4:00 pm, Monday - Friday. • The clinic is located on the 2nd floor of the Ambulatory Care Building, Desk 2A. • Please inform the desk staff if you have CHEST PAIN or have a FEVER, RASH or COUGH. While we strive to see every patient at their convenience, if you do not have an urgent need as determined by one of our nurses, you may be scheduled for an appointment at a later date. -

Locations & Contacts
Locations & Contacts As of May 1, 2020 TELEPHONE / FAX SITE MAILING ADDRESS NUMBER Bellevue Hospital Center 462 First Avenue, Rm MN-6A 212-562-7992 New York, NY 10016 FAX: (212)562-8585 [email protected] Coney Island Hospital 2601-Ocean Parkway 718-616-4197 Brooklyn, NY 11235 FAX: (718)616-4574/ Main Building Room 9E12 (718)616-5061 Brooklyn, NY 11235 [email protected] Elmhurst Hospital Center 79-01 Broadway, Rm BE-7 718-334-3144 Elmhurst, NY 11373 FAX: (718)334-2659 [email protected] Harlem Hospital Center 506 Lenox Avenue, 212-939-2777 Women's Pavillion, Rm 136 FAX:(212)939-3546 New York, NY 10037 [email protected] Jacobi Medical Center 1400 Pelham Parkway South, 718-918-4720 Building 1 Room 131 FAX: (718)918-4869 Bronx, NY 10461 [email protected] Kings County Hospital 451 Clarkson Avenue, 718-245-4206 Center Rm. BG 92 FAX:(718)245-4778/ Brooklyn N.Y. 11203 (718)245-1981 [email protected] Lincoln Medical & Mental 234 149th Street, Rm. B77 718-579-5422 Health Center Bronx, NY 10451 FAX:(718)579-4768 [email protected] Metropolitan Hospital 1901 First Avenue, 212-423-7737 Center Rm. 12B1 FAX: (212)423-8648 New York, NY 10029 [email protected] Locations & Contacts North Central Bronx 1400 Pelham Parkway South, 917-577-8398 Hospital Center Building 1 Room 131 FAX: (718)515-1489 Bronx, NY 10461 [email protected] Queens Hospital Center 82-68 164th St, Room N100 718-883-2436 Jamaica, NY 11432 FAX: (718)883-6118 [email protected] Woodhull Mental and 760 Broadway, 718-963-8023 or 8160 Medical Center Room 1Ab