Breathing Air Quality, Sampling and Testing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -
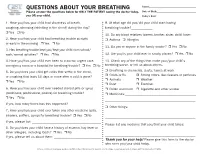
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7. -

Diving Air Compressor - Wikipedia, the Free Encyclopedia Diving Air Compressor from Wikipedia, the Free Encyclopedia
2/8/2014 Diving air compressor - Wikipedia, the free encyclopedia Diving air compressor From Wikipedia, the free encyclopedia A diving air compressor is a gas compressor that can provide breathing air directly to a surface-supplied diver, or fill diving cylinders with high-pressure air pure enough to be used as a breathing gas. A low pressure diving air compressor usually has a delivery pressure of up to 30 bar, which is regulated to suit the depth of the dive. A high pressure diving compressor has a delivery pressure which is usually over 150 bar, and is commonly between 200 and 300 bar. The pressure is limited by an overpressure valve which may be adjustable. A small stationary high pressure diving air compressor installation Contents 1 Machinery 2 Air purity 3 Pressure 4 Filling heat 5 The bank 6 Gas blending 7 References 8 External links A small scuba filling and blending station supplied by a compressor and Machinery storage bank Diving compressors are generally three- or four-stage-reciprocating air compressors that are lubricated with a high-grade mineral or synthetic compressor oil free of toxic additives (a few use ceramic-lined cylinders with O-rings, not piston rings, requiring no lubrication). Oil-lubricated compressors must only use lubricants specified by the compressor's manufacturer. Special filters are used to clean the air of any residual oil and water(see "Air purity"). Smaller compressors are often splash lubricated - the oil is splashed around in the crankcase by the impact of the crankshaft and connecting A low pressure breathing air rods - but larger compressors are likely to have a pressurized lubrication compressor used for surface supplied using an oil pump which supplies the oil to critical areas through pipes diving at the surface control point and passages in the castings. -

Effect of Dead Space on Breathing Stability at Exercise in Hypoxia Eric Hermand, François Lhuissier, Jean-Paul Richalet
Effect of dead space on breathing stability at exercise in hypoxia Eric Hermand, François Lhuissier, Jean-Paul Richalet To cite this version: Eric Hermand, François Lhuissier, Jean-Paul Richalet. Effect of dead space on breathing sta- bility at exercise in hypoxia. Respiratory Physiology & Neurobiology, 2017, 246, pp.26-32. 10.1016/j.resp.2017.07.008. hal-03189523 HAL Id: hal-03189523 https://hal.archives-ouvertes.fr/hal-03189523 Submitted on 3 Apr 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. 1 Effect of dead space on breathing stability at exercise in hypoxia. 2 3 Eric Hermand1, François J Lhuissier1,2, Jean-Paul Richalet1 4 5 1Université Paris 13, Sorbonne Paris Cité, Laboratoire “Hypoxie et poumon”, EA2363, 6 Bobigny, France 7 2Assistance Publique-Hôpitaux de Paris, Hôpital Avicenne, Service de Physiologie, 8 explorations fonctionnelles et médecine du sport, 93009 Bobigny, France 9 10 11 Corresponding author [email protected] (J.P. Richalet) [email protected] (E. Hermand) 12 13 Laboratoire “Hypoxie & poumon”, EA2363 14 74 rue Marcel Cachin 15 93017 Bobigny Cedex, FRANCE 16 Tel: +33148387758 / Fax: +33148388924 17 18 19 Word count for manuscript: 2946 20 21 22 Key words: Control of ventilation, hypoxia, exercise, periodic breathing, breathing 23 instability, dead space, alveolar ventilation 24 25 26 27 28 29 30 Abstract 31 Recent studies have shown that normal subjects exhibit periodic breathing when submitted to 32 concomitant environmental (hypoxia) and physiological (exercise) stresses. -

Advice on Positional Asphyxia
POSITIONAL (OR RESTRAINT) ASPHYXIA FACTSHEET This factsheet should be provided to anyone undergoing physical intervention training. Its contents should be emphasised during training to remind learners of the dangers of certain kinds of restraint and signs of impending asphyxiation. INTRODUCTION Although uncommon, deaths can and do occur following the restraint. A particular risk occurs in certain kinds of restraint. These deaths have frequently been attributed to positional or restraint asphyxia. Staff who use physical interventions must be trained and made aware of the: ● mechanism of restraint ● potential dangers associated with certain restraints ● adverse effects of restraints ● early warning signs of potential harm WHAT IS POSITIONAL OR RESTRAINT ASPHYXIA? Positional or restraint asphyxia is where the subject’s body position during the restraint causes asphyxiation. There are a number of adverse effects, the more common of which include: ● inability or difficulty in breathing ● feeling sick or being sick ● developing swelling to the face and neck areas ● developing pinpoint-sized haemorrhages (small blood spots) to the head, neck and chest areas brought about by asphyxiation (petechiae) RESTRAINT AND BREATHING Being able to expand one’s chest is essential to breathing as this serves to draw air into the lungs. Minimal chest movement is needed during periods of inactivity or rest. However, following exertion or upset the body requires a great deal more oxygen and both the rate and depth of breathing increases so as to cater for this additional oxygen requirement. Increased lung inflation is achieved by way of increased muscle activity in the chest wall and abdomen as well as in the shoulders and neck. -

Cheat Sheet Factors That Affect Oxygen Toxicity
Cheat Sheet Factors that Affect Oxygen Toxicity This quick reference guide is excerpted from Dr. Eric Kindwall’s chapters “The Use of Drugs Under Pressure” and “Contraindications and Side Effects to Hyperbaric Oxygen Treatment” in Hyperbaric Medicine Practice, 3rd edition. www.BestPub.com All Rights Reserved Copyright Best Publishing Company. All Rights Reserved. www.BestPub.com DRUGS THAT POTENTIATE OXYGEN TOXICITY Steroids It is well known that the administration of adrenal corticosteroids can potentiate oxygen toxicity. There seems to be an increase in epinephrine and adrenocortical hormones in response to the stress of hyperbaric oxygen. Normally, the elaboration of these substances in response to stress serves as a protective mechanism. The reverse seems to be true in oxygen toxicity. Steroids and adrenaline seem to further sensitize the organism.1 In clinical practice, hyperbaricists are often called upon to treat people who are receiving steroids. It is a good idea to carefully watch the patient who is receiving high dose steroids and to give anticonvulsant drugs, prophylactically, if necessary. Frequent air breaks are often used. It has been our experience that patients on steroids may develop premonitory signs of oxygen toxicity more quickly than normal. Steroid mediated seizures have not been seen in patients exposed to U.S. Navy Tables 5 and 6, probably because of the short exposures to oxygen between air breaks. We treated one patient with Addison’s disease who was receiving maintenance steroids. Since in this patient the addition of the hyperbaric oxygen stress caused no further elaboration of adrenocortical hormones, the patient was not at any greater risk for oxygen toxicity, despite the fact that she was receiving exogenous steroid hormones. -

Instructions for Focused Breathing
INSTRUCTIONS FOR FOCUSED BREATHING Rationale One technique for dealing with distressing feeling states involves decreasing your physiological arousal using breathing retraining. When people are in an aroused state they tend to breathe from their chest and also to breathe more quickly and deeply, taking in too much oxygen. This can actually increase symptoms of anxiety, including dizziness, breathlessness and even disorientation. The aim of this exercise is to slow down your breathing and decrease the amount of oxygen you take in, which will lead to a decrease in anxiety. It can also be used to manage states of irritation or anger and as a meditative tool for feeling calm and grounded. Procedure for Diaphragmatic Breathing: Getting started : Place one hand on your chest and the other on your stomach. Take a slow deep breath, and pay attention to which hand moves. When breathing from the diaphragm only the stomach hand should move up and down (or mostly). It can help to think of how babies sleep, how their tummy moves up and down. Or you might imagine your stomach as a balloon, filling with air and expanding as you inhale, then letting out the air and shrinking as you exhale. Slow down your rate of breathing: Take in enough air to fill the space, then let it out slowly. Sometimes breathing out through the nose is easier because it is a smaller opening, which will help to control the rate of exhalation. Pause briefly after exhaling before inhaling again. Some people tend to hold their breath too long at first; the pause should come after exhaling. -

Control of Breathing in Hypercapnic Patients with Obstructive Sleep Apnoea
Eur Respir J, 1996, 9, 1576–1577 Copyright ERS Journals Ltd 1996 DOI: 10.1183/09031936.96.09071576 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 CORRESPONDENCE Control of breathing in hypercapnic patients with obstructive sleep apnoea To the Editor: capacity (VC) 4.2±0.8 L (85±8% predicted), forced expi- ratory volume in one second (FEV1) 3.2±0.6 L (83±5% We read with great interest the article by LIN [1] recently pred), FEV1 as percentage of vital capacity (FEV1/VC) published in the Journal. The author described six patients 76±2%. ∆ ∆ with pure obstructive sleep apnoea (OSA), initially pre- The results of V'E, P0.2 and Pa,CO2 in each patient senting with hypercapnia, which was resolved after 2 are presented in table 1. Only three patients had decreased weeks of continuous positive airway pressure (CPAP) ∆V'E; others had ∆V'E slightly increased or within normal ∆ -1 treatment. limits for our laboratory ( V'E/Pa,CO2 2.1±0.4 L·min /mmHg) It is well-known that hypercapnia is more frequent in [2]. Four patients had decreased mouth occlusion pres- patients with OSA and co-existing chronic obstructive sure response to hypercapnia, two had ∆P0.2 within nor- ∆ pulmonary disease (COPD) than in patients with pure mal limits (predicted for our laboratory: P0.2/Pa,CO2 ∆ OSA [2–4]. Among 93 patients referred to our Sleep 0.7±0.25 cmH2O/mmHg [2]), and one had increased P0.2. Laboratory, in whom the diagnosis of OSA was con- Patients were given nasal CPAP treatment, which firmed by full polysomnography, we found 22 subjects reduced AHI to 6±4. -

Surface Supply Breathing Requirements / Recommendations for Kirby Morgan Helmets & Band Masks
SURFACE SUPPLY BREATHING REQUIREMENTS / RECOMMENDATIONS FOR KIRBY MORGAN HELMETS & BAND MASKS Surface Supply Breathing Requirements / Recommendations For Kirby Morgan Helmets & Band Masks TABLE OF CONTENTS Pages Terms / Definitions 3 Introduction 4 Formulas / Conversions 4 Measuring Breathing Performance 4 Work Rates as RMV 5 Breathing Resistive Effort 5 Breathing Performance Requirements 6 Diver Work Rates 7 Symptoms of Inadequate Supply 8 Free Flow and Demand Mode Systems 9 Umbilicals 10 Volume Tanks 11 Free Flow Helmet Air Pressure / Volume Requirements 12 Demand Mode Air Requirements 13 New KMDSI Supply Pressure Tables 13 Standard KMDSI Surface Supply Pressure Formula – OLD Method 14 Demand Mode Diving Using Low Pressure Compressors 14 Volume and Pressure Requirements 15-16 Low Pressure Compressor Flow Testing 17 HP Control Panel / Console 18 HP Control Panel / Console Flow Testing 19 Umbilical Flow Testing 20-21 Appendix A – LP Table – Helmets & Masks W/ SF and SF350 Reg 22-23 Appendix A – LP Table – Rex Regulator / KM-47 / KM-77 24-25 Appendix A – LP Table – KM-57 26-27 Appendix A – HP Table – SF and SF350 Reg 28 Appendix A – HP Table – Rex Regulator / KM-47 / KM-77 29 Appendix A - LP Table - 455 Stainless Steel Balanced Regulator 30 Appendix A – HP Table – 455 Stainless Steel Balanced Regulator 31 Figure 1 & Figure 2 32 Summary 33-34 2 © 2019 Dive Lab Inc® All rights reserved. © 2019 Kirby Morgan Dive Systems, Inc. All rights reserved. Revised April 17, 2019 Surface Supply Breathing Requirements / Recommendations For Kirby Morgan Helmets & Band Masks TERMS / DEFINITIONS ACFM: Actual Cubic Feet per Minute, measured at depth ALPM: Actual Liters per Minute, measured at depth Ambient Pressure: Surrounding pressure Atmosp heres Absolute: Depth in atmospheres + 1 (counts surface pressure as 1 Atm., which is added to total.) Bar: Metric pressure measurement, one BAR = 14.5 PSIG BPM: Breaths per Minute CFM: Cubic feet per minute EGS: Emergency Gas System EXH MBR: Exhalation Pressure in Millibars EXH WOB: Exhalation Work of Breathing I.D. -

BREATHING AIR CATALOG We Can Fill Your Needs CONTENTS SYSTEMS SERVICE TRAINING WORLDWIDE
SYSTEMS SERVICE TRAINING WORLDWIDE BREATHING AIR CATALOG We Can Fill Your Needs CONTENTS SYSTEMS SERVICE TRAINING WORLDWIDE Purely the right choice MISSION STATEMENT Our mission at BAUER COMPRES- SORS INC. is to provide the highest quality products and solutions for high pressure air and gas, geared towards industrial and breathing air applications. We are committed to use the latest technology, best materials, most qualified human resources and the most efficient fabrication techniques. As a result, our equipment solutions offer superior performance along with best value, which are delivered on time, defect free and are supported to achieve their maximum potential throughout their entire lifecycle. CONTENTS SYSTEMS 2 SERVICE TRAINING WORLDWIDE Contents DIVE PRODUCTS / 01 04 Portables 06 Dive Mate DIVE AND FIRE PRODUCTS / 02 08 Vertecon 10 Mini and Maxi Verticus 12 Mariner 320 14 Offshore FIRE PRODUCTS / 03 16 Open Designs 18 Engine Driven 20 Mini Unicus 22 Unicus III 24 Tcom Lite 26 Tcom Trailer ACCESSORIES / 04 28 Air Storage 30 Auto Cascade 33 Containment Fill Stations 34 Purification 36 Quick Reference Guide 3 PORTABLES 3-Stage High Pressure Breathing Air Compressors Pressure 5000 psig 345 bar Charging Rate 2.9 to 4.9 scfm 82 to 139 l/min Power 2 to 6 hp 1.5 to 4.5 kW JUNIOR II and OCEANUS, complete with air purification system and fill hose are safe, reliable three stage compressors designed for serious sport divers. Available in single phase 115/230 VAC and three phase 230/460 VAC electric motor, gasoline or diesel engine drive. www.bauercomp.com BAUER COMPRESSORS INC.