Neuromuscular Blocking Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anaesthetic Experience with Paediatric Interventional Cardiology
320 Occasional Survey Anaesthetic experience with paediatric inter- Shobha Malviya MD, Frederick A. Burrows MD FRCPC, Albert E. Johnston MD FRCPC, Lee N. Benson MD FRCPC ventional cardiology Anaesthetic and sedation techniques, complications and out- In recent years interventional cardiologic procedures have comes were reviewed in 176 children undergoing 184 interven- replaced thoracic and cardiac surgery in the treatment of tional cardiologic procedures. Techniques included sedation certain cardiac anomalies in children. Balloon dilatation only, and ketamine, inhalational or narcotic anaesthesia. is particularly effective in treating pulmonary valve Ketamine infusion was the technique most frequently used. stenosis and is also performed as a nonsurgical alternative Ketamine was associated with a higher incidence of respiratory for patients with aortic valve stenosis, recoaretation of the complications (P < 0.05) than the other techniques. The higher aorta and pulmonary artery stenosis. Insertion of an incidence of hypercarbia (15.6 per cent), which did not affect occlusion device is used to treat patent ductus arteriosus. outcome, may be attributable to the use of supplemental Procedures performed in the cardiac catheterisation sedatives. The incidence of upper airway obstruction (7.8 per suite require a darkened room, allow poor access to the cenO was similar to that of previous studies. Vascular compro- often critically ill patient and present the potential for mise resulted from the procedure in 33 patients, necessitating sudden devastating complications, including rupture of a surgical correction in 16. Cardiac perforation occurred in four cardiac chamber. In addition, interventional procedures cases, causing one death. Pulmonary valve stenosis was most require a steady haemodynamic state before oxygen amenable to balloon dilatation and aortic valve stenosis least saturation and pressures in the various cardiac chambers amenable. -

Comparative Study of Different Doses of Rocuronium Bromide For
MedDocs Publishers Annals of Anesthesia and Pain Medicine Open Access | Research Article Comparative study of different doses of rocuronium bromide for endotracheal intubation Nidhi V Sardhara1*; Sonal A Shah2; Dhaval P Pipaliya3; Shivansh Gupta3 1SVP hospital, 13th floor, Room no 13125, Near Ellis bridge, Ahmedabad, Gujarat-380006 2Assistant Professor, Department of anesthesia, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India 3First year Resident, Department of anesthesia, Smt. NHL Municipal Medical College, Ahmedabad, Gujarat, India *Corresponding Author(s): Nidhi V Sardhara Abstract SVP hospital, 13th floor, Room no 13125, Near Ellis Background: Endotracheal intubation is one of such bridge, Ahmedabad, Gujarat-380006 development without which general anesthesia cannot be Tel: +91-9428-44-7878, Fax: 7926-57-8452 considered safe for any major surgery particularly head and Email: [email protected] neck, thoracic and abdominal surgeries. Ever since the ad- vent of anesthesia, anesthesiologists have been in search of an ideal muscle relaxants which can provide ideal intu- bating conditions in ultrashort duration with minimal side effects. Rocuronium bromide provides fast onset of action, Received: Mar 11, 2020 an intermediate duration of action and rapid recovery, good Accepted: Apr 24, 2020 to excellent intubating conditions at doses having minimal Published Online: Apr 30, 2020 or no haemodynamic changes. Present study is to compare the effect of different doses (0.6 mg/kg, 0.9 mg/kg, 1.2 mg/ Journal: Annals of Anesthesia and Pain Medicine kg) of Rocuronium bromide for endotracheal intubation at Publisher: MedDocs Publishers LLC 60 seconds. Online edition: http://meddocsonline.org/ Material and methods: This study was carried out by Copyright: © Sardhara NV (2020). -

Product Monograph Vecuronium Bromide For
PRODUCT MONOGRAPH PrVECURONIUM BROMIDE FOR INJECTION Non-depolarizing Skeletal Neuromuscular Blocking Agent Pharmaceutical Partners of Canada Inc. Date of Preparation: 45 Vogell Road, Suite 200 January 15, 2008 Richmond Hill, ON L4B 3P6 Control No.: 119276 PRODUCT MONOGRAPH PrVECURONIUM BROMIDE FOR INJECTION Non-depolarizing Skeletal Neuromuscular Blocking Agent THIS DRUG SHOULD BE ADMINISTERED ONLY BY ADEQUATELY TRAINED INDIVIDUALS FAMILIAR WITH ITS ACTIONS, CHARACTERISTICS AND HAZARDS ACTIONS AND CLINICAL PHARMACOLOGY Vecuronium Bromide for Injection is a non-depolarizing neuromuscular blocking agent of intermediate duration possessing all of the characteristic pharmacological actions of this class of drugs (curariform). It acts by competing for cholinergic receptors at the motor end-plate. The antagonism to acetylcholine is inhibited and neuromuscular block reversed by acetylcholinesterase inhibitors such as neostigmine. Vecuronium Bromide for Injection is about 1/3 more potent than pancuronium; the duration of neuromuscular blockade produced by Vecuronium Bromide for Injection is shorter than that of pancuronium at initially equipotent doses. The time to onset of paralysis decreases and the duration of maximum effect increases with increasing Vecuronium Bromide for Injection doses. The use of a peripheral nerve stimulator is of benefit in assessing the degree of muscular relaxation. The ED90 (dose required to produce 90% suppression of the muscle twitch response with balanced anesthesia) has averaged 0.057 mg/kg (0.049 to 0.062 mg/kg in various studies). An initial Vecuronium Bromide for Injection dose of 0.08 to 0.10 mg/kg generally produces first depression of twitch in approximately 1 minute, good or excellent intubation conditions within 2.5 to 3 minutes, and maximum neuromuscular blockade within 3 to 5 minutes of injection in Vecuronium Bromide for Injection, Product Monograph Page 2 of 28 most patients. -

The Quest for the Origin and Prevention of Postoperative Myalgia Following Succinylcholine : New Insights in an Old Problem
The quest for the origin and prevention of postoperative myalgia following succinylcholine : new insights in an old problem Citation for published version (APA): Schreiber, J-U. (2010). The quest for the origin and prevention of postoperative myalgia following succinylcholine : new insights in an old problem. Datawyse / Universitaire Pers Maastricht. https://doi.org/10.26481/dis.20100702js Document status and date: Published: 01/01/2010 DOI: 10.26481/dis.20100702js Document Version: Publisher's PDF, also known as Version of record Please check the document version of this publication: • A submitted manuscript is the version of the article upon submission and before peer-review. There can be important differences between the submitted version and the official published version of record. People interested in the research are advised to contact the author for the final version of the publication, or visit the DOI to the publisher's website. • The final author version and the galley proof are versions of the publication after peer review. • The final published version features the final layout of the paper including the volume, issue and page numbers. Link to publication General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal. -

Vecuronium Bromide As Control
A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL. Dissertation submitted In partial fulfillment for the award of M.D DEGREE EXAMINATION M.D. ANAESTHESIOLOGY & CRITICAL CARE BRANCH X GOVT KILPAUK MEDICAL COLLEGE AND HOSPITAL SUBMITTED TO THE TAMILNADU DR. MGR MEDICAL UNIVERSITY CHENNAI APRIL – 2011 1 DECLARATION I, Dr. D.Shunmuga Priya, solemnly declare that the dissertation, “A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL” is a bonafide work done by me in the Department of Anaesthesiology and Critical Care, Government Kilpauk, Medical College, Chennai under the able guidance of Prof. Dr. P.S. Shanmugam, MD., DA., Professor and HOD, Department of Anaesthesiology and Critical Care, Government Kilpauk Medical College, Chennai. Place : Chennai Date : (Dr. D.SHUNMUGA PRIYA) 5 CERTIFICATE This is to certify that this dissertation titled “A COMPARATIVE STUDY TO FIND AN IDEAL INTUBATING DOSE OF INJ. ROCURONIUM BROMIDE USING INJ. VECURONIUM BROMIDE AS CONTROL” has been prepared by Dr. D.SHUNMUGA PRIYA under my supervision in the Department of Anaesthesiology and Critical Care, Government Kilpauk Medical College, Chennai during the academic period 2008-2011 and is being submitted to the Tamil Nadu Dr. M.G.R. Medical University, Chennai in partial fulfillment of the University regulation for the award of the Degree of Doctor of Medicine (MD Anaesthesiology and Critical Care) and her dissertation is a bonafide work. Prof..Dr. V.Kanagasabai, M.D Prof. Dr. P.S.Shanmugam, M.D., D.A. DEAN Professor & HOD, Government Kilpauk Medical College Department of Anaesthesiology and & Hospital, Critical Care, Chennai. -

BRS Pharmacology
Pharmacology Gary C. Rosenfeld, Ph.D. Professor Department of Integrated Biology and Pharmacology and Graduate School of Biomedical Sciences Assistant Dean for Education Programs University of Texas Medical School at Houston Houston, Texas David S. Loose, Ph.D. Associate Professor Department of Integrated Biology and Pharmacology and Graduate School of Biomedical Sciences University of Texas Medical School at Houston Houston, Texas With special contributions by Medina Kushen, M.D. William Beaumont Hospital Royal Oak, Michigan Todd A. Swanson, M.D., Ph.D. William Beaumont Hospital Royal Oak, Michigan Acquisitions Editor: Charles W. Mitchell Product Manager: Stacey L. Sebring Marketing Manager: Jennifer Kuklinski Production Editor: Paula Williams Copyright C 2010 Lippincott Williams & Wilkins 351 West Camden Street Baltimore, Maryland 21201-2436 USA 530 Walnut Street Philadelphia, PA 19106 All rights reserved. This book is protected by copyright. No part of this book may be reproduced in any form or by any means, including photocopying, or utilized by any information storage and retrieval system without written permission from the copyright owner. The publisher is not responsible (as a matter of product liability, negligence or otherwise) for any injury resulting from any material contained herein. This publication contains information relating to general principles of medical care which should not be construed as specific instructions for individual patients. Manufacturers’ product information and package inserts should be reviewed for current information, including contraindications, dosages and precautions. Printed in the United States of America Library of Congress Cataloging-in-Publication Data Rosenfeld, Gary C. Pharmacology / Gary C. Rosenfeld, David S. Loose ; with special contributions by Medina Kushen, Todd A. -

Doxacurium Chloride Injection Abbott Laboratories
NUROMAX - doxacurium chloride injection Abbott Laboratories ---------- NUROMAX® (doxacurium chloride) Injection This drug should be administered only by adequately trained individuals familiar with its actions, characteristics, and hazards. NOT FOR USE IN NEONATES CONTAINS BENZYL ALCOHOL DESCRIPTION NUROMAX (doxacurium chloride) is a long-acting, nondepolarizing skeletal muscle relaxant for intravenous administration. Doxacurium chloride is [1α,2β(1'S*,2'R*)]-2,2' -[(1,4-dioxo-1,4- butanediyl)bis(oxy-3,1-propanediyl)]bis[1,2,3,4-tetrahydro-6,7,8-trimethoxy-2- methyl-1-[(3,4,5- trimethoxyphenyl)methyl]isoquinolinium] dichloride (meso form). The molecular formula is C56H78CI2N2O16 and the molecular weight is 1106.14. The compound does not partition into the 1- octanol phase of a distilled water/ 1-octanol system, i.e., the n-octanol:water partition coefficient is 0. Doxacurium chloride is a mixture of three trans, trans stereoisomers, a dl pair [(1R,1'R ,2S,2'S ) and (1S,1'S ,2R,2'R )] and a meso form (1R,1'S,2S,2'R). The meso form is illustrated below: NUROMAX Injection is a sterile, nonpyrogenic aqueous solution (pH 3.9 to 5.0) containing doxacurium chloride equivalent to 1 mg/mL doxacurium in Water for Injection. Hydrochloric acid may have been added to adjust pH. NUROMAX Injection contains 0.9% w/v benzyl alcohol. Reference ID: 2867706 CLINICAL PHARMACOLOGY NUROMAX binds competitively to cholinergic receptors on the motor end-plate to antagonize the action of acetylcholine, resulting in a block of neuromuscular transmission. This action is antagonized by acetylcholinesterase inhibitors, such as neostigmine. Pharmacodynamics NUROMAX is approximately 2.5 to 3 times more potent than pancuronium and 10 to 12 times more potent than metocurine. -
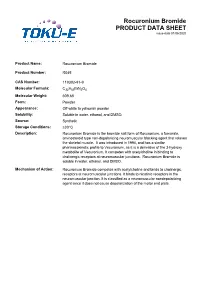
Rocuronium Bromide PRODUCT DATA SHEET Issue Date 01/06/2020
Rocuronium Bromide PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Rocuronium Bromide Product Number: R045 CAS Number: 119302-91-9 Molecular Formula: C32H53BrN2O4 Molecular Weight: 609.68 Form: Powder Appearance: Off-white to yellowish powder Solubility: Soluble in water, ethanol, and DMSO. Source: Synthetic Storage Conditions: ≤30°C Description: Rocuronium Bromide is the bromide salt form of Rocuronium, a fumarate, aminosteroid type non-depolarizing neuromuscular blocking agent that relaxes the skeletal muscle. It was introduced in 1994, and has a similar pharmacokinetic profile to Vecuronium, as it is a derivative of the 3-hydroxy metabolite of Vecuronium. It competes with acetylcholine in binding to cholinergic receptors at neuromuscular junctions. Rocuronium Bromide is soluble in water, ethanol, and DMSO. Mechanism of Action: Rocuronium Bromide competes with acetylcholine and binds to cholinergic receptors at neuromuscular junctions. It binds to nicotinic receptors in the neuromuscular junction. It is classified as a neuromuscular nondepolarizing agent since it does not cause depolarization of the motor end plate. References: Anzenbacherova et al (2015) Interaction of Rocuronium with human liver cytochromes P450. J. Pharmacol. Sci. 127(2):190-195 PMID 25727956 Cembala TM, Sherwin JD, Tidmarsh MD, Appadu BL and Lambert DG (1998) Interaction of neuromuscular blocking drugs with recombinant human m1-m5 muscarinic receptors expressed in Chinese hamster ovary cells. B. J. Pharmacol. 125(5):1088-1094 PMID 9846649 Koksal PM and Gürbüzel M(2015) Analysis of genotoxic activity of ketamine and Rocuronium Bromide using the somatic mutation and recombination test in Drosophila melanogaster. Environ Toxicol Pharmacol. 39(2):628-634 PMID 25682000 Sauer et al (2017) Rocuronium is more hepatotoxic than succinylcholine in vitro. -

Case Report Carbamazepine Toxicity Following Oxybutynin And
Spinal Cord (2005) 43, 252–255 & 2005 International Spinal Cord Society All rights reserved 1362-4393/05 $30.00 www.nature.com/sc Case Report Carbamazepine toxicity following Oxybutynin and Dantrolene administration: a case report T Vander*,1, H Odi1, V Bluvstein1, J Ronen1,2 and A Catz1,2 1Department of Spinal Rehabilitation, Loewenstein Rehabilitation Hospital, Raanana, Israel; 2Tel-Aviv University, Tel-Aviv, Israel Objective: To report a case of Carbamazepine toxicity following the administration of Oxybutynin and Dantrolene. Study design: A case report. Setting: The Spinal Rehabilitation Department, Loewenstein Hospital, Raanana, Israel. Methods: A patient with C6D tetraplegia who sustained intoxication because of drug interaction is presented. She had been treated by Carbamazepine 1000 mg/day for neuropathic pain for 2 years without clinical or laboratory signs of toxicity. After administration of Oxybutynin concomitantly with an increase in the dose of Dantrolene, she presented the clinical symptoms and laboratory finding of Carbamazepine intoxication. Trying to adjust the treatment to the patient’s requirements, Carbamazepine together with Oxybutynin and Dantrolene was readministrated in lower doses. Results: The combination of these drugs, even small doses, caused toxicity. Adding Dantrolene and Oxybutynin elevated the blood level of Carbamazepine, possibly by inhibition of cytochrome P450. Conclusion: A possible pharmacokinetic interaction between Dantrolene and Oxybutynin should be borne in mind when considering Carbamazepine medication for a patient with a spinal cord lesion. Spinal Cord (2005) 43, 252–255. doi:10.1038/sj.sc.3101689; Published online 1 February 2005 Keywords: Carbamazepine; Oxybutynin; Dantrolene; drug interaction; cytochrome P450 Introduction Both Oxybutynin chloride and Dantrolene sodium are be required when patients have concomitant post- widely used in patients with spinal cord lesion (SCL). -

COMPARISON of ROCURONIUM BROMIDE and SUCCINYLCHOLINE CHLORIDE for USE DURING RAPID SEQUENCE INTUBATION in ADULTS Ch
DOI: 10.18410/jebmh/2015/672 ORIGINAL ARTICLE COMPARISON OF ROCURONIUM BROMIDE AND SUCCINYLCHOLINE CHLORIDE FOR USE DURING RAPID SEQUENCE INTUBATION IN ADULTS Ch. Penchalaiah1, N. Jagadeesh Babu2, T. Kumar3 HOW TO CITE THIS ARTICLE: Ch. Penchalaiah, N. Jagadeesh Babu, T. Kumar. ”Comparison of Rocuronium Bromide and Succinylcholine Chloride for Use during Rapid Sequence Intubation in Adults”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 32, August 10, 2015; Page: 4796-4806, DOI: 10.18410/jebmh/2015/672 ABSTRACT: BACKGROUND AND OBJECTIVE: The goal of rapid sequence intubation is to secure the patients airway smoothly and quickly, minimizing the chances of regurgitation and aspiration of gastric contents. Traditionally succinylcholine chloride has been the neuromuscular blocking drug of choice for use in rapid sequence intubation because of its rapid onset of action and profound relaxation. Succinylcholine chloride remains unsurpassed in providing ideal intubating conditions. However the use of succinylcholine chloride is associated with many side effects like muscle pain, bradycardia, hyperkalaemia and rise in intragastric and intraocular pressure. Rocuronium bromide is the only drug currently available which has the rapidity of onset of action like succinylcholine chloride. Hence the present study was undertaken to compare rocuronium bromide with succinylcholine chloride for use during rapid sequence intubation in adult patients. METHODOLOGY: The study population consisted of 90 patients aged between 18-60 years posted for various elective surgeries requiring general anaesthesia. Study population was randomly divided into 3 groups with 30 patients in each sub group. 1. Group I: Intubated with 1 mg kg-1 of succinylcholine chloride (n=30). -

Skeletal Muscle Relaxants Review 12/17/2008
Skeletal Muscle Relaxants Review 12/17/2008 Copyright © 2007 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to -

Drug Class Review on Skeletal Muscle Relaxants
Drug Class Review on Skeletal Muscle Relaxants Final Report Update 2 May 2005 Original Report Date: April 2003 Update 1 Report Date: January 2004 A literature scan of this topic is done periodically The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Roger Chou, MD Kim Peterson, MS Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, MD, MPH, Director Copyright © 2005 by Oregon Health & Science University Portland, Oregon 97201. All rights reserved. Note: A scan of the medical literature relating to the topic is done periodically (see http://www.ohsu.edu/ohsuedu/research/policycenter/DERP/about/methods.cfm for scanning process description). Upon review of the last scan, the Drug Effectiveness Review Project governance group elected not to proceed with another full update of this report. Some portions of the report may not be up to date. Prior versions of this report can be accessed at the DERP website. Final Report Update 2 Drug Effectiveness Review Project TABLE OF CONTENTS Introduction........................................................................................................................4 Scope and