Assessing the Impact of Human Mobility to Predict Regional Excess
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fight, Flight Or Lockdown Edited
Fight, Flight or Lockdown: Dorn & Satterly 1 Fight, Flight or Lockdown - Teaching Students and Staff to Attack Active Shooters could Result in Decreased Casualties or Needless Deaths By Michael S. Dorn and Stephen Satterly, Jr., Safe Havens International. Since the Virginia Tech shooting in 2007, there has been considerable interest in an alternative approach to the traditional lockdown for campus shooting situations. These efforts have focused on incidents defined by the United States Department of Education and the United States Secret Service as targeted acts of violence which are also commonly referred to as active shooter situations. This interest has been driven by a variety of factors including: • Incidents where victims were trapped by an active shooter • A lack of lockable doors for many classrooms in institutions of higher learning. • The successful use of distraction techniques by law enforcement and military tactical personnel. • A desire to see if improvements can be made on established approaches. • Learning spaces in many campus buildings that do not offer suitable lockable areas for the number of students and staff normally in the area. We think that the discussion of this topic and these challenges is generally a healthy one. New approaches that involve students and staff being trained to attack active shooters have been developed and have been taught in grades ranging from kindergarten to post secondary level. There are however, concerns about these approaches that have not, thus far, been satisfactorily addressed resulting in a hot debate about these concepts. We feel that caution and further development of these concepts is prudent. Developing trend in active shooter response training The relatively new trend in the area of planning and training for active shooter response for K-20 schools has been implemented in schools. -

The Impact of COVID-19 Lockdown Restrictions on Dogs & Dog Owners in the UK
The impact of COVID-19 lockdown restrictions on dogs & dog owners in the UK 26th August 2020 Table of contents Executive summary 1 Introduction 2 Dog demographics 4 Gastrointestinal health 4 Dog owners 5 Owners’ bond with their dogs 5 Owners’ feelings about their dog during lockdown 6 Contingency planning 8 Management of dogs 9 Routine changes 9 Exercise 9 Walk location 9 On/off lead walking 9 Frequency of walking 9 Duration of walking 9 Meeting other dogs 9 House rules 9 Time left alone 10 Dog behaviour 12 Behaviour towards adults 12 Behaviour towards children 13 General observations 14 Reactivity 14 Attention seeking behaviour 14 Behaviour on walks 14 Separation-related behaviour 14 Behaviour when about to be left 14 Behaviour when left 14 Enrichment, games and training 16 Toys 17 Puppies: socialisation/habituation 18 Conclusions 19 Future work 20 Appendix 21 Dogs Trust 1 Executive summary Lifestyle changes ensued for many people across the United Kingdom Dog behaviour (UK) in the Spring of 2020 due to ‘lockdown’ restrictions imposed to • Dogs’ behaviour towards household members was reported curb the spread of a newly emerged virus, SARS-CoV-2, which caused by owners to have changed considerably during lockdown, a global pandemic of the disease known as COVID-19. with large increases seen in the proportion of dogs reported to display attention-seeking and ‘clingy’ behaviours. Compared with More than 6,000 dog owners living in the UK completed our online February, there was an 82% increase in the proportion of owners survey between the 4th – 12th May 2020 (the most restrictive phase of who reported that their dog whined or barked when someone the lockdown measures). -
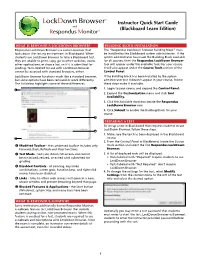
Instructor Quick Start Guide Lockdown Browser™ and Respondus Monitor
™ LockDown Browser Instructor Quick Start Guide and (Blackboard Learn Edition) Respondus Monitor™ WHAT IS RESPONDUS LOCKDOWN BROWSER? BUILDING BLOCK INSTALLATION Respondus LockDown Browser is a custom browser that The “Respondus LockDown Browser Building Block” must locks down the testing environment in Blackboard. When be installed by the Blackboard system administrator. If the students use LockDown Browser to take a Blackboard test, system administrator has made the Building Block available they are unable to print, copy, go to other websites, access for all courses, then the Respondus LockDown Browser other applications, or close a test until it is submitted for tool will appear under the available tools for your course. grading. Tests created for use with LockDown Browser It will also appear under the Course Tools section of the cannot be accessed with standard browsers, either. Control Panel. LockDown Browser functions much like a standard browser, If the Building Block has been installed by the system but some options have been removed or work differently. administrator but it doesn’t appear in your course, follow The list below highlights some of these differences. these steps make it available. 1. Login to your course and expand the Control Panel. 2. Expand the Customization menu and click Tool Availability. 3. Click the Available checkbox beside the Respondus LockDown Browser row. 4. Click Submit to enable the Building Block for your course. PREPARING A TEST To set up a test in Blackboard that requires students to use LockDown Browser, follow these steps: 1. Make sure the test has been deployed in the Blackboard course. -

Pro Wrestling Over -Sell
TTHHEE PPRROO WWRREESSTTLLIINNGG OOVVEERR--SSEELLLL™ a newsletter for those who want more Issue #1 Monthly Pro Wrestling Editorials & Analysis April 2011 For the 27th time... An in-depth look at WrestleMania XXVII Monthly Top of the card Underscore It's that time of year when we anything is responsible for getting Eddie Edwards captures ROH World begin to talk about the forthcoming WrestleMania past one million buys, WrestleMania, an event that is never it's going to be a combination of Tile in a shocker─ the story that makes the short of talking points. We speculate things. Maybe it'll be the appearances title change significant where it will rank on a long, storied list of stars from the Attitude Era of of highs and lows. We wonder what will wrestling mixed in with the newly Shocking, unexpected surprises seem happen on the show itself and gossip established stars that generate the to come few and far between, especially in the about our own ideas and theories. The need to see the pay-per-view. Perhaps year 2011. One of those moments happened on road to WreslteMania 27 has been a that selling point is the man that lit March 19 in the Manhattan Center of New York bumpy one filled with both anticipation the WrestleMania fire, The Rock. City. Eddie Edwards became the fifteenth Ring and discontent, elements that make the ─ So what match should go on of Honor World Champion after defeating April 3 spectacular in Atlanta one of the last? Oddly enough, that's a question Roderick Strong in what was described as an more newsworthy stories of the year. -

1 PROCEEDINGS of a SPECIAL COURT-MARTIAL 2 The
1 PROCEEDINGS OF A SPECIAL COURT-MARTIAL 2 The military judge called the Article 39(a) session to 3 order. The court met at Holloman Air Force Base, New Mexico, at 4 0857 hours on 6 November 2012 pursuant to the following 5 order(s): 6 7 8 9 10 [The convening order, Special Order A-60, Headquarters 12 1 Art- 11 Force,(ACC), dated 27 August 2012, Davis Monthan AFB, Arizona, 12 as amended by the convening order, Special 13 Order A-6, same Headquarters, dated 1 November 2012, as amended 14 by the convening order, Special Order A-7, same Headquarters, 15 dated 5 November 2012. They 16 are attached to this record of trial as pages 1.1 through 1.3. 17 18 19 The 20 USAF Trial Judiciary Memorandum, dated 7 Sep 2012, 21 detailing the military judge, is attached to this record as page 22 1.4]. 1 ARTICLE 39(a) SESSION 2 [The Article 39(a) session was called to order at 0857 3 hours on 6 November 2012. It was attended by the military 4 judge, both trial counsel, both defense counsel, the accused and 5 the reporter]. 6 NJ: This Article 39(a) session is called to order. 7 ATC: This court-martial is convened by Special Order A-60, 8 Headquarters 12t-' Air Force, Davis Monthan Air Force Base, g Arizona, dated 27 August 2012, as amended by Special order A-6, 10 same Headquarters, dated 1 November 2012, as amended by Special 11 Order A-7, same Headquarters, dated 5 November 2012, copies of 12 which have been furnished to the military judge, counsel, the 13 accused and which will be inserted at this point in the record. -

Annual Compilation of Wrestling Research
2020 Annual Compilation of Wrestling Research David Curby, EdD [email protected] The Annual Compilation of Wrestling Research 2020 is compilation of published wrestling- related research published during 2020 and is provided by the International Network of Wrestling Researchers (INWR). The INWR is the largest scientific support group for a sport in the world! Our group has grown to over 500 academics, scientists, doctors and wrestling professionals, from 82 countries who are involved with the sport of wrestling. (www.inwr-wrestling.com) Our Mission Statement is: The International Network of Wrestling Researchers (INWR) seeks to facilitate the development of wrestling around the world by drawing all wrestling sport science professionals together, in a manner that through our international and intercultural cooperation we are empowered to support the development of wrestling with our research and educational programs. We have organized scientific meetings at the senior world wrestling championships and we were instrumental in working with United World Wrestling (UWW) in establishing the Scientific Commission. The INWR sponsors the Rayko Petrov Award memorializing the great Bulgarian wrestler, coach and prolific scholar. Each year the INWR names the person to be honored and that person delivers the memorial lecture at the INWR Annual Meeting. They are presented with the spectacular bronze trophy by Christo Christov commissioned by the Bulgarian Wrestling Federation. The Young Researcher Award is also presented to a researcher less than thirty years of age. We publish the International Journal of Wrestling Science which is the only journal dedicated to the study of the world’s oldest sport. The International Journal of Wrestling Science is a peer reviewed journal for professionals working in wrestling and wrestling sport science. -

Weyanoke Wildlife Sanctuary Pathways Spring 2020
Weyanoke Wildlife Sanctuary Pathways Spring 2020 Coronavirus and the Weyanoke Sanctuary Hello Neighbors and Friends, First off we hope that everyone is well and maintaining responsible anti virus precautions. Because of the pandemic we thought it especially important that the Sanctuary stays open and available for people to go to as a place of safety and relax- ation where folks can go in these times of stress. We have had lots of people take ad- vantage of this; families, young kids, older folks, all enjoying the fresh outdoors. We are very thankful for the way that trash is mostly picked up and the Sanctuary is mostly respected. Unfortunately there have been some people that ignore the rules, and bring their dogs and bikes in the Sanctuary and then get angry when someone points out the rules. We have also had two break-ins at our shed on the property, locks cut and chains stolen, a Tazz wood chipper, that used to be green with a bent left rear axel in case anyone has seen it, was stolen, in addition to packs of work gloves and face masks used by our volunteers. As a result of the break-ins and thefts we will now lock the Sanctuary up every night. We will install surveillance and security equipment at great expense. We also need to give the Sanctuary a rest from all the human contact that has been going on, with so many people using the space. This is, after all, a bird and wildlife sanctuary, not a people sanctuary, and it needs time to recuperate. -

Book Review of Caught: the Prison State and the Lockdown of American Politics, by Marie Gottschalk
445 Book Review Marie Gottschalk, Caught: The Prison State and the Lockdown of American Politics, Princeton, NJ: Princeton University Press, 2015, pp. 474, $35.00 Cloth; $24.95 Paper. Reviewed by Shon Hopwood Introduction The American criminal justice system is a mess. It criminalizes too much conduct, disproportionately targets the poor and people of color, and overly relies on incarceration. It has become so immense that millions of Americans are starting to feel its squeeze as its grip fails every demographic of America from crime victims and taxpayers to those it convicts. The system desperately needs to be reexamined before an even larger segment of Americans comes to view the rule of criminal law as a rule of oppression. To their credit, academics can lay claim to being among the first to highlight the carceral state and its causes. A deep body of literature now exists on the mass incarceration crisis,1 and Professor Marie Gottschalk has made an important contribution with her book Caught. Whereas others focused on discrete parts of the carceral state, Gottschalk has meticulously detailed all of it—from the political factors that created the American carceral state to those who have profited from it. No stone is unturned in her quest to comprehensively strip our criminal justice problems bare, and she consistently reminds us of their enormity. Her thesis: The carceral state has grown so massive that it has cut off millions from the American Dream, which Gottschalk defines as “the faith that everyone has an inalienable right to freedom, justice, and equal opportunities to get ahead, and that everyone stands equal before the law” (2). -

SHOULD SCHOOLS BE CONDUCTING LOCKDOWN DRILLS? by Jaclyn Schildkraut, Kathryn Grogan, & Amanda Nabors June 2020
SHOULD SCHOOLS BE CONDUCTING LOCKDOWN DRILLS? by Jaclyn Schildkraut, Kathryn Grogan, & Amanda Nabors June 2020 Mass shootings in schools, includ- available research and best practices, such experiences are traumatizing. ing the 2012 attack at Sandy Hook to provide better context to answer The other main argument raised by Elementary School in Newtown, such a question. advocates is that by teaching students Connecticut, and the 2018 attack how to respond to active shooters, at Marjory Stoneman Douglas High Concerns Over Drills schools are also training potential School in Parkland, Florida, prompt assailants because a considerable calls for improved safety and security Much of the concern over lockdowns proportion of school-shooting perpe- practices to help prevent future attacks follows news reports of school drills trators are themselves students (Wilkie, or, in the event that one occurs, including activities that have raised 2019). Such an argument, however, minimize the loss of life. Following issues concerning the safety and fails to acknowledge the efficacy of a the 1999 shooting at Columbine psychological well-being of students, locked door — the number-one life- High School in Littleton, Colorado, faculty, and staff. For example, Indiana saver in school shootings, and a major lockdown drills were introduced as teachers were shot with plastic pellets focus of lockdown drills (Martaindale a response strategy for educational during one training exercise (Zraick, et al., 2017; Sandy Hook Advisory institutions faced with a similar situa- 2019). High school students in Ohio Commission, 2015). Locked doors tion. Today, 95 percent of U.S. schools were exposed to sounds of simulated can be highly effective in stopping perform lockdown drills as part of their gunfire (Richter, 2019). -

Impact of the Coronavirus Pandemic Lockdown on Atmospheric Nanoparticle Concentrations in Two Sites of Southern Italy
atmosphere Article Impact of the Coronavirus Pandemic Lockdown on Atmospheric Nanoparticle Concentrations in Two Sites of Southern Italy Adelaide Dinoi 1,* , Daniel Gulli 2 , Ivano Ammoscato 2, Claudia R. Calidonna 2 and Daniele Contini 1 1 Institute of Atmospheric Sciences and Climate, ISAC-CNR, S. P. Lecce-Monteroni km 1.2, 73100 Lecce, Italy; [email protected] 2 Institute of Atmospheric Sciences and Climate, ISAC-CNR, Zona Industriale, Comparto 15, 88046 Lamezia Terme, Italy; [email protected] (D.G.); [email protected] (I.A.); [email protected] (C.R.C.) * Correspondence: [email protected] Abstract: During the new coronavirus infection outbreak, the application of strict containment mea- sures entailed a decrease in most human activities, with the consequent reduction of anthropogenic emissions into the atmosphere. In this study, the impact of lockdown on atmospheric particle number concentrations and size distributions is investigated in two different sites of Southern Italy: Lecce and Lamezia Terme, regional stations of the GAW/ACTRIS networks. The effects of restrictions are quantified by comparing submicron particle concentrations, in the size range from 10 nm to 800 nm, measured during the lockdown period and in the same period of previous years, from 2015 to 2019, considering three time intervals: prelockdown, lockdown and postlockdown. Different percentage reductions in total particle number concentrations are observed, −19% and −23% in Lecce and −7% Citation: Dinoi, A.; Gulli, D.; and −4% in Lamezia Terme during lockdown and postlockdown, respectively, with several variations Ammoscato, I.; Calidonna, C.R.; in each subclass of particles. -
Epidemiological and Economic Effects of Lockdown
BPEA Conference Drafts, September 24, 2020 Epidemiological and Economic Effects of Lockdown Alexander Arnon, Penn Wharton Budget Model John Ricco, Penn Wharton Budget Model Kent Smetters, Penn Wharton Budget Model DO NOT DISTRIUTE – ALL PAPERS ARE EMBARGOED UNTIL 9:00PM ET 9/23/2020 Conflict of Interest Disclosure: The authors did not receive financial support from any firm or person for this paper or from any firm or person with a financial or political interest in this paper. They are currently not an officer, director, or board member of any organization with an interest in this paper. PRELIMINARY: PLEASE DO NOT CITE Epidemiological and Economic Effects of Lockdown Alexander Arnon* Penn Wharton Budget Model John Ricco* Penn Wharton Budget Model Kent Smetters* Penn Wharton Budget Model The Wharton School NBER Abstract We examine the period of national lockdown beginning in March 2020 using an integrated epidemiological-econometric framework in which health and economic outcomes are jointly determined. We augment a state-level compartmental model with behavioral responses to non-pharmaceutical interventions (NPIs) and to local epidemiological conditions. To calibrate the model, we construct daily, county-level measures of contact rates and employment and estimate key parameters with an event study design. We have three main findings: First, NPIs introduced by state and local governments explain a small fraction of the nationwide decline in contact rates but nevertheless reduced COVID-19 deaths by almost 30% percent---saving about 33,000 lives---over the first 3 months of the pandemic. However, NPIs also explain nearly 15% of the decline in employment---around 3 million jobs---over the same period. -

Lockdown Or Lockup
EDITORIAL Lockdown or Lockup James J. James, MD, Dr PH, MHA e are currently wrestling with the crucial clusters of individuals in enclosed spaces. When the question of “reopening” America - when relatively negligible costs of the social distancing W and how. The reason for this is that we measures are compared to the almost catastrophic have seemingly created two competing priorities: socio-economic costs of full lockdown the answer to saving lives vs restoring the economy. No one can guar- this question becomes imperative. It becomes increas- antee the best solution to such a complex and rapidly ingly difficult to support full lockdowns without evolving puzzle and we will not be able to truly assess supporting evidence of significant benefit beyond that the results of today’s decisions for months or even years attained from less extreme social distancing interven- to come. With that in mind, what follows is not meant tions. This is especially true given that all epidemic to provide a solution to this conundrum, but to offer curves eventually flatten out and descend. The current some considerations that might assist in helping to trend of attributing this predetermined outcome to full formulate a strategy with which to approach it. lockdowns in the absence of supporting evidence sets an extremely dangerous precedent going forward and Central to the management of this pandemic is deter- violates a fundamental tenet of science and logic— mining what Public Health interventions to imple- correlation is not causation. ment to best contain and mitigate the impacts of COVID-19. Accepting the fact that all interventions Unfortunately, there is no reliable direct evidence have some cost, the goal is to achieve the desired other than anecdotal that full lockdowns result in outcome with the least overall harm to society.