Thyroid Appendices
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inventory Size (Ml Or G) 103220 Dimethyl Sulfate 77-78-1 500 Ml
Inventory Bottle Size Number Name CAS# (mL or g) Room # Location 103220 Dimethyl sulfate 77-78-1 500 ml 3222 A-1 Benzonitrile 100-47-0 100ml 3222 A-1 Tin(IV)chloride 1.0 M in DCM 7676-78-8 100ml 3222 A-1 103713 Acetic Anhydride 108-24-7 500ml 3222 A2 103714 Sulfuric acid, fuming 9014-95-7 500g 3222 A2 103723 Phosphorus tribromide 7789-60-8 100g 3222 A2 103724 Trifluoroacetic acid 76-05-1 100g 3222 A2 101342 Succinyl chloride 543-20-4 3222 A2 100069 Chloroacetyl chloride 79-04-9 100ml 3222 A2 10002 Chloroacetyl chloride 79-04-9 100ml 3222 A2 101134 Acetyl chloride 75-36-5 500g 3222 A2 103721 Ethyl chlorooxoacetate 4755-77-5 100g 3222 A2 100423 Titanium(IV) chloride solution 7550-45-0 100ml 3222 A2 103877 Acetic Anhydride 108-24-7 1L 3222 A3 103874 Polyphosphoric acid 8017-16-1 1kg 3222 A3 103695 Chlorosulfonic acid 7790-94-5 100g 3222 A3 103694 Chlorosulfonic acid 7790-94-5 100g 3222 A3 103880 Methanesulfonic acid 75-75-2 500ml 3222 A3 103883 Oxalyl chloride 79-37-8 100ml 3222 A3 103889 Thiodiglycolic acid 123-93-3 500g 3222 A3 103888 Tetrafluoroboric acid 50% 16872-11-0 1L 3222 A3 103886 Tetrafluoroboric acid 50% 16872-11-0 1L 3222 A3 102969 sulfuric acid 7664-93-9 500 mL 2428 A7 102970 hydrochloric acid (37%) 7647-01-0 500 mL 2428 A7 102971 hydrochloric acid (37%) 7647-01-0 500 mL 2428 A7 102973 formic acid (88%) 64-18-6 500 mL 2428 A7 102974 hydrofloric acid (49%) 7664-39-3 500 mL 2428 A7 103320 Ammonium Hydroxide conc. -

Synthesis of New Thiazole and Thiazolyl Derivatives of Medicinal Significant-A Short Review
MOJ Bioorganic & Organic Chemistry Mini Review Open Access Synthesis of new thiazole and thiazolyl derivatives of medicinal significant-a short review Abstract Volume 2 Issue 2 - 2018 In the field of therapeutic science, thiazoles are of extraordinary importance, because of their potent and significant biological activities. Likewise thiazole and their Weiam Hussein,1 Gülhan Turan- derivatives are found in various powerful naturally and biologically active compounds Zitouni2 which possess a broad spectrum of biological activity therefore, synthesis of this 1Department of Pharmaceutical Chemistry, Aden University, compound is of remarkable concern. This review primarily focuses on the updated Yemen research papers reported in literature for the synthesis of thiazole and thiazolyl 2Department of Pharmaceutical Chemistry, Anadolu University, compounds. Turkey Keywords: thiazoles, thiazolyl, synthetic procedures, biological activity Correspondence: Weiam Hussein, Anadolu University, Faculty of Pharmacy, Department of Pharmaceutical Chemistry, Eskişehir, Turkey, Tel +905074929053, Email [email protected] Received: February 23, 2018| Published: March 12, 2018 Introduction Kaplancikli et al. 11 reported a simple and three steps-reaction procedure for the synthesis of new benzimidazole-thiazole derivatives. The synthesis of heterocyclic rings has been a fascinating field 4-(1H-benzimidazol-1-yl)benzaldehyde was prepared by reacting in therapeutic science. Various heterocyclic compounds containing 1H-benzimidazole and 4-fluorobenzaldehyde under microwave nitrogen and sulfur have flexible frameworks for drugs development irradiation, then, the reaction between 4-(1H-benzimidazol- and design.1 Thiazole is one of the most intensively studied classes of 1-yl)benzaldehyde and hydrazine carbothioamide gave as a aromatic five-membered heterocyclics. It was first defined by Hantzschresult 2-(4-(1H-benzimidazol-1-yl)benzylidene)hydrazine-1- and Weber in 1887. -
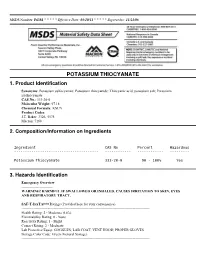
Potassium Thiocyanate 1
MSDS Number: P6181 * * * * * Effective Date: 03/10/11 * * * * * Supersedes: 11/21/08 POTASSIUM THIOCYANATE 1. Product Identification Synonyms: Potassium sulfocyanate; Potassium thiocyanide; Thiocyanic acid, potassium salt; Potassium isothiocyanate CAS No.: 333-20-0 Molecular Weight: 97.18 Chemical Formula: KSCN Product Codes: J.T. Baker: 3326, 5578 Macron: 7168 2. Composition/Information on Ingredients Ingredient CAS No Percent Hazardous --------------------------------------- ------------ ------------ --------- Potassium Thiocyanate 333-20-0 90 - 100% Yes 3. Hazards Identification Emergency Overview -------------------------- WARNING! HARMFUL IF SWALLOWED OR INHALED. CAUSES IRRITATION TO SKIN, EYES AND RESPIRATORY TRACT. SAF-T-DATA(tm) Ratings (Provided here for your convenience) ----------------------------------------------------------------------------------------------------------- Health Rating: 2 - Moderate (Life) Flammability Rating: 0 - None Reactivity Rating: 1 - Slight Contact Rating: 2 - Moderate Lab Protective Equip: GOGGLES; LAB COAT; VENT HOOD; PROPER GLOVES Storage Color Code: Green (General Storage) ----------------------------------------------------------------------------------------------------------- Potential Health Effects ---------------------------------- Inhalation: Causes irritation to the respiratory tract. Symptoms may include coughing, shortness of breath. Ingestion: May cause psychosis, vomiting, disorientation, weakness, low blood pressure, convulsions and death which may be delayed. The probable lethal -

1 Abietic Acid R Abrasive Silica for Polishing DR Acenaphthene M (LC
1 abietic acid R abrasive silica for polishing DR acenaphthene M (LC) acenaphthene quinone R acenaphthylene R acetal (see 1,1-diethoxyethane) acetaldehyde M (FC) acetaldehyde-d (CH3CDO) R acetaldehyde dimethyl acetal CH acetaldoxime R acetamide M (LC) acetamidinium chloride R acetamidoacrylic acid 2- NB acetamidobenzaldehyde p- R acetamidobenzenesulfonyl chloride 4- R acetamidodeoxythioglucopyranose triacetate 2- -2- -1- -β-D- 3,4,6- AB acetamidomethylthiazole 2- -4- PB acetanilide M (LC) acetazolamide R acetdimethylamide see dimethylacetamide, N,N- acethydrazide R acetic acid M (solv) acetic anhydride M (FC) acetmethylamide see methylacetamide, N- acetoacetamide R acetoacetanilide R acetoacetic acid, lithium salt R acetobromoglucose -α-D- NB acetohydroxamic acid R acetoin R acetol (hydroxyacetone) R acetonaphthalide (α)R acetone M (solv) acetone ,A.R. M (solv) acetone-d6 RM acetone cyanohydrin R acetonedicarboxylic acid ,dimethyl ester R acetonedicarboxylic acid -1,3- R acetone dimethyl acetal see dimethoxypropane 2,2- acetonitrile M (solv) acetonitrile-d3 RM acetonylacetone see hexanedione 2,5- acetonylbenzylhydroxycoumarin (3-(α- -4- R acetophenone M (LC) acetophenone oxime R acetophenone trimethylsilyl enol ether see phenyltrimethylsilyl... acetoxyacetone (oxopropyl acetate 2-) R acetoxybenzoic acid 4- DS acetoxynaphthoic acid 6- -2- R 2 acetylacetaldehyde dimethylacetal R acetylacetone (pentanedione -2,4-) M (C) acetylbenzonitrile p- R acetylbiphenyl 4- see phenylacetophenone, p- acetyl bromide M (FC) acetylbromothiophene 2- -5- -

WSAVA List of Essential Medicines for Cats and Dogs
The World Small Animal Veterinary Association (WSAVA) List of Essential Medicines for Cats and Dogs Version 1; January 20th, 2020 Members of the WSAVA Therapeutic Guidelines Group (TGG) Steagall PV, Pelligand L, Page SW, Bourgeois M, Weese S, Manigot G, Dublin D, Ferreira JP, Guardabassi L © 2020 WSAVA All Rights Reserved Contents Background ................................................................................................................................... 2 Definition ...................................................................................................................................... 2 Using the List of Essential Medicines ............................................................................................ 2 Criteria for selection of essential medicines ................................................................................. 3 Anaesthetic, analgesic, sedative and emergency drugs ............................................................... 4 Antimicrobial drugs ....................................................................................................................... 7 Antibacterial and antiprotozoal drugs ....................................................................................... 7 Systemic administration ........................................................................................................ 7 Topical administration ........................................................................................................... 9 Antifungal drugs ..................................................................................................................... -

Illness-Induced Changes in Thyroid Hormone Metabolism: Focus on the Tissue Level
r e V i e W illness-induced changes in thyroid hormone metabolism: focus on the tissue level J. Kwakkel*, E. Fliers, A. Boelen Department of Endocrinology & Metabolism, Academic Medical Center, University of Amsterdam, the Netherlands, *corresponding author: tel.: +31 (0)20-566 67 01, fax: +31 (0)20-691 76 82, e-mail: [email protected] a b s t r a C t during illness changes in thyroid hormone metabolism ring and the outer (tyrosyl) ring of T4 can be deiodinated, occur, collectively known as the non-thyroidal illness ultimately leading to the formation of 3,3’-di-iodothyronine syndrome (NTIS). NTIS is characterised by low serum (T2) (figure 1). thyroid hormone levels without the expected rise in serum thyroid-stimulating hormone, indicating a major change in thyroid hormone feedback regulation. recent studies n o n - t H yroidal illness syndro M e have made clear that during NTIS differential changes in thyroid hormone metabolism occur in various tissues, the During illness many aspects of thyroid hormone net effect of which may be either activation or inhibition of metabolism change, collectively known as the thyroid hormone action. in this review we discuss systemic non-thyroidal illness syndrome (NTIS). The hallmark of and local changes in thyroid hormone metabolism during NTIS is decreased serum thyroid hormone levels without illness, highlighting their physiological implications in an increase in TSH and TRH expression, indicating terms of disease course. the absence of negative feedback regulation. This may represent a useful adaptation of the body to counteract excessive catabolism observed during illness and can be K e y W o r d s viewed as a part of the acute phase response.4 However, especially during prolonged critical illness in the ICU Deiodinase, inflammation, non-thyroidal illness syndrome, setting NTIS may be maladaptative.5 thyroid hormone figure 1. -

IHS National Pharmacy & Therapeutics Committee National
IHS National Pharmacy & Therapeutics Committee National Core Formulary; Last Updated: 09/23/2021 **Note: Medications in GREY indicate removed items.** Generic Medication Name Pharmacological Category (up-to-date) Formulary Brief (if Notes / Similar NCF Active? available) Miscellaneous Medications Acetaminophen Analgesic, Miscellaneous Yes Albuterol nebulized solution Beta2 Agonist Yes Albuterol, metered dose inhaler Beta2 Agonist NPTC Meeting Update *Any product* Yes (MDI) (Nov 2017) Alendronate Bisphosphonate Derivative Osteoporosis (2016) Yes Allopurinol Antigout Agent; Xanthine Oxidase Inhibitor Gout (2016) Yes Alogliptin Antidiabetic Agent, Dipeptidyl Peptidase 4 (DPP-4) Inhibitor DPP-IV Inhibitors (2019) Yes Anastrozole Antineoplastic Agent, Aromatase Inhibitor Yes Aspirin Antiplatelet Agent; Nonsteroidal Anti-Inflammatory Drug; Salicylate Yes Azithromycin Antibiotic, Macrolide STIs - PART 1 (2021) Yes Calcium Electrolyte supplement *Any formulation* Yes Carbidopa-Levodopa (immediate Anti-Parkinson Agent; Decarboxylase Inhibitor-Dopamine Precursor Parkinson's Disease Yes release) (2019) Clindamycin, topical ===REMOVED from NCF=== (See Benzoyl Peroxide AND Removed January No Clindamycin, topical combination) 2020 Corticosteroid, intranasal Intranasal Corticosteroid *Any product* Yes Cyanocobalamin (Vitamin B12), Vitamin, Water Soluble Hematologic Supplements Yes oral (2016) Printed on 09/25/2021 Page 1 of 18 National Core Formulary; Last Updated: 09/23/2021 Generic Medication Name Pharmacological Category (up-to-date) Formulary Brief -

Step-By-Step Guide to Better Laboratory Management Practices
Step-by-Step Guide to Better Laboratory Management Practices Prepared by The Washington State Department of Ecology Hazardous Waste and Toxics Reduction Program Publication No. 97- 431 Revised January 2003 Printed on recycled paper For additional copies of this document, contact: Department of Ecology Publications Distribution Center PO Box 47600 Olympia, WA 98504-7600 (360) 407-7472 or 1 (800) 633-7585 or contact your regional office: Department of Ecology’s Regional Offices (425) 649-7000 (509) 575-2490 (509) 329-3400 (360) 407-6300 The Department of Ecology is an equal opportunity agency and does not discriminate on the basis of race, creed, color, disability, age, religion, national origin, sex, marital status, disabled veteran’s status, Vietnam Era veteran’s status or sexual orientation. If you have special accommodation needs, or require this document in an alternate format, contact the Hazardous Waste and Toxics Reduction Program at (360)407-6700 (voice) or 711 or (800) 833-6388 (TTY). Table of Contents Introduction ....................................................................................................................................iii Section 1 Laboratory Hazardous Waste Management ...........................................................1 Designating Dangerous Waste................................................................................................1 Counting Wastes .......................................................................................................................8 Treatment by Generator...........................................................................................................12 -

Type 3 Lodothyronine Deiodinase: Cloning, in Vitro Expression, and Functional Analysis of the Placental Selenoenzyme
Type 3 lodothyronine deiodinase: cloning, in vitro expression, and functional analysis of the placental selenoenzyme. D Salvatore, … , D L St Germain, P R Larsen J Clin Invest. 1995;96(5):2421-2430. https://doi.org/10.1172/JCI118299. Research Article Type 3 iodothyronine deiodinase (D3) catalyzes the conversion of T4 and T3 to inactive metabolites. It is highly expressed in placenta and thus can regulate circulating fetal thyroid hormone concentrations throughout gestation. We have cloned and expressed a 2.1-kb human placental D3 cDNA which encodes a 32-kD protein with a Km of 1.2 nM for 5 deiodination of T3 and 340 nM for 5' deiodination of reverse T3. The reaction requires DTT and is not inhibited by 6n- propylthiouracil. We quantitated transiently expressed D3 by specifically labeling the protein with bromoacetyl [125I]T3. The Kcat/Km ratio for 5 deiodination of T3 was over 1,000-fold that for 5' deiodination of reverse T3. Human D3 is a selenoenzyme as evidenced by (a) the presence of an in frame UGA codon at position 144, (b) the synthesis of a 32-kD 75Se-labeled protein in D3 cDNA transfected cells, and (c) the presence of a selenocysteine insertion sequence element in the 3' untranslated region of the mRNA which is required for its expression. The D3 selenocysteine insertion sequence element is more potent than that in the type 1 deiodinase or glutathione peroxidase gene, suggesting a high priority for selenocysteine incorporation into this enzyme. The conservation of this enzyme from Xenopus laevis tadpoles to humans implies an essential role for regulation of thyroid hormone inactivation during embryological development. -

Potassium Thiocyanate: a Rare Case Report
Case Report J Forensic Sci & Criminal Inves Volume 13 Issue 2 - November 2019 Copyright © All rights are reserved by R Rajiv DOI: 10.19080/JFSCI.2019.13.555857 A Homicidal Attempt - Potassium Thiocyanate: A Rare Case Report R Rajiv1*, GThirunavukkarasu2 and D Shanmugam3 1Scientific Officer, Regional Forensic Science Laboratory, India 2Deputy Director, Forensic Sciences Département, India 3Deputy Director, Regional Forensic Science Laboratory, India Submission: November 19, 2019, Published: November 26, 2019 *Corresponding author: R Rajiv, Scientific Officer, Regional Forensic Science Laboratory, Villupuram, India Abstract Forensic Toxicologist does tremendous work to find out various poisonous substances from Viscera to other materials pertaining to the crime cases. Potassium Thiocyanate (CAS number 333-20-0) is the chemical compound with the molecular formula KSCN. It is a colourless deliquescent crystals. In this case, one borrower offered a packed Gulab Jamun (Sweet) box to the money lender while returning the borrowed money. While the lender was tasting the sweet, he found some different taste, so he spat and subsequently he rushed to hospital. A criminal case has been registered in this regard, and the case article (Gulab jamun) was forwarded to our Forensic Science Laboratory by the investigating agency.Keywords: After the scrupulous analysis, Potassium Thiocyanate was detected in the content of the said item. Forensic science; Toxicological analysis; Potassium thiocyanate; Gulab jamun Introduction home to return some money and offered a sweet box full of The role of Forensic Toxicologist is to find out various Gulab jamun after a long chat. The lender happily accepted the poisonous substances from viscera and other materials offer as the borrower appealed to him to take some pieces as pertaining to the crime cases. -

Thyroxine Binding to Type III Iodothyronine Deiodinase Craig A
www.nature.com/scientificreports OPEN Thyroxine binding to type III iodothyronine deiodinase Craig A. Bayse*, Eric S. Marsan, Jenna R. Garcia & Alexis T. Tran‑Thompson Iodothyronine deiodinases (Dios) are important selenoproteins that control the concentration of the active thyroid hormone (TH) triiodothyronine through regioselective deiodination. The X‑ray structure of a truncated monomer of Type III Dio (Dio3), which deiodinates TH inner rings through a selenocysteine (Sec) residue, revealed a thioredoxin-fold catalytic domain supplemented with an unstructured Ω-loop. Loop dynamics are driven by interactions of the conserved Trp207 with solvent in multi-microsecond molecular dynamics simulations of the Dio3 thioredoxin(Trx)-fold domain. Hydrogen bonding interactions of Glu200 with residues conserved across the Dio family anchor the loop’s n‑terminus to the active site Ser‑cys-Thr‑Sec sequence. A key long‑lived loop conformation coincides with the opening of a cryptic pocket that accommodates thyroxine (T4) through an I⋯Se halogen bond to Sec170 and the amino acid group with a polar cleft. The Dio3-T4 complex is stabilized by an I⋯O halogen bond between an outer ring iodine and Asp211, consistent with Dio3 selectivity for inner ring deiodination. Non-conservation of residues, such as Asp211, in other Dio types in the fexible portion of the loop sequence suggests a mechanism for regioselectivity through Dio type- specifc loop conformations. Cys168 is proposed to attack the selenenyl iodide intermediate to regenerate Dio3 based upon structural comparison with related Trx-fold proteins. Iodothyronine deiodinase (Dio) membrane selenoproteins regulate thyroid hormone (TH) activity through regioselective deiodination (Fig. 1a)1–10. -

The Interactions Between Selenium and Iodine Deficiencies in Man And
Nutrition Research Reviews (1999), 12, 55±73 55 The interactions between selenium and iodine de®ciencies in man and animals John R. Arthur1*, Geoffrey J. Beckett2 and Julie H. Mitchell1 1Division of Micronutrient and Lipid Metabolism, Rowett Research Institute, Greenburn Road, Bucksburn, Aberdeen AB21 9SB, UK 2University Department of Clinical Biochemistry, The Royal In®rmary, Edinburgh EH3 9YW, UK Abstract Up to one billion people live in areas where they may be at risk from I de®ciency. Many of the debilitating effects of the de®ciency may be irreversible, consequently it is essential to understand the mechanisms whereby lack of I can cause disease 0 through decreased thyroxine and 3,3 ,5-triiodothyronine (T3) synthesis. Since Se has an essential role in thyroid hormone metabolism, it has the potential to play a major part in the outcome of I de®ciency. These effects of Se derive from two aspects of its biological function. First, three Se-containing deiodinases regulate the synthesis and degradation of the biologically active thyroid hormone, T3. Second, selenoperoxidases and possibly thioredoxin reductase (EC 1.6.4.5) protect the thyroid gland from H2O2 produced during the synthesis of thyroid hormones. The mechanisms whereby Se de®ciency exacerbates the hypothyroidism due to I de®ciency have been elucidated in animals. In contrast to these adverse effects, concurrent Se de®ciency may also cause changes in deiodinase activities which can protect the brain from low T3 concentrations in I de®ciency. Animals with Se and I de®ciency have changes in serum thyroid hormone concentrations that are similar to those observed in patients with I de®ciency disease.