Respiratory Syncytial Virus and African Americans
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

NMQF 2007 Leadership Summit Biographical Sketches
National Minority Quality Forum 2007 Leadership Summit Biographical Sketches Angel F. Avendano, MD Angel F. Avendano, MD, is a bilingual cardiologist with more than 20 years of clinical practice experience. He served as professor of medicine at Universidad Central de Venezuela. He cofounded and directed IDET, a main primary care institution in Venezuela. He has experience in clinical research since 1998 both international and in the United States. His work has been published. His research experience includes hypertension, hepatitis C, and HIV. His main research interests include the metabolic syndrome in HIV, lipid metabolic and cardiac risk factors in HIV, and hypertension. Jennifer Beaulieu (BIOGRAPHY NOT AVAILABLE.) Richard Beswick, PhD Richard Beswick, PhD, is associate medical director with Roche Laboratories Inc. Previously, Dr. Beswick served as manager of clinical affairs with Johnson and Johnson/Orthobiotech. During Dr. Beswick’s tenure with Orthobiotech, he was involved in new business development and clinical trial development. Born in Montego Bay, Jamaica, he earned a bachelor’s degree in biology from Morehouse College, Atlanta, GA, a master’s degree in cardiovascular physiology from Central Michigan University, Mount Pleasant; a master’s in business administration from Rollins College in Florida; and a PhD in molecular renal physiology from the University of Michigan School of Medicine. Dr. Beswick trained with Janice Douglas and Jackson Wright at Case Western Reserve University in the area of endocrinology and receptor kinetics with a focus on angiotensin receptor system in the kidneys of African American patients. Moreover, he has been involved in and has developed numerous protocols for academia and pharmaceutical industry. -
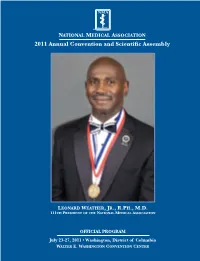
2011 Annual Convention and Scientific Assembly Table of Contents
11-0143 NMA ConvBk_Cvr 6/29/11 2:34 PM Page 1 N ATIONAL M EDICAL NATIONAL MEDICAL ASSOCIATION 2011 Annual Convention and Scientific Assembly A SSOCIATION 2011 Annual Convention and Scientific Assembly LEONARD WEATHER,JR., R.PH., M.D. 111TH PRESIDENT OF THE NATIONAL MEDICAL ASSOCIATION Washington, DC OFFICIAL PROGRAM July 23-27, 2011 • Washington, District of Columbia WALTER E. WASHINGTON CONVENTION CENTER 11-0143 NMA ConvBk_Cvr 6/29/11 2:34 PM Page 2 PLEASE JOIN US NEW ORLEANS, LOUISIANA July 28 - August 1, 2012 2012ANNUAL CONVENTION AND SCIENTIFIC ASSEMBLY National Medical Association 8403 Colesville Road, Suite 920 Silver Spring, MD 20910 202-347-1895 www.NMAnet.org July 23-27, 2011 Washington, DC Health Equity: Lead, Reform, Deliver OFFICIAL CONVENTION PROGRAM BOOK* NATIONAL MEDICAL ASSOCIATION 109TH ANNUAL CONVENTION AND SCIENTIFIC ASSEMBLY Walter E.Washington Convention Center Related additional information including needs assessment, disclosures, and speaker descriptions will be found in the individual session or section manuals. *This program is subject to change without prior notice. 8403 Colesville Road, Suite 920 Leonard Weather Jr., R.Ph., M.D. Silver Spring, Maryland 20910 President 202.347.1895 Ext. 211 • Fax 202.347.0722 www.NMAnet.org Dear Colleagues and Friends, I am pleased to welcome you to the National Medical Association’s (NMA) 109th Annual Convention and Scientific Assembly. The theme of this year’s meeting – “Health Equity: Lead, Reform, Deliver” references the vital leadership role that the NMA, and its members, must actively play in ensuring that healthcare reform is implemented in all states in a man- ner that results in improved health access, services, and outcomes for all especially our most vulnerable patients. -
Onsolidated R & D *Annual Project Report
/ RCC1.950804.003 REPORTS CONTROL SYMBOL CSCRO-16 ARMY MEDICAL SERVIC€ ONSOLIDATED R & D *ANNUAL PROJECT REPORT (EXCLUDING 0 M) Tlg I-TTOII COWAIlYOD -IN IS UWCLASBIFm EUT YAY NOT W mI&tQ)WITmIJT Tm expR688 PwYISsIrn dc n QIIOI, R#Ascdm AI0 DIVISION. -ICE CF TIP SuaOn m,DEPART- mtrQlmARyy. Whoa this document hr served its uur~oeeit my be di.Wlad of without reference to tha originating offiur. -. -. I JANUARY - 31 DECEMBER 1957 RESEARCH AND DEVELOPMENT DIVISION OFF!CE OF THE SURGEON GENERAL US ARMY pJm-yb-*?w?r. "-'-" .;~*:?q?.,~3.~ ' -1 . '* ,'.',. :)". I' AFXY MEDICAL SERVIm CONSOLIDATSD R & D ANNUAL PROJECT REPORT (Excluding GM) (Reports Control Symbol CSCRD-16) 1 January - 31 December 1957 The information contained herein is unclassified but may not be published 5.iithout the express permission of the Chief, Research and Development Division, Office of Tho Surgeon General, Department of the Amy. When this document has served its purpose it may be disposed of without reference to the originating office. Do not return this document. Research and Development Division Office of The Surgeon General u. s. Army .. _... - . .-..- - ... .--.. .- .. ,.. __ . - , TABU OF COIJTlEJTS Reports Control Symbol CSCRD-16 DIDEX OF PROJECTS 31 December 1957 CODE NO. PROJECT TITI;F: PROJECT NUIBEX PAGE 6.28 IIedical Wpment .I Developnent of Uedical, Dental 8 Veterinary 3qyipment & Supplies 1 7.23 IiIedical Sciences 4 ArnTy eosthetics Research Program 4 Ocular Research 6 X-ray & Photographic Techniques 8 Biological &Medical Aspects of 10 Ionizing Radiatim -

THE Double Helix Vol
THE DOUBLE HELIX Vol. 35, No. 4 | December 2010 Published by the National Foundation for Infectious Diseases NFID to Present Prestigious Awards at Upcoming Gala he National Foundation for result of Dr. Beasley’s findings vaccination Minister Tedros Adhanom Ghebreyesus Infectious Diseases (NFID) program around the world have prevented Dr. Tedros Adhanom Tannounces honorees for its 2011 untold numbers of deaths. Ghebreyesus has served Annual Awards Dinner on Tuesday, as Ethiopia’s Minister March 22, 2011 —Drs. R. Palmer Beasley Dr. Beasley conducted his remarkable of Health for the past and Tedros Adhanom Ghebreyesus. research career in Taiwan, as the director of five years. Under his the American Medical Research unit at the leadership the country NFID will present the Maxwell Finland U.S. Naval Research Unit in Taipei, where has embarked on an Award for Scientific Achievement to Dr. he and his colleagues studied and wrote effort to improve the Beasley for his distinguished scientific about hepatitis B. The studies led by Dr. health of Ethiopians career in preventive medicine and infectious Beasley were “incredible in terms of size and by addressing specific diseases. The Maxwell Finland Award is thoroughness,” stated Herbert L. DuPont, diseases such as malaria and HIV/AIDS presented to a scientist who has made out- MD, former NFID president and recipient and to improve the structure and capacity standing contributions to the understanding of the 2007 Maxwell Finland Award. for health services, with a special emphasis of infectious diseases or public health. on maternal care. Under Dr. Beasley’s leadership the Center Dr. Ghebreyesus will be honored with the for Infectious Disease at the University Dr. -
Bulletin of the College of William and Mary--Catalogue Issue, 1952-1953
College ot Willmm antr jHarp in Virginia Two Hundred and Sixtieth Year Williamsburg, Virginia 1952 - 1953 Bulletin of The College of William and Mary—Catalogue Issue Vol. 47, No. 6 April, 1953 Entered at the post office at Williamsburg, Virginia, July 3, 1926, under act of August 24, 1912, as second-class matter. Issued 10 times: Januar)', February, three issues in March, one issue in April, two issues in June, one issue in August, and one in December. "^ |£^-V •• my ^ •^- • •« - , * >Sgv^> ^''^^9^1% ^^A^^ • PRIORITIES • OF THE COLLEGE OF WILLIAM AND MARY. Charterf'd Febrnary 8,lBfl3.by Kiu^ William and One<»D Mary Maiu baildiog designod by Sir (hrisTopber Wen. First Collesje in the Uuiteri States m its antece- dents, which j?o hacK to the College propo?^ed at Heurico ( iGi 9 ). Second to Harvard University in actual operatioD. First American College to receive its charter from the Crown under the Seal of the Privy Coimctt. 1683. Hence it was known as their Majesties' Royal College of William and Mary." First and OMY American College to receive a Coat-ofArms from the College of Heralds,l694. First College in the United States to have a fnll Fac nlty. consisting of a President,six Professors, nsher. and writing master f229. First College to coiiler medallic prizesrthe ^old medals donated hy Lord Botetourt in iWl. First College to establish an inter collegiate fraternity, the Phi Beta Kappa. Ilec ember 5, 1'XIfG. First College to have the Elective System of stndy, 1773. First College to have the Honor Svstem,l'278. -

ACIP Meeting Minutes
DEPARTMENT OF HEALTH AND HUMAN SERVICES CENTERS FOR DISEASE CONTROL AND PREVENTION Advisory Committee on Immunization Practices February 21-22, 2007 Atlanta, Georgia Record of the Proceedings DEPARTMENT OF HEALTH AND HUMAN SERVICES CENTERS FOR DISEASE CONTROL AND PREVENTION ADVISORY COMMITTEE ON IMMUNIZATION PRACTICES February 21-22, 2007 Atlanta, Georgia C O N T E N T S February 21, 2007 WELCOME AND INTRODUCTION………………………………………………………..1 HEPATITIS A POSTEXPOSURE PROPHYLAXIS ………………………………………..2 Introduction: Dr. Bell........................... ……………………………………………....2 Study Results: Dr. Victor........................ …………………………………………….2 ROTAVIRUS VACCINE …………………………………………………………………...12 General Update: Dr. Parashar......................................................................................13 Disease Burden: Dr. Payne........................ ………………………………………….14 VAERS: Ms. Haber.....................................................................................................15 Data Interpretation: Dr. Patel................... …………………………………………...16 THIMEROSAL: REVIEWING THE EVIDENCE ………………………………………….21 Dr. Lieberman VACCINE SUPPLY………………………………………………………………………….28 Dr. Wallace INFLUENZA…………………………………………………………………………………32 Update: Dr. Allos..........................................................................................................33 Information: Dr. Fiore...................................................................................................34 Vote...............................................................................................................................43 -

U.S. Army Office of Medical History
Office of Medical History HOME FAQ CONTACTS LINKS MEDCOM SITEMAP ARMY.MIL AKO SEARCH ACCESS TO CARE Section 1 The Histories of the Commissions - Contents HISTORY OF THE OFFICE OF MEDICAL Commission on Acute Respiratory Diseases HISTORY ANC HISTORY Incorporating Three Other Commissions: Commission on Air-Borne Infections Commission on Meningococcal Meningitis Commission on Pneumonia AMEDD BIOGRAPHIES This history is dedicated with grateful appreciation to Drs. John H. Dingle and Colin M. AMEDD CORPS HISTORY MacLeod. Dingle's pioneering work was highly instrumental in ensuring success of the Commission on Acute Respiratory Diseases. MacLeod, his friend and associate, directed the BOOKS AND first Commission on Pneumonia and made lasting contributions not only to a number of DOCUMENTS commissions, but to the Armed Forces Epidemiological Board. It is not possible to measure the HISTORICAL ART impact of each of these two remarkable medical scientists in the whole field of preventive WORK & IMAGES medicine. MEDICAL MEMOIRS Foreword AMEDD MEDAL OF HONOR RECIPIENTS The annals of military preventive medicine provides a remarkable record of achievement ORGANIZATIONAL extending from Beaumont to Billings to Sternberg, Reed, Strong, Siler, Simmons, and so many HISTORIES more. Their work was a culmination of intelligent thought and scientific innovation all aimed at THE SURGEONS solving problems that arose from those social forces and political upheavals that involve GENERAL society as a whole. So often, there has been productive interaction between military and civilian scientists. Their combined opinions and collective funds of knowledge have helped ANNUAL REPORTS OF THE SURGEON determine just what should be done and how it might be accomplished, all with the aim to GENERAL better maintain the highest standards of health in military personnel. -

Full Text Article
SJIF Impact Factor: 5.464 WORLD JOURNAL OF ADVANCE ISSN: 2457-0400 Arpita et al. World Journal of Advance HealthcareVolume: Research 5. HEALTHCARE RESEARCH Issue: 2. Page N. 171-179 Year: 2021 Review Article www.wjahr.com NASAL PASSAGE IS THE COMMON ROUTE FOR RHINOVIRUS: A SILENT PATHOGENIC ALLERGEN READY TO HARM ANYTIME IS A CONTAGIOUS ONE *1Arpita Biswas, 1Amrita Chakraborty, 1Kushal Nandi, 1Saroni Saha, 1Dr. Dhrubo Jyoti Sen, 2Dr. Dhananjoy Saha, 3Dr. Kishor Dholwani and 4Dr. Pankaj H. Prajapati 1Department of Pharmaceutical Chemistry, School of Pharmacy, Techno India University, Salt Lake City, Sector–V, EM–4/1, Kolkata– 700091, West Bengal, India. 2Deputy Director, Directorate of Technical Education, Bikash Bhavan, Salt Lake City, Kolkata‒700091, West Bengal, India. 3Laxminarayandev College of Pharmacy, Narmada Nagar, Beside Swaminarayan School, Bharuch, Gujarat, India. 4Department of Pharmaceutics, Shri Sarvajanik Pharmacy College, Gujarat Technological University, Arvind Baug, Mehsana–384001, Gujarat, India. Received date: 25 January 2021 Revised date: 15 February 2021 Accepted date: 05 February 2021 *Corresponding author: Arpita Biswas Department of Pharmaceutical Chemistry, School of Pharmacy, Techno India University, Salt Lake City, Sector–V, EM–4/1, Kolkata– 700091, West Bengal, India. ABSTRACT The rhinovirus (from the Greek ῥίς rhis "nose", GEN ῥινός rhinos "of the nose", and the Latin virus) is the most common viral infectious agent in humans and is the predominant cause of the common cold. Rhinovirus infection proliferates in temperatures of 33–35°C (91–95°F), the temperatures found in the nose. Rhinoviruses belong to the genus Enterovirus in the family Picornaviridae. The three species of rhinovirus (A, B, and C) include around 160 recognized types of human rhinovirus that differ according to their surface proteins (serotypes). -

Annual Prevalence of HRV and Its Genotypes in Asia, Review
Journal of Entomology and Zoology Studies 2016; 4(5): 97-104 E-ISSN: 2320-7078 P-ISSN: 2349-6800 JEZS 2016; 4(5): 97-104 Annual prevalence of HRV and its genotypes in © 2016 JEZS Received: 15-07-2016 Asia, review Accepted: 16-08-2016 Sonia Aslam Sonia Aslam, Hameed Ur Rehman, Maryuem Humayun, Zakir Ullah, Department of Zoology, Saeed Ahmad, Muhammad Ayub Jadoon, Javid Khan, Mian Numan, Kohat University of Science and Technology, KPK, Pakistan. Muhammad Naeem and Kausar Saeed Hameed Ur Rehman Abstract Department of Chemistry, Human rhinovirus is the major pathogen among all age groups causing common cold and can be Kohat University of Science and Technology, KPK, Pakistan. associated with severe infections like asthma, pneumonia, wheezing which may lead to hospitalization. Phylogenetic analysis has led to the classification of human rhinovirus into three genotypes i-e HRV-A, Maryuem Humayun HRV-B and HRV-C. These genotypes have different biological properties, clinical outcome and provide Department of Microbiology, information for studying the epidemiology and pathogenesis. This review article characterizes the Abbottabad University of Science distribution of HRV and its genotypes for the first time in Asia. 94 published articles (2005-2015) related and Technology, Pakistan to HRV and its genotypes in Asia were searched. Children were more infected with HRV in Asia than in any other age group. HRV is the main agent causing acute respiratory infections in Asian countries, Zakir Ullah Department of Microbiology, responsible for mild to severe respiratory infections in all age groups, particularly in children. Effective Abbottabad University of Science preventive measures are needed on urgent basis to control the disease burden. -
VIRTUAL SYMPOSIUM and LECTURESHIP of the W
SUNDAY, JULY 18, 2021 18, JULY SUNDAY, 3:00–5:00 PM ET 2021 VIRTUAL SYMPOSIUM AND LECTURESHIP of the W. Montague Cobb/NMA Health Institute A CME PROGRAM TABLE OF CONTENTS Cobb Events at a Glance . 3 Scientific Planning Committee . 4 Disclosures of Commercial Relationships . 4 Accreditation Statement . 5 Letter from the Chief Executive Officer . 5 Statement of Credit and Purpose . 6 Learning Objectives . 7 Statement of Needs Assessment . 8 Agenda . 9 Award Recipients . 10 Speaker Biographies . 11 ABOUT THE COBB INSTITUTE The W. Montague Cobb/National Medical Association close partnership with Morehouse School of Medicine and (NMA) Health Institute (The Cobb Institute)—a 501(c)(3) the Association for Academic Minority Physicians (AAMP), in Washington, DC—engages in innovative research and the Institute also provides opportunities for early career knowledge dissemination for the reduction and elimination doctorates to receive intensive mentoring and networking of racial and ethnic health disparities. Founded in 2004, the in the areas of research, policy and practice. With funding Institute is named in honor of the late William Montague from governmental agencies such as the National Institutes Cobb M.D., Ph.D., LL.B., physician, anthropologist, of Health (NIH) as well as significant in-kind contributions, distinguished professor of medicine and anatomy at the the Institute continues to cultivateLogo a trusted and proven Howard University School of Medicine, and noted architect network of diverse stakeholders committed to solving of the National -

Bulletin of the College of William and Mary—Catalogue Issue
olfcCiC KJriJ;f } Bulletin of The College of William and Mary—Catalogue Issue Vol. 49, No. 6 April, 1955 Entered at the Post-Office at Williamsburg, Virginia, July 3, 1926, under act of August 24, 1912, as second-class matter. Issued 10 times: January, February, three issues in March, one issue in April, two issues in June, one issue in August, and one in December, //,' At pi y |— PP ^^1|te r- iviiit^ w '* • PRIORITIES ^ or THE COLLEGE OF WILLIAM AND MARY. Chartered Febrnary 8.i693.by King >^lliam and Qneeu Mar^c Main btrildin^ designod by Sir Cbri<fitopber Wen. First College in the UDitecl States in its antece- dents, which go back to the College proposed at Henrico ( iGi 9 ). Second to Harvard Univer'^ity in acttial operation. First American College to receive its charter from the Crown ander the Seal of the Privy Coimril. 1683. Hence it was known as their xMajesties' Royal College of William and Mary." First and ONLY American College to receive a Coat-ofArms from the College of Heralds. 1684. First College in the United States to have a foil Fac nlty, consisting of a President.six Professors. usher, and writing master. 1V29. First College to confer medallic prizes.the <|old medals donated hy Lord Botetourt in l"?*?!. First College to establish an intercollegiate fraternity, the Phi Beta Kappa. December 5. 1'Z'Ze. First College to have the nective System of study 1779. First College to have the Honor System,l7;?3. First College to become a University. IZPS. First College to have a school of Modern Lan^ua ges.17'29. -
RF Annual Report
The Rockefeller Foundation Annual Report, 1955 THE ROCKEFELLER JAM 2'< ZUul 'Y • XUvT. ^ vxX\^ 49 West 49th Street, New York 2003 The Rockefeller Foundation PRINTED IN THB UNITED STATES OF AMERICA 2003 The Rockefeller Foundation THE ROCKEFELLER FOUNDATION Trustees, Officers, and Staff 2003 The Rockefeller Foundation The Rockefeller Foundation TRUSTEES, OFFICERS, AND COMMITTEES April 19 55-April ig$6 TRUSTEES CHESTER BOWLES HENRY ALLEN MOE DETLEV W. BRONK WILLIAM I. MYERS RALPH J. BUNCHE THOMAS PARRAN WILLIAM H. CLAFLIN JOHN D. ROCKEFELLER, 3RD JOHN S. DICKEY DEAN RUSK LEWIS W, DOUGLAS GEOFFREY S. SMITH1 WALLACE K. HARRISON ROBERT G. SPROUL JOHN R. KIMBERLY ARTHUR HAYS SULZBERGER ROBERT F. LOEB HENRY P. VAN DUSEN ROBERT A. LOVETT W. BARRY WOOD, JR. JOHN J.MCCLOY EXECUTIVE COMMITTEE THE PRESIDENT, Chairman CHESTER BOWLES JOHN D. ROCKEFELLER, 3RD DETLEV W. BRONK W. BARRY WOOD, JR. ROBERT A. LOVETT RALPH J. BUNCHE, alternate member HENRY ALLEN MOE ROBERT F. LOEB, alternate member FINANCE COMMITTEE ROBERT A. LOVETT, Chairman WILLIAM H. CLAFLIN LEWIS w. DOUGLAS, alternate member JOHN J. MCCLOY GEOFFREY S. SMITH,1 alternate member THE PRESIDENT THE CHAIRMAN OF THE BOARD OF TRUSTEES 1 Resigned October 21, 1955. iv © 2003 The Rockefeller Foundation OFFICERS Chairman of the Board of Trustees JOHN D, ROCKEFELLER, SRD President DEAN RUSK Pice-President ALAN GREGG Executive Pice-President LINDSLEY p. KIM BALL Pice-President for the Natural and Medical Sciences WARREN WEAVER Secretary FLORA M. RHIND Treasurer EDWARD ROBINSON Comptroller H. MALCOLM GILLETTE Director for Agriculture j. GEORGE HARRAR Director for Biological and Medical Research ROBERT s. MORISON Director for the Humanities CHARLES B.