Common Causes of 'Swelling' in the Oral Cavity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Keratocystic Odontogenic Tumour Mimicking As a Dentigerous Cyst – a Rare Case Report Dr
DOI: 10.21276/sjds.2017.4.3.16 Scholars Journal of Dental Sciences (SJDS) ISSN 2394-496X (Online) Sch. J. Dent. Sci., 2017; 4(3):154-157 ISSN 2394-4951 (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Case Report Keratocystic Odontogenic Tumour Mimicking as a Dentigerous Cyst – A Rare Case Report Dr. K. Saraswathi Gopal1, Dr. B. Prakash vijayan2 1Professor and Head, Department of Oral Medicine and Radiology, Meenakshi Ammal Dental College and Hospital, Chennai 2PG Student, Department of Oral Medicine and Radiology, Meenakshi Ammal Dental College and Hospital, Chennai *Corresponding author Dr. B. Prakash vijayan Email: [email protected] Abstract: Keratocystic odontogenic tumor (KCOT) formerly known as odontogenic keratocyst (OKC), is considered a benign unicystic or multicystic intraosseous neoplasm and one of the most aggressive odontogenic lesions presenting relatively high recurrence rate and a tendency to invade adjacent tissue. On the other hand Dentigerous cyst (DC) is one of the most common odontogenic cysts of the jaws and rarely recurs. They were very similar in clinical and radiographic characteristics. In our case a pathological report following incisional biopsy turned out to be dentigerous cyst and later as Keratocystic odontogenic tumour following total excision. The treatment was chosen in order to prevent any pathological fracture. A recurrence was noticed after 2 months following which the lesion was surgically enucleated. At 2-years of follow-up, patient showed no recurrence. Keywords: Dentigerous cyst, Keratocystic odontogenic tumour (KCOT), Recurrence, Enucleation INTRODUCTION Keratocystic odontogenic tumour (KCOT) is a CASE REPORT rare developmental, epithelial and benign cyst of the A 17-year-old patient reported to the OP with a jaws of odontogenic origin with high recurrence rates. -

Jaw Lesions Associated with Impacted Tooth: a Radiographic Diagnostic Guide
Imaging Science in Dentistry 2016; 46: 147-57 http://dx.doi.org/10.5624/isd.2016.46.3.147 Jaw lesions associated with impacted tooth: A radiographic diagnostic guide Hamed Mortazavi1, Maryam Baharvand1,* 1Department of Oral Medicine, School of Dentistry, Shahid Beheshti University of Medical Sciences, Tehran, Iran ABSTRACT This review article aimed to introduce a category of jaw lesions associated with impacted tooth. General search engines and specialized databases such as Google Scholar, PubMed, PubMed Central, MedLine Plus, Science Direct, Scopus, and well-recognized textbooks were used to find relevant studies using keywords such as “jaw lesion”, “jaw disease”, “impacted tooth”, and “unerupted tooth”. More than 250 articles were found, of which approximately 80 were broadly relevant to the topic. We ultimately included 47 articles that were closely related to the topic of interest. When the relevant data were compiled, the following 10 lesions were identified as having a relationship with impacted tooth: dentigerous cysts, calcifying odontogenic cysts, unicystic (mural) ameloblastomas, ameloblastomas, ameloblastic fibromas, adenomatoid odontogenic tumors, keratocystic odontogenic tumors, calcifying epithelial odontogenic tumors, ameloblastic fibro-odontomas, and odontomas. When clinicians encounter a lesion associated with an impacted tooth, they should first consider these entities in the differential diagnosis. This will help dental practitioners make more accurate diagnoses and develop better treatment plans based on patients’ -

WHAT HAPPENED? CDR, a 24-Year-Old Chinese Male
CHILDHOOD DEVELOPMENTAL SCREENING 2020 https://doi.org/10.33591/sfp.46.5.up1 FINDING A MASS WITHIN THE ORAL CAVITY: WHAT ARE THE COMMON CAUSES AND 4-7 GAINING INSIGHT: WHAT ARE THE ISSUES? In Figure 2 below, a list of masses that could arise from each site Figure 3. Most common oral masses What are the common salivary gland pathologies Salivary gland tumours (Figure 7) commonly present as channel referrals to appropriate specialists who are better HOW SHOULD A GP MANAGE THEM? of the oral cavity is given and elaborated briey. Among the that a GP should be aware of? painless growing masses which are usually benign. ey can equipped in centres to accurately diagnose and treat these Mr Tan Tai Joum, Dr Marie Stella P Cruz CDR had a slow-growing mass in the oral cavity over one year more common oral masses are: torus palatinus, torus occur in both major and minor salivary glands but are most patients, which usually involves surgical excision. but sought treatment only when he experienced a sudden acute mandibularis, pyogenic granuloma, mucocele, broma, ere are three pairs of major salivary glands (parotid, commonly found occurring in the parotid glands. e most 3) Salivary gland pathology may be primary or secondary to submandibular and sublingual) as well as hundreds of minor ABSTRACT onset of severe pain and numbness. He was fortunate to have leukoplakia and squamous cell carcinoma – photographs of common type of salivary gland tumour is the pleomorphic systemic causes. ese dierent diseases may present with not sought treatment as it had not caused any pain. -
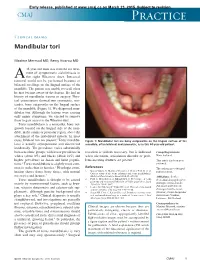
Mandibular Tori
Early release, published at www.cmaj.ca on March 23, 2015. Subject to revision. CMAJ Practice Clinical images Mandibular tori Maxime Mermod MD, Remy Hoarau MD 44-year-old man was referred for treat- ment of symptomatic sialolithiasis in A the right Wharton duct. Intraoral removal could not be performed because of bilateral swellings on the lingual surface of the mandible. The patient was unable to recall when he first became aware of the lesions. He had no history of mandibular trauma or surgery. Phys- ical examination showed two symmetric, non- tender, bony outgrowths on the lingual surface of the mandible (Figure 1). We diagnosed man- dibular tori. Although the lesions were causing only minor symptoms, we elected to remove them to gain access to the Wharton duct. Torus mandibularis is a nontender, bony out- growth located on the lingual side of the man- dible, in the canine or premolar region, above the attachment of the mylohyoid muscle. In most 1 cases, bilateral tori are present. Torus mandibu- Figure 1: Mandibular tori are bony outgrowths on the lingual surface of the laris is usually asymptomatic and discovered mandible, often bilateral and symmetric, as in this 44-year-old patient. incidentally. The prevalence varies substantially between ethnic groups, with lower prevalence in resection is seldom necessary, but is indicated Competing interests: whites (about 8%) and blacks (about 16%) and when ulceration, articulation disorder or prob- None declared. higher prevalence in Asian and Inuit popula- lems inserting dentures are present.3 This article has been peer tions.2 Torus mandibularis is slightly more com- reviewed. -

Evaluation of Bone Regeneration of Maxillary
EGYPTIAN Vol. 67, 1147:1156, April, 2021 DENTAL JOURNAL Print ISSN 0070-9484 • Online ISSN 2090-2360 Oral Surgery www.eda-egypt.org • Codex : 119/21.04 • DOI : 10.21608/edj.2021.65551.1533 EVALUATION OF BONE REGENERATION OF MAXILARY CYSTIC DEFECT GRAFTED WITH PUERARIN WITH CALCIUM SULPHATE GRANULES VERSUS CALCIUM SULPHATE AS A SOLOGRAFT: A RANDOMIZED CLINICAL TRIAL Saleh Ahmed Bakry* and Hesham Fattouh* ABSTRACT Aim: The aim of this study was to evaluate bone regeneration of maxillary cystic defect grafted with puerarin with calcium sulphate granules versus calcium sulphate granules as a solograft. Materials and Methods: This was a randomized controlled clinical trial conducted on 20 patients suffering from maxillary cystic lesions with size more than 3 cm2 indicated for enucleation without the need for resection or plate reconstruction. In the first group (A): Bony cavities were grafted by Puerarin mixed with hemihydrated calcium sulphate bone graft granules, while in the second group (B): The bony cavities were grafted by hemihydrated calcium sulphate bone graft granules only. All patients were followed up for 6 months recording the progress of the healing both clinically and radiographically via CBCT. Results: Surgeries went uneventful in patients of both groups. No notable complications occurred during the surgical procedures and the healing period of the two groups. Radiographic results after 6 months showed that there was a significant decrease in cyst volume in the purerein group compared to the other group. Conclusions: Puerarin is a promising graft material with probably an osteoinductive role, an issue that needs more researches to optimize its use and to understand its bone forming mechanism. -

Abscesses Apicectomy
BChD, Dip Odont. (Mondchir.) MBChB, MChD (Chir. Max.-Fac.-Med.) Univ. of Pretoria Co Reg: 2012/043819/21 Practice.no: 062 000 012 3323 ABSCESSES WHAT IS A TOOTH ABSCESS? A dental/tooth abscess is a localised acute infection at the base of a tooth, which requires immediate attention from your dentist. They are usually associated with acute pain, swelling and sometimes an unpleasant smell or taste in the mouth. More severe infections cause facial swelling as the bacteria spread to the nearby tissues of the face. This is a very serious condition. Once the swelling begins, it can spread rapidly. The pain is often made worse by drinking hot or cold fluids or biting on hard foods and may spread from the tooth to the ear or jaw on the same side. WHAT CAUSES AN ABSCESS? Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve. WHY CAN'T ANTIBIOTIC TREATMENT ALONE BE USED? Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. -

The Nutrition and Food Web Archive Medical Terminology Book
The Nutrition and Food Web Archive Medical Terminology Book www.nafwa. -

Radiology in the Diagnosis of Oral Pathology in Children Henry M
PEDIATRICDENTISTRY/Copyright © 1982 by AmericanAcademy of Pedodontics SpecialIssue/Radiology Conference Radiology in the diagnosis of oral pathology in children Henry M. Cherrick, DDS, MSD Introduction As additional information becomes available about that the possibility of caries or pulpal pathology the adverse effects of radiation, it is most important exists. that we review current practices in the use of radio- Pathological conditions excluding caries and pulpal graphs for diagnosis. It should be remembered that pathology, that do occur in the oral cavity in children the radiograph is only a diagnostic aid and rarely can can be classified under the following headings: a definitive diagnosis can be madewith this tool. Rou- 1. Congenital or developmental anomolies; 2. Cysts of tine dental radiographs are often taken as a screening the jaws; 3. Tumors of odontogenic origin; 4. Neo- procedure m frequently this tool is used to replace plasms occurring in bone; 5. Fibro-osseous lesions; 6. good physical examination techniques. A review of Trauma. procedures often employed in the practice of dentistry A good understanding of the clinical signs and reveals that a history is elicited from the patient (usu- symptoms, normal biological behavior, radiographic in- ally by an auxiliary) and then radiographs are taken terpretive data, and treatment of pathological condi- before a physical examination is completed. This tions which occur in the oral cavity will allow us to be sequence should be challenged inasmuch as most moreselective in the use of radiographs for diagnosis. pathologic conditions that occur in the facial bones It is not the purvue of this presentation to cover all present with clinical symptoms. -

Volving Periodontal Attachment, the Apposition of Fire Or Severe Trauma, Physical Features Are Often Cementum at the Root Apex, the Amount of Apical Destroyed
ISSN 0976-2256 E-ISSN: 2249-6653 The journal is indexed with ‘Indian Science Abstract’ (ISA) (Published by National Science Library), www.ebscohost.com, www.indianjournals.com JADCH is available (full text) online: Website- www.adc.org.in/html/viewJournal.php This journal is an official publication of Ahmedabad Dental College and Hospital, published bi-annually in the month of March and September. The journal is printed on ACID FREE paper. Editor - in - Chief Dr. Darshana Shah Co - Editor Dr. Rupal Vaidya DENTISTRY TODAY... Assistant Editor: We are living in an era in which community experience for Dr. Harsh Shah students is becoming a more essential component to the mission of dental education. Dental Public Health aims to improve the oral health of the population through preventive and curative services. The Editorial Board: introduction of mobile clinics into dentistry dates back to 1924. They have Dr. Mihir Shah been successfully used to provide dental treatment to schools, disabled patients, rural communities, industries and armed forces of various Dr. Vijay Bhaskar countries. Outreach programs using Mobile Dental Vans (MDV) are desirable model of clinical practice in a non-conventional setting, and help Dr. Monali Chalishazar the student to disassociate the image that best dentistry can only be Dr. A. R. Chaudhary practiced in conventional clinical settings. Confrontation with limited resources and economic barriers to Dr. Neha Vyas dental care for patients requiring more extensive procedures also serve as an additional learning experience in community-based programs. Unlike Dr. Sonali Mahadevia stationary dental clinics, mobile clinics provide greater physical access to dental care for medically underserved populations in poor urban and Dr. -

Cryotherapy in the Treatment of Glandular
Cryotherapy in the treatment of glandular odontogenic cyst: case report and review Crioterapia no tratamento de cisto odontogênico glandular: relato de caso e revisão Milene Borges Campagnaro* Raquel Medeiros Farias* Roger Correa de Barros Berthold** Márcia Rejane Brücker*** Fábio Dal Moro Maito**** Claiton Heitz***** Objective: The Glandular Odontogenic Cyst (GOC) is Introduction a rare benign odontogenic lesion, of considerable ag- gression, and often incorrectly diagnosed. We present a Glandular Odontogenic Cyst (GOC) was first patient with a Glandular Odontogenic Cyst in the pos- described by Gardner in 1988 as a distinct clinical terior mandible, its evolution, treatment, and follow-up. pathologic entity, and it was included in the WHO Case report: A female patient, 45 years old, was referred histological typing of odontogenic tumors under to the Oral and Maxillofacial Surgery and Traumatology GOC or sialo-odontogenic cyst1-5. Division at Cristo Redentor Hospital, Porto Alegre, Bra- Glandular Odontogenic Cyst is a rare lesion, of zil, for the assessment of a painful edema on the right considerable aggressive behavior, originated at the hemiface. A unilocular area with well-defined borders 1-5 in the retromolar region, posterior to the third molar on areas of dental support . Clinically, the most affec- the right side of the mandible. The histopathological ted site is the anterior part of the mandible and it examination suggested GOC. Final considerations: The mostly occurs in middle-aged patients with a slight Glandular Odontogenic Cyst needs a complete clinical male prevalence2,4-8. Epidemiological features are assessment associated with image analyses, and espe- scarce due to the rarity of the lesion and a review in cially, with histopathology for the correct diagnosis of 2008 pointed 111 cases published in the literature6. -

Glandular Odontogenic Cyst: Case Series and Summary of the Literature
502 > CLINICAL REVIEW http://dx.doi.org/10.17159/2519-0105/2019/v74no9a6 Glandular odontogenic cyst: case series and summary of the literature SADJ October 2019, Vol. 74 No. 9 p502 - p507 F Opondo1, S Shaik2, J Opperman3, CJ Nortjé4 ABSTRACT The glandular odontogenic cyst (GOC) remains a Histologically, it may mimic any one of a dentigerous rare entity. It was initially named “sialo-odontogenic cyst, radicular cyst, surgical ciliated cyst, lateral perio- cyst” by Padayachee and Van Wyk in 1987 when dontal cyst or a botryoid odontogenic cyst. Importantly, they reported the first two cases. Thereafter the the features of a cystic lesion with squamous and term glandular odontogenic cyst was suggested mucous epithelial elements may cause it to be mis- by Gardner et al. in 1988 and was subsequently diagnosed as a central mucoepidermoid carcinoma. adopted by the WHO.1 With more comprehensive diagnostic criteria, at least 180 In addition to its rarity, it has non-pathognomonic cases have so far been reported in the English literature.4 clinical and radiological features and hence can It is therefore reasonable to assume that the previous mimic other lesions. Since its recognition as an rarity of this entity may be attributable to misdiagnosis. entity by the WHO in 1992, only two further cases of glandular odontogenic cyst have been seen at CASE 1 the authors’ institution and are hereby reported together with a summary of the review articles in A 60-year-old man presented at the diagnostic clinic at the English literature. Tygerberg Oral Health Centre with an asymptomatic swelling of the anterior mandible.