A Counseling Guide for Sickle Cell and Other Hemoglobin Variants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosis of Sickle Cell Disease and HBB Haplotyping in the Era of Personalized Medicine: Role of Next Generation Sequencing
Journal of Personalized Medicine Article Diagnosis of Sickle Cell Disease and HBB Haplotyping in the Era of Personalized Medicine: Role of Next Generation Sequencing Adekunle Adekile 1,*, Nagihan Akbulut-Jeradi 2, Rasha Al Khaldi 2, Maria Jinky Fernandez 2 and Jalaja Sukumaran 1 1 Department of Pediatrics, Faculty of Medicine, Kuwait University, P.O. Box 24923, Safat 13110, Kuwait; jalajasukumaran@hotmail 2 Advanced Technology Company, Hawali 32060, Kuwait; [email protected] (N.A.-J.); [email protected] (R.A.); [email protected] (M.J.F.) * Correspondence: [email protected]; Tel.: +965-253-194-86 Abstract: Hemoglobin genotype and HBB haplotype are established genetic factors that modify the clinical phenotype in sickle cell disease (SCD). Current methods of establishing these two factors are cumbersome and/or prone to errors. The throughput capability of next generation sequencing (NGS) makes it ideal for simultaneous interrogation of the many genes of interest in SCD. This study was designed to confirm the diagnosis in patients with HbSS and Sβ-thalassemia, identify any ß-thal mutations and simultaneously determine the ßS HBB haplotype. Illumina Ampliseq custom DNA panel was used to genotype the DNA samples. Haplotyping was based on the alleles on five haplotype-specific SNPs. The patients studied included 159 HbSS patients and 68 Sβ-thal patients, previously diagnosed using high performance liquid chromatography (HPLC). There was Citation: Adekile, A.; considerable discordance between HPLC and NGS results, giving a false +ve rate of 20.5% with a S Akbulut-Jeradi, N.; Al Khaldi, R.; sensitivity of 79% for the identification of Sβthal. -

The Developmental Genetics of Hemoglobin Synthesis in Chironomus Darrel Starr English Iowa State University
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1968 The developmental genetics of hemoglobin synthesis in Chironomus Darrel Starr English Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Genetics Commons Recommended Citation English, Darrel Starr, "The developmental genetics of hemoglobin synthesis in Chironomus " (1968). Retrospective Theses and Dissertations. 3660. https://lib.dr.iastate.edu/rtd/3660 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. This dissertation has been microfilmed exactly as received 6 8-14,785 ENGLISH, Barrel Starr, 1936- THE DEVELOPMENTAL GENETICS OF HEMOGLOBIN SYNTHESIS IN CHIRONOMUS. Iowa State University, Ph.D., 1968 Biology- Genetics University Microfilms, Inc., Ann Arbor, Michigan THE DEVELOPMENTAL GENETICS OF HEMOGLOBIN SYNTHESIS IN CHIRONOMUS by Darrel Starr English A Dissertation Submitted to the Graduate Faculty in Partial Fulfillment of The Requirements for the Degree of DOCTOR OF PHILOSOPHY Major Subject: Genetics Approved: Signature was redacted for privacy. In Charge of MajdA Work Signature was redacted for privacy. Head ^ Major Department Signature was redacted for privacy. -
Hemoglobin C Trait (AC) Hemoglobin Eletrophoresis and a Mean Corpuscular Volume
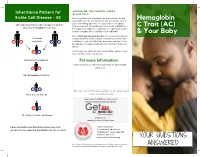
Inheritance Pattern for SHOULD WE, THE PARENTS, TAKE A BLOOD TEST? Sickle Cell Disease - SC Before you have your next baby, we suggest that you and Hemoglobin your partner get special blood test. We all have two sets of genes for hemoglobin. One set is passed on to the baby When one parent has sickle cell trait (AS) and the from each parent. The testing should include, at minimum, a C Trait (AC) other has hemoglobin C trait (AC) hemoglobin eletrophoresis and a mean corpuscular volume. A sickle solubility test (sickledex) is not sufficient! & Your Baby Only if both you and your partner are tested can you know their baby exactly what kind of hemoglobin condition your next child A S may have A C could have. Look carefully at the inheritance pattern for the possibilities of having a baby with the SC form of sickle cell disease. A A A counselor can tell you if any of your future children could have a form of sickle cell disease. AA (normal hemoglobin) For more information or Contact your local SCDAA organization or other health A C agency at: AC (hemoglobin C trait) or A S Or contact the SCDAA National Office at the address and AS (sickle cell trait) or telephone number below. Stay connected with Get Connected the first patient powered registry S C SC (a type of sickle cell disease) Register at www.getconnectedscd.com It does not matter what their other babies have, their Sickle Cell Disease next one has the same four possibilities: AA, AC, AS, or SC. -

Thalassemia, Hemophilia & Sickle Cell Disease
10/22/2018 Global Best Practices in Care, Rehabilitation and Research Thalassemia Syndrome Blood Disorders (Thalassemia, Hemophilia & Sickle Cell Disease) Dr. J.S. Arora Thalassemialogist 7% of the world population MSc in Haemoglobinopathy University College London Carry Thalassemia/Hb’pathy gene General secretary: National Thalassemia Welfare Society Federation of Indian Thalassemics Member Ethics Committee: 400 million heterozygous carriers IIT Delhi Lady Hardinge Medical College and Associated Hospitals, New Delhi ITS Dental College Hospital & Research Centre, Greater NOIDA 3,00,000-4,00,000 babies with severe Founder Member: Indian Alliance of Patient Groups haemoglobinopathies born each year. Founding Trustee: Genomics And Public Health Foundation Formerly Coordinator Thalassemia Cell Govt. of Delhi Member Advisory Committee - D D U Hospital Govt. of Delhi INDIA , THAILAND AND INDONESIA “Life Time Service Award” from PHO Chambers of IAP ► 50% OF WORLD’S THALASSAEMIA CARRIERS Patients for Patient Safety (PFPS) Champion India Member: Patients for Patient Safety Advisory Group ► 50% OF THALASSAEMIA MAJORS [email protected] β Thalassemia Who are affected 100 million carriers of β Thalassemia. More than 100,000 Thalassemia Major born/year India • thalassemia : Carrier rate 1% - 17% (mean 3.9%) more prevalent in certain communities. 50 million carriers, Over 12,000 affected born every year. • Sickle Cell Disease : common in tribes carrier rate as high as 40% in some areas • HbE : Highly prevalent in West Bengal & North Eastern -

Impact of Heterozygous Hemoglobin E on Six Commercial Methods for Hemoglobin A1c Measurement
Impact of heterozygous hemoglobin E on six commercial methods for hemoglobin A1c measurement Sharon Yong1, Hong Liu1, Cindy Lye Teng Lum2, Qian Liu2, Sin Ye Sim3, Felicia Fu Mun Chay3, Wan Ling Cheng4, Siew Fong Neo4, Suru Chew4, Lizhen Ong4, Tze Ping Loh4, Qinde Liu1, Tang Lin Teo1 and Sunil Kumar Sethi4 1 Chemical Metrology Division, Health Sciences Authority, Singapore, Singapore 2 Department of Pathology, Sengkang General Hospital, Singapore, Singapore 3 Department of Laboratory Medicine, Alexandra Hospital, Singapore, Singapore 4 Department of Laboratory Medicine, National University Hospital, Singapore, Singapore ABSTRACT Background: This study examined the impact of heterozygous HbE on HbA1c measurements by six commonly used commercial methods. The results were compared with those from a modified isotope-dilution mass spectrometry (IDMS) reference laboratory method on a liquid chromatograph coupled with tandem mass spectrometer (LC-MS/MS). Methods: Twenty-three leftover samples of patients with heterozygous HbE (HbA1c range: 5.4–11.6%), and nineteen samples with normal hemoglobin (HbA1c range: 5.0–13.7%) were included. The selected commercial methods included the Tina-quant HbA1c Gen. 3 (Roche Diagnostics, Basel, Switzerland), Cobas B 101 (Roche Diagnostics, Basel, Switzerland), D100 (Bio-Rad Laboratories, Hercules, CA, USA), Variant II Turbo HbA1c 2.0 (Bio-Rad Laboratories, Hercules, CA, USA), DCA Vantage (Siemens Healthcare, Erlangen, Germany) and HbA1c Advanced (Beckman Coulter Inc., Brea, CA, USA). Results: With the exception of Cobas B 101 and the Variant II Turbo 2.0, the 95% confidence intervals of the Passing–Bablok regression lines between the results Submitted 25 September 2020 from the six commercial methods and the IDMS method overlapped. -

224 Subpart H—Hematology Kits and Packages
§ 864.7040 21 CFR Ch. I (4–1–02 Edition) Subpart H—Hematology Kits and the treatment of venous thrombosis or Packages pulmonary embolism by measuring the coagulation time of whole blood. § 864.7040 Adenosine triphosphate re- (b) Classification. Class II (perform- lease assay. ance standards). (a) Identification. An adenosine [45 FR 60611, Sept. 12, 1980] triphosphate release assay is a device that measures the release of adenosine § 864.7250 Erythropoietin assay. triphosphate (ATP) from platelets fol- (a) Identification. A erythropoietin lowing aggregation. This measurement assay is a device that measures the is made on platelet-rich plasma using a concentration of erythropoietin (an en- photometer and a luminescent firefly zyme that regulates the production of extract. Simultaneous measurements red blood cells) in serum or urine. This of platelet aggregation and ATP re- assay provides diagnostic information lease are used to evaluate platelet for the evaluation of erythrocytosis function disorders. (increased total red cell mass) and ane- (b) Classification. Class I (general mia. controls). (b) Classification. Class II. The special [45 FR 60609, Sept. 12, 1980] control for this device is FDA’s ‘‘Docu- ment for Special Controls for Erythro- § 864.7060 Antithrombin III assay. poietin Assay Premarket Notification (a) Identification. An antithrombin III (510(k)s).’’ assay is a device that is used to deter- [45 FR 60612, Sept. 12, 1980, as amended at 52 mine the plasma level of antithrombin FR 17733, May 11, 1987; 65 FR 17144, Mar. 31, III (a substance which acts with the 2000] anticoagulant heparin to prevent co- agulation). This determination is used § 864.7275 Euglobulin lysis time tests. -

Fetal and Embryonic Haemoglobins P
Review Article J Med Genet: first published as 10.1136/jmg.10.1.50 on 1 March 1973. Downloaded from Journal of Medical Genetics (1973). 10, 50. Fetal and Embryonic Haemoglobins P. A. LORKIN MRC Abnormal Haemoglobin Unit, University Department of Biochemistry, Cambridge Haemoglobin has been the subject of intensive form a nearly spherical molecule with extensive research for many years and is one of the most areas of contact between unlike chains; the two thoroughly understood of all protein molecules. main types of contact are denoted alp, and alg2 The amino-acid sequences of haemoglobins from The tetramer exhibits cooperative behaviour or many species of animals have been determined haem-haem interaction. As each haem combines (tabulated by Dayhoff, 1969) and the molecular with oxygen the affinity of successive haems in- structures of horse and human haemoglobins have creases. The oxygen affinity curve of the tetramer been determined in great detail by x-ray crystallo- is sigmoidal and may be represented approximately graphy (Perutz et al, 1968a and b; Perutz 1969). A by the Hill equation:* mechanism of action of haemoglobin has been pro- = kpo2n posed (Perutz, 1970a and b and 1972). The y haemoglobins of higher organisms share a common +kpo2n tetrameric structure built up of two pairs of unlike Oxygen affinity data are usually presented in copyright. chains; the a chains containing 141 amino-acid terms of P102, the partial pressure of oxygen re- residues and the non-a chains containing generally quired to attain half saturation with oxygen, and of 145 or 146 amino acids. In man, five types of n, the exponent of the Hill equation. -

A Distant Gene Deletion Affects Beta-Globin Gene Function in an Atypical Gamma Delta Beta-Thalassemia
A distant gene deletion affects beta-globin gene function in an atypical gamma delta beta-thalassemia. P Curtin, … , A D Stephens, H Lehmann J Clin Invest. 1985;76(4):1554-1558. https://doi.org/10.1172/JCI112136. Research Article We describe an English family with an atypical gamma delta beta-thalassemia syndrome. Heterozygosity results in a beta-thalassemia phenotype with normal hemoglobin A2. However, unlike previously described cases, no history of neonatal hemolytic anemia requiring blood transfusion was obtained. Gene mapping showed a deletion that extended from the third exon of the G gamma-globin gene upstream for approximately 100 kilobases (kb). The A gamma-globin, psi beta-, delta-, and beta-globin genes in cis remained intact. The malfunction of the beta-globin gene on a chromosome in which the deletion is located 25 kb away suggests that chromatin structure and conformation are important for globin gene expression. Find the latest version: https://jci.me/112136/pdf A Distant Gene Deletion Affects ,8-Globin Gene Function in an Atypical '6y5-Thalassemia Peter Curtin, Mario Pirastu, and Yuet Wai Kan Howard Hughes Medical Institute and Department ofMedicine, University of California, San Francisco, California 94143 John Anderson Gobert-Jones Department ofPathology, West Suffolk County Hospital, Bury St. Edmunds IP33-2QZ, Suffolk, England Adrian David Stephens Department ofHaematology, St. Bartholomew's Hospital, London ECIA-7BE, England Herman Lehmann Department ofBiochemistry, University ofCambridge, Cambridge CB2-lQW, England Abstract tologic picture of f3-thalassemia minor in adult life. Globin syn- thetic studies reveal a ,3 to a ratio of -0.5, but unlike the usual We describe an English family with an atypical 'yS6-thalassemia fl-thalassemia heterozygote, the levels of HbA2 (and HbF) are syndrome. -

Homozygous Delta-Beta Thalassemia in a Child: a Rare Cause of Elevated Fetal Hemoglobin
Case Report Homozygous delta-beta Thalassemia in a Child: a Rare Cause of Elevated Fetal Hemoglobin Verma S MD1, Bhargava M MD2, Mittal SK MD 3, Gupta R MD4 1. Senior Resident, Department of Pathology, Chacha Nehru Bal Chikitsalaya, Delhi,India. 2. Consultant Pathologist, Department of Pathology, Pushpanjali Crosslay Hospital,India. 3. Director & Senior Consultant, Department of Pediatrics, Pushpanjali Crosslay Hospital,India. 4. Assistant Professor and Head, Departments of Pathology, Chacha Nehru Bal Chikitsalaya, Delhi,India. Received: 15 November 2012 Accepted: 26 January 2013 Abstract Background complete absence of HbA and HbA2 with HbF Delta beta (δβ) thalassemia is an unusual variant of constituting 100% of the hemoglobin. Hemoglobin thalassemia with elevated level of fetal hemoglobin analysis of both parents showed elevated level of (HbF). Homozygous patients of this disorder, unlike HbF with normal HbA2. A final diagnosis of δβ- β-thalassemia, show mild anemia. Only few cases of thalassemia in the child with both parents being δβ-thalassemia have been reported from India in the carriers was rendered. available indexed English literature. Conclusion Case presentation Delta beta-thalassemia is an uncommon cause of A four-year old male child was evaluated for recent- markedly elevated fetal hemoglobin beyond fetal onset jaundice. Hematological investigations showed period. Clinical and haematological parameters mild anemia with microcytic hypochromic red cells. should be evaluated to render an accurate diagnosis. A comprehensive analysis of hemoglobin by high- Key Words performance liquid chromatography (HPLC) showed Delta-Beta Thalassemia ;Homozygote; Chromatography, High Pressure Liquid Corresponding Author Ruchika Gupta,Department of Pathology,Chacha Nehru Bal Chikitsalaya (Associate Hospital of Maulana Azad Medical College),Geeta Colony,Delhi (India), E-mail: [email protected] Introduction confirmatory test for diagnosis of this rare disorder Delta beta (δβ) thalassemia is an infrequent cause of (4). -

Physiology & Biophysics
DEPARTMENTAL RESOURCES The Department of Physiology & Biophysics plays a unique role in biological research. It is in effect a conduit through which the powerful techniques and tools of the physical sciences are brought to bear on significant problems of biological importance. The range of problems being addressed in the Department runs the gamut from understanding functionally important atomic scale motions of proteins to characterizing complex behavior on the cellular through organelle level. The tools being used to pursue these cutting edge problems include state of the art instrumentation for magnetic resonance, laser and synchrotron radiation spectroscopies as well as extensive computer modeling. The strength of the Department stems not only from the significant problems that are being aggressively addressed by the departmental faculty, but also from the resources and the collaborative spirit with the department. The Department houses several world class spectroscopy facilities: Biomolecular Laser Research Center (BLRC) The BLRC is composed of three interrelated laser oriented facilities. The laser spectroscopy facility (LSF) contains an extensive array of state-of-the-art laser spectroscopic tools devoted to studying structure, function and dynamics in isolated biomolecules. The laser imaging and microscopy facility (L1MF) focuses on interfacing laser spectroscopy with microscopy to study complex systems at the molecular level. The third facility, devoted to laser based diagnostic tools for clinical applications, is still in the development stage. Pulsed EPR Facility The EPR facility consists of a number of state-of-the-art spectrometers that have been constructed at Einstein. Both theoretical work and experiments are being carried out to define the structure of metal binding sites in metalloproteins and to determine the orientation and distance of substrates to metal centers at active sites of metalloenzymes. -

Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant
Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease 1 Produced by St. Jude Children’s Research Hospital Departments of Hematology, Patient Education, and Biomedical Communications. Funds were provided by St. Jude Children’s Research Hospital, ALSAC, and a grant from the Plough Foundation. This document is not intended to take the place of the care and attention of your personal physician. Our goal is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specifi c treatment options should be discussed with your physician. For more general information on sickle cell disease, please visit our Web site at www.stjude.org/sicklecell. Copyright © 2009 St. Jude Children’s Research Hospital How did bone marrow (stem cell) transplants begin for children with sickle cell disease? Bone marrow (stem cell) transplants have been used for the treatment and cure of a variety of cancers, immune system diseases, and blood diseases for many years. Doctors in the United States and other countries have developed studies to treat children who have severe sickle cell disease with bone marrow (stem cell) transplants. How does a bone marrow (stem cell) transplant work? 2 In a person with sickle cell disease, the bone marrow produces red blood cells that contain hemoglobin S. This leads to the complications of sickle cell disease. • To prepare for a bone marrow (stem cell) transplant, strong medicines, called chemotherapy, are used to weaken or destroy the patient’s own bone marrow, stem cells, and infection fi ghting system. -

8.5 X12.5 Doublelines.P65
Cambridge University Press 978-0-521-87519-6 - Disorders of Hemoglobin: Genetics, Pathophysiology, and Clinical Management, Second Edition Edited by Martin H. Steinberg, Bernard G. Forget, Douglas R. Higgs and David J. Weatherall Index More information anti-inflammatory therapy, 762–763 thalassemia-related complications, 779 sulfasalazine, nuclear factor (NF)-kB, 762 transplant-related complications, 778–779 targeting ET-1, 762–763 S-linked haplotypes, African/Indo-European, anti-oxidant therapy targeting erythrocyte, 638–640 765–766 burst forming unit-erythroid (BFU-E), 10, 29 deferiprone, 765 oral glutamine, 765 calcium-activated potassium channel (Gardos oral N-acetyl-cysteine, 765–766 pathway), 167–168 anti-oxidant therapy targeting vascular, 763–765 capillary electrophoresis, 660 Index Apo A-I mimetics, 764 capillary IEF, 660 NO, 763–764 carbon monoxide poisoning, 613–616 statins, 764 clinical features, 615 xanthine oxidase inhibitors, 764–765 diagnosis, treatment, 615–616 anti-thrombotic therapy epidemiology, 613–614 -thalassemia, 761–762 cardiac, arterial abnormalities, 151 sickle cell disease, 761–762 cardiac abnormalities, ATRX syndrome, 305 aortagonad-mesonephros (AGM), 6 cardiovascular disease, 652 Apo A-I mimetics, 764 cation content, cellular hydration, 164–172 apoptosis, vasculature permeability, 193–194 calcium-activated potassium channel, 167–168 assays, assay systems, 7, 142 cation permeability alterations, 166–167 ATMDS. See ␣ thalassemia-myelodysplastic cell calcium, calcium pump activity, 167 syndromes cell sodium,