Report on Epidemiological Mapping of Schistosomiasis and Soil Transmitted Helminthiasis in 19 States and the FCT, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
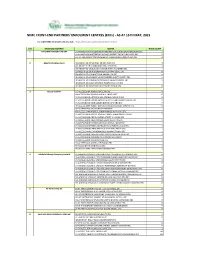
NIMC FRONT-END PARTNERS' ENROLMENT CENTRES (Ercs) - AS at 15TH MAY, 2021
NIMC FRONT-END PARTNERS' ENROLMENT CENTRES (ERCs) - AS AT 15TH MAY, 2021 For other NIMC enrolment centres, visit: https://nimc.gov.ng/nimc-enrolment-centres/ S/N FRONTEND PARTNER CENTER NODE COUNT 1 AA & MM MASTER FLAG ENT LA-AA AND MM MATSERFLAG AGBABIAKA STR ILOGBO EREMI BADAGRY ERC 1 LA-AA AND MM MATSERFLAG AGUMO MARKET OKOAFO BADAGRY ERC 0 OG-AA AND MM MATSERFLAG BAALE COMPOUND KOFEDOTI LGA ERC 0 2 Abuchi Ed.Ogbuju & Co AB-ABUCHI-ED ST MICHAEL RD ABA ABIA ERC 2 AN-ABUCHI-ED BUILDING MATERIAL OGIDI ERC 2 AN-ABUCHI-ED OGBUJU ZIK AVENUE AWKA ANAMBRA ERC 1 EB-ABUCHI-ED ENUGU BABAKALIKI EXP WAY ISIEKE ERC 0 EN-ABUCHI-ED UDUMA TOWN ANINRI LGA ERC 0 IM-ABUCHI-ED MBAKWE SQUARE ISIOKPO IDEATO NORTH ERC 1 IM-ABUCHI-ED UGBA AFOR OBOHIA RD AHIAZU MBAISE ERC 1 IM-ABUCHI-ED UGBA AMAIFEKE TOWN ORLU LGA ERC 1 IM-ABUCHI-ED UMUNEKE NGOR NGOR OKPALA ERC 0 3 Access Bank Plc DT-ACCESS BANK WARRI SAPELE RD ERC 0 EN-ACCESS BANK GARDEN AVENUE ENUGU ERC 0 FC-ACCESS BANK ADETOKUNBO ADEMOLA WUSE II ERC 0 FC-ACCESS BANK LADOKE AKINTOLA BOULEVARD GARKI II ABUJA ERC 1 FC-ACCESS BANK MOHAMMED BUHARI WAY CBD ERC 0 IM-ACCESS BANK WAAST AVENUE IKENEGBU LAYOUT OWERRI ERC 0 KD-ACCESS BANK KACHIA RD KADUNA ERC 1 KN-ACCESS BANK MURTALA MOHAMMED WAY KANO ERC 1 LA-ACCESS BANK ACCESS TOWERS PRINCE ALABA ONIRU STR ERC 1 LA-ACCESS BANK ADEOLA ODEKU STREET VI LAGOS ERC 1 LA-ACCESS BANK ADETOKUNBO ADEMOLA STR VI ERC 1 LA-ACCESS BANK IKOTUN JUNCTION IKOTUN LAGOS ERC 1 LA-ACCESS BANK ITIRE LAWANSON RD SURULERE LAGOS ERC 1 LA-ACCESS BANK LAGOS ABEOKUTA EXP WAY AGEGE ERC 1 LA-ACCESS -

Appraisal of Cowpea Cropping Systems and Farmers' Perceptions Of
Mohammed et al. CABI Agric Biosci (2021) 2:25 https://doi.org/10.1186/s43170-021-00046-7 CABI Agriculture and Bioscience RESEARCH Open Access Appraisal of cowpea cropping systems and farmers’ perceptions of production constraints and preferences in the dry savannah areas of Nigeria Saba Baba Mohammed1,2, Daniel Kwadjo Dzidzienyo2* , Muhammad Lawan Umar1, Mohammad Faguji Ishiyaku1, Pangirayi Bernard Tongoona2 and Vernon Gracen2,3 Abstract Background: Low plant density and wide intra-plant spacing in traditional cowpea cropping systems are among the factors responsible for low yield on farmers’ felds. Sole cropping and improved intercropping systems have been advocated in the last few years to increase yield in the dry savannah areas of Nigeria. This study investigated the level of adoption of high yielding cowpea cropping systems including factors that infuenced their use and farmers’ perceived production constraints and preferences. A total of 420 farmers across 36 villages of northern Nigeria were interviewed, and data collected was analyzed using descriptive statistics to appraise farmers predominant cowpea cropping systems and factors that determine the use of sole versus intercropping were identifed with the aid of binary logit regression. Furthermore, pairwise comparison ranking was deployed to understand farmers’ view of cow- pea production constraints and preferred traits. Results: The results revealed that, many of the farmers (42%) still grow cowpeas in the traditional intercropping and a good number (25%) cultivate the crop as a sole crop, while 23% had felds of cowpeas in both sole and intercropping systems. Farmers reported the incidence of high insect pests, limited access to land, desire to have multiple benefts, and assurance in the event of crop failure as reasons for preference for intercropping over sole planting. -

The Cholera Risk Assessment in Kano State, Nigeria: a Historical Review, Mapping of Hotspots and Evaluation of Contextual Factors
PLOS NEGLECTED TROPICAL DISEASES RESEARCH ARTICLE The cholera risk assessment in Kano State, Nigeria: A historical review, mapping of hotspots and evaluation of contextual factors 1 2 2 2 Moise Chi NgwaID *, Chikwe Ihekweazu , Tochi OkworID , Sebastian Yennan , 2 3 4 5 Nanpring Williams , Kelly ElimianID , Nura Yahaya Karaye , Imam Wada BelloID , David A. Sack1 1 Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States of America, 2 Nigeria Centre for Disease Control, Abuja, Nigeria, 3 Department of a1111111111 Microbiology, University of Benin, Nigeria, 4 Department of Public Health and Disease Control, Kano State a1111111111 Ministry of Health, Kano, Nigeria, 5 Department of Public Health and Disease Control, Ministry of Health a1111111111 Kano, Kano, Nigeria a1111111111 a1111111111 * [email protected] Abstract OPEN ACCESS Nigeria is endemic for cholera since 1970, and Kano State report outbreaks annually with Citation: Ngwa MC, Ihekweazu C, Okwor T, Yennan high case fatality ratios ranging from 4.98%/2010 to 5.10%/2018 over the last decade. How- S, Williams N, Elimian K, et al. (2021) The cholera ever, interventions focused on cholera prevention and control have been hampered by a risk assessment in Kano State, Nigeria: A historical lack of understanding of hotspot Local Government Areas (LGAs) that trigger and sustain review, mapping of hotspots and evaluation of contextual factors. PLoS Negl Trop Dis 15(1): yearly outbreaks. The goal of this study was to identify and categorize cholera hotspots in e0009046. https://doi.org/10.1371/journal. Kano State to inform a national plan for disease control and elimination in the State. -

Aquifers in the Sokoto Basin, Northwestern Nigeria, with a Description of the Genercl Hydrogeology of the Region
Aquifers in the Sokoto Basin, Northwestern Nigeria, With a Description of the Genercl Hydrogeology of the Region By HENRY R. ANDERSON and WILLIAM OGILBEE CONTRIBUTIONS TO THE HYDROLOGY OF AFRICA AND THE MEDITERRANEAN REGION GEOLOGICAL SURVEY WATER-SUPPLY PAPER 1757-L UNITED STATES GOVERNMENT PRINTING OFFICE, WASHINGTON : 1973 UNITED STATES DEPARTMENT OF THE INTERIOR ROGERS C. B. MORTON, Secretary GEOLOGICAL SURVEY V. E. McKelvey, Director Library of Congress catalog-card No. 73-600131 For sale by the Superintendent of Documents, U.S. Government Pri'ntinll Office Washinl\ton, D.C. 20402 - Price $6.75 Stock Number 2401-02389 CONTENTS Page Abstract -------------------------------------------------------- Ll Introduction -------------------------------------------------·--- 3 Purpose and scope of project ---------------------------------- 3 Location and extent of area ----------------------------------- 5 Previous investigations --------------------------------------- 5 Acknowledgments -------------------------------------------- 7 Geographic, climatic, and cultural features ------------------------ 8 Hydrology ----------------------_---------------------- __________ 10 Hydrogeology ---------------------------------------------------- 17 General features -------------------------------------------- 17 Physical character of rocks and occurrence of ground water ------- 18 Crystalline rocks (pre-Cretaceous) ------------------------ 18 Gundumi Formation (Lower Cretaceous) ------------------- 19 Illo Group (Cretaceous) ---------------------------------- -

LGA Agale Agwara Bida Borgu Bosso Chanchaga Edati Gbako Gurara
LGA Agale Agwara Bida Borgu Bosso Chanchaga Edati Gbako Gurara Katcha Kontagora Lapai Lavun Magama Mariga Mashegu Mokwa Munya Paikoro Rafi Rijau Shiroro Suleja Tafa Wushishi PVC PICKUP ADDRESS Santali Road, After Lga Secretariat, Agaie Opposite Police Station, Along Agwara-Borgu Road, Agwara Lga Umaru Magajib Ward, Yahayas, Dangana Way, Bida Lga Borgu Lga New Bussa, Niger Along Leg Road, Opp. Baband Abo Primary/Junior Secondary Schoo, Near Divisional Police Station, Maikunkele, Bosso Lga Along Niger State Houseso Assembly Quarters, Western Byepass, Minna Opposite Local Govt. Secretariat Road Edati Lga, Edati Along Bida-Zungeru Road, Gbako Lga, Lemu Gwadene Primary School, Gawu Babangida Gangiarea, Along Loga Secretariat, Katcha Katcha Lga Near Hamdala Motors, Along Kontagora-Yauri Road, Kontagoa Along Minna Road, Beside Pension Office, Lapai Opposite Plice Station, Along Bida-Mokwa Road, Lavun Off Lga Secretariat Road, Magama Lga, Nasko Unguwan Sarki, Opposite Central Mosque Bangi Adogu, Near Adogu Primary School, Mashegu Off Agric Road, Mokwa Lga Munya Lga, Sabon Bari Sarkin Pawa Along Old Abuja Road, Adjacent Uk Bello Primary School, Paikoro Behind Police Barracks, Along Lagos-Kaduna Road, Rafi Lga, Kagara Dirin-Daji/Tungan Magajiya Road, Junction, Rijau Anguwan Chika- Kuta, Near Lag Secretariat, Gussoroo Road, Kuta Along Suleja Minna Road, Opp. Suleman Barau Technical Collage, Kwamba Beside The Div. Off. Station, Along Kaduna-Abuja Express Road, Sabo-Wuse, Tafa Lga Women Centre, Behind Magistration Court, Along Lemu-Gida Road, Wushishi. Along Leg Road, Opp. Baband Abo Primary/Junior Secondary Schoo, Near Divisional Police Station, Maikunkele, Bosso Lga. -

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -
Nigeria Conflict Re-Interview (Emergency Response
This PDF generated by kmcgee, 8/18/2017 11:01:05 AM Sections: 11, Sub-sections: 0, Questionnaire created by akuffoamankwah, 8/2/2017 7:42:50 PM Questions: 130. Last modified by kmcgee, 8/18/2017 3:00:07 PM Questions with enabling conditions: 81 Questions with validation conditions: 14 Shared with: Rosters: 3 asharma (never edited) Variables: 0 asharma (never edited) menaalf (never edited) favour (never edited) l2nguyen (last edited 8/9/2017 8:12:28 PM) heidikaila (never edited) Nigeria Conflict Re- interview (Emergency Response Qx) [A] COVER No sub-sections, No rosters, Questions: 18, Static texts: 1. [1] DISPLACEMENT No sub-sections, No rosters, Questions: 6. [2] HOUSEHOLD ROSTER - BASIC INFORMATION No sub-sections, Rosters: 1, Questions: 14, Static texts: 1. [3] EDUCATION No sub-sections, Rosters: 1, Questions: 3. [4] MAIN INCOME SOURCE FOR HOUSEHOLD No sub-sections, No rosters, Questions: 14, Static texts: 1. [5] MAIN EMPLOYMENT OF HOUSEHOLD No sub-sections, No rosters, Questions: 6, Static texts: 1. [6] ASSETS No sub-sections, Rosters: 1, Questions: 12, Static texts: 1. [7] FOOD AND MARKET ACCESS No sub-sections, No rosters, Questions: 21. [8] VULNERABILITY MEASURE: COPING STRATEGIES INDEX No sub-sections, No rosters, Questions: 6. [9] WATER ACCESS AND QUALITY No sub-sections, No rosters, Questions: 22. [10] INTERVIEW RESULT No sub-sections, No rosters, Questions: 8, Static texts: 1. APPENDIX A — VALIDATION CONDITIONS AND MESSAGES APPENDIX B — OPTIONS LEGEND 1 / 24 [A] COVER Household ID (hhid) NUMERIC: INTEGER hhid SCOPE: IDENTIFYING -

Grain Price Seasonality in Kebbi State, Nigeria Patrick Hatzenbuehler, George Mavrotas, Mohammad Abubakar Maikasuwa, and Abdulrahaman Aliyu
STRATEGY SUPPORT PROGRAM | POLICY NOTE 47 | July 2018 Synopsis: Grain price seasonality in Kebbi state, Nigeria Patrick Hatzenbuehler, George Mavrotas, Mohammad Abubakar Maikasuwa, and Abdulrahaman Aliyu RESEARCH OVERVIEW will readjust that price back toward its prior level. Recent studies found the extent of food price Hence, trade stabilizes prices. seasonality in sub-Saharan Africa to be two to Likewise, storage, which allows supply in the three times greater than that observed on global current period to be carried over to the next, can markets. This implies that, despite decades of stabilize prices, but only under certain conditions. market liberalization in many countries, there Storage can reduce the probability of a steep price remains much progress to be made to improve decline because consumers and traders increase general food marketing conditions throughout purchases of grain to place into storage as prices Africa. This issue deserves research because the decline. Similarly, storage can also reduce the movements of prices during a crop year influence likelihood of price spikes, since traders and farmers the consumption decisions of households, the will sell their stored stocks when prices are rising – production decisions of farmers, and the marketing there is a lower likelihood of a steep rise in prices decisions of traders.1 if there are stocks in storage available to sell. A practical matter that emerges from these However, the ability to prevent price spikes is observations is what is the proper scale at which to conditional on the availability of stocks to sell and study the issue so that policy interventions can be the ability of traders and farmers to facilitate trade. -

Unmet Needs for Care and Support for the Elderly in Nigeria
Unmet Needs for Care and Support for the Elderly in Nigeria: Gaps in Experiences and Expectations of the Aged in Ilesa, South-West Nigeria DOI: 10.36108/NJSA/4102/12(0120) Akanni Ibukun Akinyemi 1 Ambrose Akinlo Department of Demography and Social Statistics Obafemi Awolowo University, Ile Ife, Nigeria 1Corresponding author: [email protected] Abstract The study is focused on understanding the broad issues of care and support of the elderly with a view to explaining factors influencing the gaps in their expectations and experiences. This is an empirical attempt with a view to understanding and under- scoring the importance and limitation of the domains of support from core family members (spouses and children) within the available support networks for the elderly. The study utilized primary dataset including quantitative and qualitative data collected in Ijesa communities in South-west, Nigeria. The findings showed that children and spouses ranked highest among sources of support networks rated by the elderly for five patterns of support identified. Logistic regression results showed that individual variables including age, education, family of orientation, and living in same town with children to a large extent determine level of unmet need for support. The study concluded that personal attributes rather than other social variables are important determinants of high level of unmet need for elderly. Keywords: unmet needs, care and support, elderly, Ilesa, Nigeria Introduction Increasing trend in the population of the aged or elderly has been a big challenge for many developed countries. Their prevailing high life expectancy and low total fertility rates, hovering around the replacement level of 2.1, have given rise to a population structure with a large proportion of the aged relative to the working population. -

Title the Minority Question in Ife Politics, 1946‒2014 Author(S
Title The Minority Question in Ife Politics, 1946‒2014 ADESOJI, Abimbola O.; HASSAN, Taofeek O.; Author(s) AROGUNDADE, Nurudeen O. Citation African Study Monographs (2017), 38(3): 147-171 Issue Date 2017-09 URL https://doi.org/10.14989/227071 Right Type Journal Article Textversion publisher Kyoto University African Study Monographs, 38 (3): 147–171, September 2017 147 THE MINORITY QUESTION IN IFE POLITICS, 1946–2014 Abimbola O. ADESOJI, Taofeek O. HASSAN, Nurudeen O. AROGUNDADE Department of History, Obafemi Awolowo University ABSTRACT The minority problem has been a major issue of interest at both the micro and national levels. Aside from the acclaimed Yoruba homogeneity and the notion of Ile-Ife as the cradle of Yoruba civilization, relationships between Ife indigenes and other communities in Ife Division (now in Osun State, Nigeria) have generated issues due to, and influenced by, politi- cal representation. Where allegations of marginalization have not been leveled, accommoda- tion has been based on extraneous considerations, similar to the ways in which outright exclu- sion and/or extermination have been put forward. Not only have suspicion, feelings of outright rejection, and subtle antagonism characterized majority–minority relations in Ife Division/ Administrative Zone, they have also produced political-cum-administrative and territorial ad- justments. As a microcosm of the Nigerian state, whose major challenge since attaining politi- cal independence has been the harmonization of interests among the various ethnic groups in the country, the Ife situation presents a peculiar example of the myths and realities of majority domination and minority resistance/response, or even a supposed minority attempt at domina- tion. -

Evaluation of Fungi Species from Commercial Yoghurts in Birnin
Equity Journal of Science and Technology, 2019 6(1): 72 -77 ISSN; 2354 – 1814 EQUIJOST An Official Publication of Kebbi State University of Science and Technology, Aliero, Nigeria Evaluation of Fungi Species from Commercial Yoghurts in Birnin Kebbi, Kebbi State Nigeria *1Keta, J.N., 2Suberu, H.A., 3Aliero, A.A., 4Mohammed, N.K., 1Anas, H., 1Mubarak, A. 1Department of Plant Sciences and Biotechnology, Kebbi State University of Science and Technology, Aliero, Nigeria 2Department of Biological Science, Federal University, Lokoja, Kogi State, Nigeria 3Department of Biological Science Federal University, Kalgo, Kebbi State, Nigeria 4Department of Microbiology, Kebbi State University of Science and Technology, Aliero *Corresponding author Email; [email protected]; Abstract Yoghurt is frequently taken as a drink or prepared together with Fura in the northern part of Nigeria due to the quality of nutrients present. Five different commercial Yoghurts, namely Hamdala, Rufaida, Gamji, Alhilal and Batulah were purchased from distributors in Birnin Kebbi metropolis. Using culture growth medium (Potato dextrose Agar) and poured plate method, the fungi species present were analyzed. A total of five (5) fungal species were isolated and identified from the samples. These include Aspergillus niger, Aspergillus fumigatus, Penicillium, Fusarium species and Mucor species. The results obtained from the samples analyzed showed that the Yoghurts samples had fungal load in the range of 1.2 x 105 (as the lowest fungal count in Gamji and Hamdala Yoghurts) and 8.0 x 106 (as the highest fungal count in Batula, Alhalal and Rufaida yoghurts). The highest levels of fungal species identified from this study could be attributed to poor processing method, environment, equipment used and preservation method adopted by these industries. -
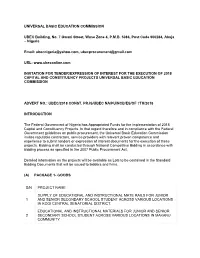
UNIVERSAL BASIC EDUCATION COMMISSION UBEC Building, No
UNIVERSAL BASIC EDUCATION COMMISSION UBEC Building, No. 7 Gwani Street, Wuse Zone 4, P.M.B. 5086, Post Code 900284, Abuja – Nigeria Email: [email protected], [email protected] URL: www.ubeconline.com INVITATION FOR TENDER/EXPRESSION OF INTEREST FOR THE EXECUTION OF 2018 CAPITAL AND CONSTITUENCY PROJECTS UNIVERSAL BASIC EDUCATION COMMISSION ADVERT NO.: UBEC/2018 CONST. PRJS/UBEC NA/PU/NCB/ES/OF 7TH/2018 INTRODUCTION The Federal Government of Nigeria has Appropriated Funds for the implementation of 2018 Capital and Constituency Projects. In that regard therefore and in compliance with the Federal Government guidelines on public procurement, the Universal Basic Education Commission invites reputable contractors, service providers with relevant proven competence and experience to submit tenders or expression of interest documents for the execution of these projects. Bidding shall be conducted through National Competitive Bidding in accordance with bidding process as specified in the 2007 Public Procurement Act. Detailed information on the projects will be available as Lots to be contained in the Standard Bidding Documents that will be issued to bidders and firms. (A) PACKAGE 1- GOODS S/N PROJECT NAME SUPPLY OF EDUCATIONAL AND INSTRUCTIONAL MATE RAILS FOR JUNIOR 1 AND SENIOR SECONDARY SCHOOL STUDENT ACROSS VARIOUS LOCATIONS IN KOGI CENTRAL SENATORIAL DISTRICT. EDUCATIONAL AND INSTRUCTIONAL MATERIALS FOR JUNIOR AND SENIOR 2 SECONDARY SCHOOL STUDENT ACROSS VARIOUS LOCATIONS IN MAKANU COMMUNITY PRINTING OF JOLLY PHONICS TEXTBOOKS (BOOK