Neurology Neurosurgery & Psychiatry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dystonia and Chorea in Acquired Systemic Disorders
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.65.4.436 on 1 October 1998. Downloaded from 436 J Neurol Neurosurg Psychiatry 1998;65:436–445 NEUROLOGY AND MEDICINE Dystonia and chorea in acquired systemic disorders Jina L Janavs, Michael J AminoV Dystonia and chorea are uncommon abnormal Associated neurotransmitter abnormalities in- movements which can be seen in a wide array clude deficient striatal GABA-ergic function of disorders. One quarter of dystonias and and striatal cholinergic interneuron activity, essentially all choreas are symptomatic or and dopaminergic hyperactivity in the nigros- secondary, the underlying cause being an iden- triatal pathway. Dystonia has been correlated tifiable neurodegenerative disorder, hereditary with lesions of the contralateral putamen, metabolic defect, or acquired systemic medical external globus pallidus, posterior and poste- disorder. Dystonia and chorea associated with rior lateral thalamus, red nucleus, or subtha- neurodegenerative or heritable metabolic dis- lamic nucleus, or a combination of these struc- orders have been reviewed frequently.1 Here we tures. The result is decreased activity in the review the underlying pathogenesis of chorea pathways from the medial pallidus to the and dystonia in acquired general medical ventral anterior and ventrolateral thalamus, disorders (table 1), and discuss diagnostic and and from the substantia nigra reticulata to the therapeutic approaches. The most common brainstem, culminating in cortical disinhibi- aetiologies are hypoxia-ischaemia and tion. Altered sensory input from the periphery 2–4 may also produce cortical motor overactivity medications. Infections and autoimmune 8 and metabolic disorders are less frequent and dystonia in some cases. To date, the causes. Not uncommonly, a given systemic dis- changes found in striatal neurotransmitter order may induce more than one type of dyski- concentrations in dystonia include an increase nesia by more than one mechanism. -

Abadie's Sign Abadie's Sign Is the Absence Or Diminution of Pain Sensation When Exerting Deep Pressure on the Achilles Tendo
A.qxd 9/29/05 04:02 PM Page 1 A Abadie’s Sign Abadie’s sign is the absence or diminution of pain sensation when exerting deep pressure on the Achilles tendon by squeezing. This is a frequent finding in the tabes dorsalis variant of neurosyphilis (i.e., with dorsal column disease). Cross References Argyll Robertson pupil Abdominal Paradox - see PARADOXICAL BREATHING Abdominal Reflexes Both superficial and deep abdominal reflexes are described, of which the superficial (cutaneous) reflexes are the more commonly tested in clinical practice. A wooden stick or pin is used to scratch the abdomi- nal wall, from the flank to the midline, parallel to the line of the der- matomal strips, in upper (supraumbilical), middle (umbilical), and lower (infraumbilical) areas. The maneuver is best performed at the end of expiration when the abdominal muscles are relaxed, since the reflexes may be lost with muscle tensing; to avoid this, patients should lie supine with their arms by their sides. Superficial abdominal reflexes are lost in a number of circum- stances: normal old age obesity after abdominal surgery after multiple pregnancies in acute abdominal disorders (Rosenbach’s sign). However, absence of all superficial abdominal reflexes may be of localizing value for corticospinal pathway damage (upper motor neu- rone lesions) above T6. Lesions at or below T10 lead to selective loss of the lower reflexes with the upper and middle reflexes intact, in which case Beevor’s sign may also be present. All abdominal reflexes are preserved with lesions below T12. Abdominal reflexes are said to be lost early in multiple sclerosis, but late in motor neurone disease, an observation of possible clinical use, particularly when differentiating the primary lateral sclerosis vari- ant of motor neurone disease from multiple sclerosis. -

Golisano Restorative Neurology & Rehabilitation
GOLISANO RESTORATIVE NEUROLOGY & REHABILITATION CENTER TABLE OF CONTENTS Letter of Welcome................................................................ 2 Mary L. Dombovy, MD, MHSA Vice President, Neuroscience Institute Introduction to Our Program................................................ 5 Our Services......................................................................... 9 Brain Injury Rehabilitation Stroke Rehabilitation Spinal Cord Rehabilitation General Rehabilitation Pediatric Rehabilitation Patient Outcomes.................................................................12 The Journey Back Home......................................................13 A Special Recognition...........................................................15 A LETTER OF WELCOME In 1989, we began as a small inpatient brain injury rehabilitation unit at St. Mary’s Hospital. Today, the Rochester Regional Health Neuroscience Institute has evolved into a program offering a wide breadth of services for those with neurological and musculoskeletal disorders across a continuum of care from emergency and acute care, to rehabilitation, transitional and home care. As a result of an improved understanding of neurologic recovery, neurologic rehabilitation is evolving into restorative neurology, where we are now beginning to be able to restore loss of function. New approaches such as bodyweight supported training, constraint-induced therapy, functional electrical assistive devices and new methods of brain scanning, are all enhancing our ability to understand how -
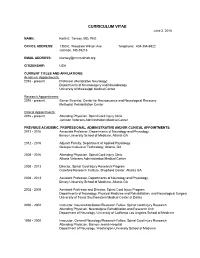
CURRICULUM VITAE June 2, 2016
CURRICULUM VITAE June 2, 2016 NAME: Keith E. Tansey, MD, PhD OFFICE ADDRESS: 1350 E. Woodrow Wilson Ave. Telephone: 404-354-6922 Jackson, MS 39216 EMAIL ADDRESS: [email protected] CITIZENSHIP: USA CURRENT TITLES AND AFFILIATIONS: Academic Appointments: 2016 - present Professor (Restorative Neurology) Departments of Neurosurgery and Neurobiology University of Mississippi Medical Center Research Appointments: 2016 - present Senior Scientist, Center for Neuroscience and Neurological Recovery Methodist Rehabilitation Center Clinical Appointments: 2016 - present Attending Physician, Spinal Cord Injury Clinic Jackson Veterans Administration Medical Center PREVIOUS ACADEMIC, PROFESSIONAL, ADMINISTRATIVE AND/OR CLINICAL APPOINTMENTS: 2013 - 2016 Associate Professor, Departments of Neurology and Physiology, Emory University School of Medicine, Atlanta GA 2012 - 2016 Adjunct Faculty, Department of Applied Physiology Georgia Institute of Technology, Atlanta, GA 2008 - 2016 Attending Physician, Spinal Cord Injury Clinic Atlanta Veterans Administration Medical Center 2008 - 2013 Director, Spinal Cord Injury Research Program Crawford Research Institute, Shepherd Center, Atlanta GA 2008 - 2013 Assistant Professor, Departments of Neurology and Physiology, Emory University School of Medicine, Atlanta GA 2002 - 2008 Assistant Professor and Director, Spinal Cord Injury Program Departments of Neurology, Physical Medicine and Rehabilitation, and Neurological Surgery University of Texas Southwestern Medical Center at Dallas 2000 - 2002 Instructor, Neurorehabilitation/Research -

THE SYNDROMES of the ARTERIES of the BRAIN and SPINAL CORD Part 1 by LESLIE G
65 Postgrad Med J: first published as 10.1136/pgmj.29.328.65 on 1 February 1953. Downloaded from THE SYNDROMES OF THE ARTERIES OF THE BRAIN AND SPINAL CORD Part 1 By LESLIE G. KILOH, M.D., M.R.C.P., D.P.M. First Assistant in the Joint Department of Psychological Medicine, Royal Victoria Infirmary and University of Durham Introduction general circulatory efficiency at the time of the Little interest is shown at present in the syn- catastrophe is of the greatest importance. An dromes of the arteries of the brain and spinal cord, occlusion, producing little effect in the presence of and this perhaps is related to the tendency to a normal blood pressure, may cause widespread minimize the importance of cerebral localization. pathological changes if hypotension co-exists. Yet these syndromes are far from being fully A marked discrepancy has been noted between elucidated and understood. It must be admitted the effects of ligation and of spontaneous throm- that in many cases precise localization is often of bosis of an artery. The former seldom produces little more than academic interest and ill effects whilst the latter frequently determines provides Protected by copyright. nothing but a measure of personal satisfaction to infarction. This is probably due to the tendency the physician. But it is worth recalling that the of a spontaneous thrombus to extend along the detailed study of the distribution of the bronchi affected vessel, sealing its branches and blocking and of the pathological anatomy of congenital its collateral circulation, and to the fact that the abnormalities of the heart, was similarly neglected arterial disease is so often generalized. -

Autologous Stem Cell Therapy for Cerebral Palsy
Open Journal of Pediatrics, 2020, 10, 36-64 https://www.scirp.org/journal/ojped ISSN Online: 2160-8776 ISSN Print: 2160-8741 Autologous Stem Cell Therapy for Cerebral Palsy Sagar Jawale, Vijay Bhaskar, Veeresh Nandikolmath, Shreedhar Patil Jawale Institute of Pediatric Surgery, Jalgaon, Maharashtra, India How to cite this paper: Jawale, S., Bhaskar, Abstract V., Nandikolmath, V. and Patil, S. (2020) Autologous Stem Cell Therapy for Cerebral Introduction: We describe treatment of Cerebral Palsy with adult stem cells Palsy. Open Journal of Pediatrics, 10, 36-64. derived from bone marrow and fat of the same patient. Adult stem cells are of https://doi.org/10.4236/ojped.2020.101004 two types, the mesenchymal and haemopoietic stem cells which have Received: November 5, 2019 potential to duplicate, indefinitely produce 50 types of growth factors that Accepted: January 17, 2020 repair and regenerate tissues in an epigenetic manner. Every organ has its Published: January 20, 2020 own stem cells, for example kidney stem cells, liver stem cells, etc. When spe- cialized cells in an organ get damaged, the local stem cells come forward and Copyright © 2020 by author(s) and Scientific Research Publishing Inc. get differentiated into specialized cells and the tissue damage is replenished. This work is licensed under the Creative But when the stock of this reserve of local stem cell is over, the organ starts Commons Attribution International failing. In autologous stem cell therapy, we harvest stem cells from other License (CC BY 4.0). healthy organs like fat and bone marrow which have abundant stem cells and http://creativecommons.org/licenses/by/4.0/ put them into the diseased organ. -

Post Stroke Focal Aware Seizures Presenting As Delayed Onset Choreoathetosis
Lehigh Valley Health Network LVHN Scholarly Works Department of Medicine Post Stroke Focal Aware Seizures Presenting as Delayed Onset Choreoathetosis Artish Patel USF MCOM - LVHN Campus, [email protected] Patrick Davis USF MCOM - LVHN Campus, [email protected] Beth Stepanczuk MD Lehigh Valley Health Network, [email protected] Follow this and additional works at: https://scholarlyworks.lvhn.org/medicine Part of the Medicine and Health Sciences Commons Published In/Presented At Patel, A., Davis, P., & Stepanczuk, B. (2021, February 9-13). Post Stroke Focal Aware Seizures Presenting as Delayed Onset Choreoathetosis. [Poster presentation]. Association of Academic Physiatrists Annual Meeting, Virtual. This Poster is brought to you for free and open access by LVHN Scholarly Works. It has been accepted for inclusion in LVHN Scholarly Works by an authorized administrator. For more information, please contact [email protected]. Post Stroke Focal Aware Seizures Presenting as Delayed Onset Choreoathetosis Artish Patel, MD, BS, Patrick Davis, MD, BS, and Beth Stepanczuk, MD Lehigh Valley Health Network; Allentown, Pa. Setting Case Description Discussion Outpatient follow-up office She initially presented with acute onset confusion, nausea, This patient offered a rare case of focal aware seizures vomiting, and aphasia. Imaging revealed acute left parietal presenting as delayed onset choreoathetosis of the right Patient temporal intraparenchymal hemorrhage with surrounding upper extremity secondary to acute left parietal temporal 39-year-old female with history of migraines and recent left parietal edema and restricted diffusion consistent with infarction intraparenchymal hemorrhage. It has been documented that temporal intraparenchymal hemorrhage presenting at three- secondary to superior sagittal sinus thrombosis. -

Paraneoplastic Neurological and Muscular Syndromes
Paraneoplastic neurological and muscular syndromes Short compendium Version 4.5, April 2016 By Finn E. Somnier, M.D., D.Sc. (Med.), copyright ® Department of Autoimmunology and Biomarkers, Statens Serum Institut, Copenhagen, Denmark 30/01/2016, Copyright, Finn E. Somnier, MD., D.S. (Med.) Table of contents PARANEOPLASTIC NEUROLOGICAL SYNDROMES .................................................... 4 DEFINITION, SPECIAL FEATURES, IMMUNE MECHANISMS ................................................................ 4 SHORT INTRODUCTION TO THE IMMUNE SYSTEM .................................................. 7 DIAGNOSTIC STRATEGY ..................................................................................................... 12 THERAPEUTIC CONSIDERATIONS .................................................................................. 18 SYNDROMES OF THE CENTRAL NERVOUS SYSTEM ................................................ 22 MORVAN’S FIBRILLARY CHOREA ................................................................................................ 22 PARANEOPLASTIC CEREBELLAR DEGENERATION (PCD) ...................................................... 24 Anti-Hu syndrome .................................................................................................................. 25 Anti-Yo syndrome ................................................................................................................... 26 Anti-CV2 / CRMP5 syndrome ............................................................................................ -

High-Yield Neuroanatomy
LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page i Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page ii Aptara Inc. LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iii Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION James D. Fix, PhD Professor Emeritus of Anatomy Marshall University School of Medicine Huntington, West Virginia With Contributions by Jennifer K. Brueckner, PhD Associate Professor Assistant Dean for Student Affairs Department of Anatomy and Neurobiology University of Kentucky College of Medicine Lexington, Kentucky LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iv Aptara Inc. Acquisitions Editor: Crystal Taylor Managing Editor: Kelley Squazzo Marketing Manager: Emilie Moyer Designer: Terry Mallon Compositor: Aptara Fourth Edition Copyright © 2009, 2005, 2000, 1995 Lippincott Williams & Wilkins, a Wolters Kluwer business. 351 West Camden Street 530 Walnut Street Baltimore, MD 21201 Philadelphia, PA 19106 Printed in the United States of America. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at 530 Walnut Street, Philadelphia, PA 19106, via email at [email protected], or via website at http://www.lww.com (products and services). -

THE SYNDROMES of the ARTERIES of the BRAIN AND, SPINAL CORD Part II by LESLIE G
I19 Postgrad Med J: first published as 10.1136/pgmj.29.329.119 on 1 March 1953. Downloaded from - N/ THE SYNDROMES OF THE ARTERIES OF THE BRAIN AND, SPINAL CORD Part II By LESLIE G. KILOH, M.D., M.R.C.P., D.P.M. First Assistant in the Joint Department of Psychological Medicine, Royal Victoria Infirmary and University of Durham The Vertebral Artery (See also Cabot, I937; Pines and Gilensky, Each vertebral artery enters the foramen 1930.) magnum in front of the roots of the hypoglossal nerve, inclines forwards and medially to the The Posterior Inferior Cerebellar Artery anterior aspect of the medulla oblongata and unites The posterior inferior cerebellar artery arises with its fellow at the lower border of the pons to from the vertebral artery at the level of the lower form the basilar artery. border of the inferior olive and winds round the The posterior inferior cerebellar and the medulla oblongata between the roots of the hypo- Protected by copyright. anterior spinal arteries are its principal branches glossal nerve. It passes rostrally behind the root- and it sometimes gives off the posterior spinal lets of the vagus and glossopharyngeal nerves to artery. A few small branches are supplied directly the lower border of the pons, bends backwards and to the medulla oblongata. These are in line below caudally along the inferolateral boundary of the with similar branches of the anterior spinal artery fourth ventricle and finally turns laterally into the and above with the paramedian branches of the vallecula. basilar artery. Branches: From the trunk of the artery, In some cases of apparently typical throm- twigs enter the lateral aspect of the medulla bosis of the posterior inferior cerebellar artery, oblongata and supply the region bounded ventrally post-mortem examination has demonstrated oc- by the inferior olive and medially by the hypo- clusion of the entire vertebral artery (e.g., Diggle glossal nucleus-including the nucleus ambiguus, and Stcpford, 1935). -

EMERGENCY CARE AID for ALTERNATING HEMIPLEGIA of CHILDHOOD (AHC) PATIENTS a Reference Guide for Medical Professionals
EMERGENCY CARE AID FOR ALTERNATING HEMIPLEGIA OF CHILDHOOD (AHC) PATIENTS A Reference Guide for Medical Professionals AHC DEFINITION: (Handb Clin Neurol. 2013; 112:821-6) Alternating hemiplegia of childhood (AHC) is a very rare disease characterized by recurrent attacks of loss of muscular tone resulting in hypomobility of one side of the body. The etiology of the disease is due to ATP1A3 gene mutations in the majority of patients. AHC has an onset in the first few months of life. Hemiplegic episodes are often accompanied by other paroxysmal manifestations, such as lateral eyes and head deviation toward the hemiplegic side and a very peculiar monocular nystagmus. Movement disorders such as dystonia and abnormal movements are frequent. Cognitive delay of variable degree is a common feature. Epilepsy has been reported in 50% of the cases, but seizure onset is usually during the third or fourth year of life. Many drugs have been used in AHC with very few results. Flunarizine has the most supportive anecdotal evidence regarding efficacy. AHC RISK FACTORS: TREATMENT: (Neurol Genet. 2017 Apr; 3(2): e139) There is no specific treatment for AHC. There is no approved medication or device that alters the underlying deficit in the Na+/K+ pump (see Flunarizine next page). NEUROLOGICAL: (Neurology. 2019 Sep 24;93(13)) Epilepsy is present in over 50% of AHC patients. Epilepsy in AHC can be focal or generalized seizures. Dystonia is also a common feature that affects the majority of patients dealing with AHC. Patients with AHC can deteriorate either abruptly or gradually at the motor and intellectual function level, depending on the severity of their disease. -

High-Yield Neuroanatomy, FOURTH EDITION
LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page i Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page ii Aptara Inc. LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iii Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION James D. Fix, PhD Professor Emeritus of Anatomy Marshall University School of Medicine Huntington, West Virginia With Contributions by Jennifer K. Brueckner, PhD Associate Professor Assistant Dean for Student Affairs Department of Anatomy and Neurobiology University of Kentucky College of Medicine Lexington, Kentucky LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iv Aptara Inc. Acquisitions Editor: Crystal Taylor Managing Editor: Kelley Squazzo Marketing Manager: Emilie Moyer Designer: Terry Mallon Compositor: Aptara Fourth Edition Copyright © 2009, 2005, 2000, 1995 Lippincott Williams & Wilkins, a Wolters Kluwer business. 351 West Camden Street 530 Walnut Street Baltimore, MD 21201 Philadelphia, PA 19106 Printed in the United States of America. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at 530 Walnut Street, Philadelphia, PA 19106, via email at [email protected], or via website at http://www.lww.com (products and services).