Control of Breathing in Hypercapnic Patients with Obstructive Sleep Apnoea
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Breathing & Buoyancy Control: Stop, Breathe, Think, And
Breathing & Buoyancy control: Stop, Breathe, Think, and then Act For an introduction to this five part series see: House of Cards 'As a child I was fascinated by the way marine creatures just held their position in the water and the one creature that captivated my curiosity and inspired my direction more than any is the Nautilus. Hanging motionless in any depth of water and the inspiration for the design of the submarine with multiple air chambers within its shell to hold perfect buoyancy it is truly a grand master of the art of buoyancy. Buoyancy really is the ultimate Foundation skill in the repertoire of a diver, whether they are a beginner or an explorer. It is the base on which all other skills are laid. With good buoyancy a problem does not become an emergency it remains a problem to be solved calmly under control. The secret to mastery of buoyancy is control of breathing, which also gives many additional advantages to the skill set of a safe diver. Calming one's breathing can dissipate stress, give a sense of well being and control. Once the breathing is calmed, the heart rate will calm too and any situation can be thought through, processed and solved. Always ‘Stop, Breathe, Think and then Act.' Breath control is used in martial arts as a control of the flow of energy, in prenatal training and in child birth. At a simpler more every day level, just pausing to take several slow deep breaths can resolve physical or psychological stress in many scenarios found in daily life. -

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Apnea and Control of Breathing Christa Matrone, M.D., M.Ed
APNEA AND CONTROL OF BREATHING CHRISTA MATRONE, M.D., M.ED. DIOMEL DE LA CRUZ, M.D. OBJECTIVES ¢ Define Apnea ¢ Review Causes and Appropriate Evaluation of Apnea in Neonates ¢ Review the Pathophysiology of Breathing Control and Apnea of Prematurity ¢ Review Management Options for Apnea of Prematurity ¢ The Clinical Evidence for Caffeine ¢ The Role of Gastroesophageal Reflux DEFINITION OF APNEA ¢ Cessation of breathing for greater than 15 (or 20) seconds ¢ Or if accompanied by desaturations or bradycardia ¢ Differentiate from periodic breathing ¢ Regular cycles of respirations with intermittent pauses of >3 S ¢ Not associated with other physiologic derangements ¢ Benign and self-limiting TYPES OF APNEA CENTRAL ¢ Total cessation of inspiratory effort ¢ Absence of central respiratory drive OBSTRUCTIVE ¢ Breathing against an obstructed airway ¢ Chest wall motion without nasal airflow MIXED ¢ Obstructed respiratory effort after a central pause ¢ Accounts for majority of apnea in premature infants APNEA IS A SYMPTOM, NOT A DIAGNOSIS Martin RJ et al. Pathogenesis of apnea in preterm infants. J Pediatr. 1986; 109:733. APNEA IN THE NEONATE: DIFFERENTIAL Central Nervous System Respiratory • Intraventricular Hemorrhage • Airway Obstruction • Seizure • Inadequate Ventilation / Fatigue • Cerebral Infarct • Hypoxia Infection Gastrointestinal • Sepsis • Necrotizing Enterocolitis • Meningitis • Gastroesophageal Reflux Hematologic Drug Exposure • Anemia • Perinatal (Ex: Magnesium, Opioids) • Polycythemia • Postnatal (Ex: Sedatives, PGE) Cardiovascular Other • Patent Ductus Arteriosus • Temperature instability • Metabolic derangements APNEA IN THE NEONATE: EVALUATION ¢ Detailed History and Physical Examination ¢ Gestational age, post-natal age, and birth history ¢ Other new signs or symptoms ¢ Careful attention to neurologic, cardiorespiratory, and abdominal exam APNEA IN THE NEONATE: EVALUATION ¢ Laboratory Studies ¢ CBC/diff and CRP ¢ Cultures, consideration of LP ¢ Electrolytes including magnesium ¢ Blood gas and lactate ¢ Radiologic Studies ¢ Head ultrasound vs. -

Asphyxia Neonatorum
CLINICAL REVIEW Asphyxia Neonatorum Raul C. Banagale, MD, and Steven M. Donn, MD Ann Arbor, Michigan Various biochemical and structural changes affecting the newborn’s well being develop as a result of perinatal asphyxia. Central nervous system ab normalities are frequent complications with high mortality and morbidity. Cardiac compromise may lead to dysrhythmias and cardiogenic shock. Coagulopathy in the form of disseminated intravascular coagulation or mas sive pulmonary hemorrhage are potentially lethal complications. Necrotizing enterocolitis, acute renal failure, and endocrine problems affecting fluid elec trolyte balance are likely to occur. Even the adrenal glands and pancreas are vulnerable to perinatal oxygen deprivation. The best form of management appears to be anticipation, early identification, and prevention of potential obstetrical-neonatal problems. Every effort should be made to carry out ef fective resuscitation measures on the depressed infant at the time of delivery. erinatal asphyxia produces a wide diversity of in molecules brought into the alveoli inadequately com Pjury in the newborn. Severe birth asphyxia, evi pensate for the uptake by the blood, causing decreases denced by Apgar scores of three or less at one minute, in alveolar oxygen pressure (P02), arterial P02 (Pa02) develops not only in the preterm but also in the term and arterial oxygen saturation. Correspondingly, arte and post-term infant. The knowledge encompassing rial carbon dioxide pressure (PaC02) rises because the the causes, detection, diagnosis, and management of insufficient ventilation cannot expel the volume of the clinical entities resulting from perinatal oxygen carbon dioxide that is added to the alveoli by the pul deprivation has been further enriched by investigators monary capillary blood. -

Sleep Apnea Sleep Apnea
Health and Safety Guidelines 1 Sleep Apnea Sleep Apnea Normally while sleeping, air is moved at a regular rhythm through the throat and in and out the lungs. When someone has sleep apnea, air movement becomes decreased or stops altogether. Sleep apnea can affect long term health. Types of sleep apnea: 1. Obstructive sleep apnea (narrowing or closure of the throat during sleep) which is seen most commonly, and, 2. Central sleep apnea (the brain is causing a change in breathing control and rhythm) Obstructive sleep apnea (OSA) About 25% of all adults are at risk for sleep apnea of some degree. Men are more commonly affected than women. Other risk factors include: 1. Middle and older age 2. Being overweight 3. Having a small mouth and throat Down syndrome Because of soft tissue and skeletal alterations that lead to upper airway obstruction, people with Down syndrome have an increased risk of obstructive sleep apnea. Statistics show that obstructive sleep apnea occurs in at least 30 to 75% of people with Down syndrome, including those who are not obese. In over half of person’s with Down syndrome whose parents reported no sleep problems, sleep studies showed abnormal results. Sleep apnea causing lowered oxygen levels often contributes to mental impairment. How does obstructive sleep apnea occur? The throat is surrounded by muscles that are active controlling the airway during talking, swallowing and breathing. During sleep, these muscles are much less active. They can fall back into the throat, causing narrowing. In most people this doesn’t affect breathing. However in some the narrowing can cause snoring. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Potential Protective Mechanism of Arousal in Obstructive Sleep Apnea
Editorial Potential protective mechanism of arousal in obstructive sleep apnea Naomi Deacon, Atul Malhotra Department of Medicine, Pulmonary, Critical Care and Sleep Medicine, University of California San Diego, La Jolla, California, USA Correspondence to: Naomi Deacon, PhD. 9300 Campus Point Drive #7381, La Jolla, CA 92037-7381, USA. Email: [email protected]. Submitted Jul 01, 2016. Accepted for publication Jul 02, 2016. doi: 10.21037/jtd.2016.07.43 View this article at: http://dx.doi.org/10.21037/jtd.2016.07.43 Obstructive sleep apnea (OSA) pathophysiology is thought increase the magnitude of post-occlusion hyperventilation to be due to the interaction of traits including airway (and consequently hypocapnia) due both to arousal associated anatomy and neuromuscular control which vary between sympathetic activation and the state dependent differences individuals. These traits include a low arousal threshold in eupneic CO2 and sensitivity. This theory is based on (wake easily from sleep), upper airway gain (how effectively the founding work by Iber and colleagues in 1986 (7) activation of upper airway dilator muscles improves who studied tracheostomized OSA patients following ventilation), loop gain (stability of the negative feedback experimental tracheal occlusion during stable NREM sleep. chemoreflex control system) and upper airway collapsibility They found that tracheal occlusion yielded arousal and (anatomical predisposition to passive airway collapse) (1). pharyngeal opening which resulted in hyperventilation and While deficits in these traits and how they interact varies hypocapnia, followed by a reduction in minute ventilation between individuals, generally mechanisms that increase and prolongation of expiratory time. The magnitude of activation of upper airway dilator muscles are considered to hypocapnia correlated with expiratory prolongation and help protect the airway from collapse. -

Den170044 Summary
DE NOVO CLASSIFICATION REQUEST FOR CLEARMATE REGULATORY INFORMATION FDA identifies this generic type of device as: Isocapnic ventilation device. An isocapnic ventilation device is a prescription device used to administer a blend of carbon dioxide and oxygen gases to a patient to induce hyperventilation. This device may be labeled for use with breathing circuits made of reservoir bags (21 CFR 868.5320), oxygen cannulas (21 CFR 868.5340), masks (21 CFR 868.5550), valves (21 CFR 868.5870), resuscitation bags (21 CFR 868.5915), and/or tubing (21 CFR 868.5925). NEW REGULATION NUMBER: 21 CFR 868.5480 CLASSIFICATION: Class II PRODUCT CODE: QFB BACKGROUND DEVICE NAME: ClearMateTM SUBMISSION NUMBER: DEN170044 DATE OF DE NOVO: August 23, 2017 CONTACT: Thornhill Research, Inc. 5369 W. Wallace Ave Scottsdale, AZ 85254 INDICATIONS FOR USE ClearMateTM is intended to be used by emergency department medical professionals as an adjunctive treatment for patients suffering from carbon monoxide poisoning. The use of ClearMateTM enables accelerated elimination of carbon monoxide from the body by allowing isocapnic hyperventilation through simulated partial rebreathing. LIMITATIONS Intended Patient Population is adults aged greater than 16 years old and a minimum of 40 kg (80.8 lbs) ClearMateTM is intended to be used by emergency department medical professionals. This device should always be used as adjunctive therapy; not intended to replace existing protocol for treating carbon monoxide poisoning. When providing treatment to a non-spontaneously breathing patient using the ClearMate™ non-spontaneous breathing patient circuit, CO2 monitoring equipment for the measurement of expiratory carbon dioxide concentration must be used. PLEASE REFER TO THE LABELING FOR A MORE COMPLETE LIST OF WARNINGS AND CAUTIONS. -

BTS Guideline for Oxygen Use in Adults in Healthcare and Emergency
BTS guideline BTS guideline for oxygen use in adults in healthcare Thorax: first published as 10.1136/thoraxjnl-2016-209729 on 15 May 2017. Downloaded from and emergency settings BRO’Driscoll,1,2 L S Howard,3 J Earis,4 V Mak,5 on behalf of the British Thoracic Society Emergency Oxygen Guideline Group ▸ Additional material is EXECUTIVE SUMMARY OF THE GUIDELINE appropriate oxygen therapy can be started in the published online only. To view Philosophy of the guideline event of unexpected clinical deterioration with please visit the journal online ▸ (http://dx.doi.org/10.1136/ Oxygen is a treatment for hypoxaemia, not hypoxaemia and also to ensure that the oxim- thoraxjnl-2016-209729). breathlessness. Oxygen has not been proven to etry section of the early warning score (EWS) 1 have any consistent effect on the sensation of can be scored appropriately. Respiratory Medicine, Salford ▸ Royal Foundation NHS Trust, breathlessness in non-hypoxaemic patients. The target saturation should be written (or Salford, UK ▸ The essence of this guideline can be summarised ringed) on the drug chart or entered in an elec- 2Manchester Academic Health simply as a requirement for oxygen to be prescribed tronic prescribing system (guidance on figure 1 Sciences Centre (MAHSC), according to a target saturation range and for those (chart 1)). Manchester, UK 3Hammersmith Hospital, who administer oxygen therapy to monitor the Imperial College Healthcare patient and keep within the target saturation range. 3 Oxygen administration NHS Trust, London, UK ▸ The guideline recommends aiming to achieve ▸ Oxygen should be administered by staff who are 4 University of Liverpool, normal or near-normal oxygen saturation for all trained in oxygen administration. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Acute Respiratory Failure As the First Sign of Arnold-Chiari Malformation Associated with Syringomyelia
Eur Respir J, 1995, 8, 661–663 Copyright ERS Journals Ltd 1995 DOI: 10.1183/09031936.95.08040661 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 CASE REPORT Acute respiratory failure as the first sign of Arnold-Chiari malformation associated with syringomyelia D. Alvarez*, I. Requena**, M. Arias**, L. Valdés*, I. Pereiro+, R. De la Torre++ Acute respiratory failure as the first sign of Arnold-Chiari malformation associated with Services of *Pneumology, **Neurology, syringomyelia. D. Alvarez, I. Requena, M. Arias, L. Valdés, I. Pereiro, R. De la Torre. +Neuroimaging and ++Intensive Care, Hos- ERS Journals Ltd 1995. pital Provincial and Dept of Medicine of ABSTRACT: We report a rare case of acute respiratory failure in a previously the University of Santiago de Compostela, Santiago de Compostela, Spain. asymptomatic patient showing clinical signs of inferior cranial nerve palsy together with weakness and muscular atrophy of the upper limbs. Correspondence: D. Alvarez García, c) Magnetic resonance imaging revealed Arnold-Chiari malformation associated with Rosalía de Castro 57, 4º I., 15706 Santiago platybasia, basilar impression, syringomyelia and Klippel-Feil syndrome. Episodes de Compostela, Spain of apnoea required tracheostomy and recurred upon tentative closure of the tracheostome, but remitted upon decompression of the posterior fossa. Keywords: Adult respiratory distress, This case involved both obstructive mechanisms and dysfunction of the respiratory Arnold-Chiari malformation, sleep apnoea, centre. Patients with respiratory failure not explained by pulmonary pathology syringomyelia should be checked for underlying neurological disease. Received: October 29 1993 Eur Respir J., 1995, 8, 661–663. Accepted after revision September 13 1994 Arnold-Chiari malformation is a dysraphic congenital attempts at extubation were each followed by respiratory disorder, frequently associated with other malformations failure. -
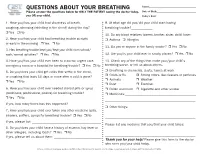
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7.