6.7.1 Acute Problems Questions and Answers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Management of Peri-Implant Mucositis and Peri-Implantitis Elena Figuero1, Filippo Graziani2, Ignacio Sanz1, David Herrera1,3, Mariano Sanz1,3
PERIODONTOLOGY 2000 Management of peri-implant mucositis and peri-implantitis Elena Figuero1, Filippo Graziani2, Ignacio Sanz1, David Herrera1,3, Mariano Sanz1,3 1. Section of Graduate Periodontology, University Complutense, Madrid, Spain. 2. Department of Surgery, Unit of Dentistry and Oral Surgery, University of Pisa 3. ETEP (Etiology and THerapy of Periodontal Diseases) ResearcH Group, University Complutense, Madrid, Spain. Corresponding author: Elena Figuero Running title: Management of peri-implant diseases Key words: Peri-implant Mucositis, Peri-implantitis, Peri-implant Diseases, Treatment Title series: Implant surgery – 40 years experience Editors: M. Quirynen, David Herrera, Wim TeugHels & Mariano Sanz 1 ABSTRACT Peri-implant diseases are defined as inflammatory lesions of the surrounding peri-implant tissues, and they include peri-implant mucositis (inflammatory lesion limited to the surrounding mucosa of an implant) and peri-implantitis (inflammatory lesion of the mucosa, affecting the supporting bone with resulting loss of osseointegration). This review aims to describe the different approacHes to manage both entities and to critically evaluate the available evidence on their efficacy. THerapy of peri-implant mucositis and non-surgical therapy of peri-implantitis usually involve the mecHanical debridement of the implant surface by means of curettes, ultrasonic devices, air-abrasive devices or lasers, with or without the adjunctive use of local antibiotics or antiseptics. THe efficacy of these therapies Has been demonstrated for mucositis. Controlled clinical trials sHow an improvement in clinical parameters, especially in bleeding on probing. For peri-implantitis, the results are limited, especially in terms of probing pocket depth reduction. Surgical therapy of peri-implantitis is indicated wHen non-surgical therapy fails to control the inflammatory cHanges. -

Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report Abstract Hereditary gingival fibromatosis (HGF) is a rare condition characterized by varying degrees of gingival hyperplasia. Gingival fibromatosis usually occurs as an isolated disorder or can be associated with a variety of other syndromes. A 33-year-old male patient who had a generalized severe gingival overgrowth covering two thirds of almost all maxillary and mandibular teeth is reported. A mucoperiosteal flap was performed using interdental and crevicular incisions to remove excess gingival tissues and an internal bevel incision to reflect flaps. The patient was treated 15 years ago in the same clinical facility using the same treatment strategy. There was no recurrence one year following the most recent surgery. Keywords: Gingival hyperplasia, hereditary gingival hyperplasia, HGF, hereditary disease, therapy, mucoperiostal flap Citation: S¸engün D, Hatipog˘lu H, Hatipog˘lu MG. Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report. J Contemp Dent Pract 2007 January;(8)1:090-096. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 8, No. 1, January 1, 2007 Introduction Hereditary gingival fibromatosis (HGF), also Ankara, Turkey with a complaint of recurrent known as elephantiasis gingiva, hereditary generalized gingival overgrowth. The patient gingival hyperplasia, idiopathic fibromatosis, had presented himself for examination at the and hypertrophied gingival, is a rare condition same clinic with the same complaint 15 years (1:750000)1 which can present as an isolated ago. At that time, he was treated with full-mouth disorder or more rarely as a syndrome periodontal surgery after the diagnosis of HGF component.2,3 This condition is characterized by had been made following clinical and histological a slow and progressive enlargement of both the examination (Figures 1 A-B). -

ABC of Oral Health Periodontal Disease John Coventry, Gareth Griffiths, Crispian Scully, Maurizio Tonetti
Clinical review ABC of oral health Periodontal disease John Coventry, Gareth Griffiths, Crispian Scully, Maurizio Tonetti Most periodontal disease arises from, or is aggravated by, accumulation of plaque, and periodontitis is associated particularly with anaerobes such as Porphyromonas gingivalis, Bacteroides forsythus, and Actinobacillus actinomycetemcomitans. Calculus (tartar) may form from calcification of plaque above or below the gum line, and the plaque that collects on calculus exacerbates the inflammation. The inflammatory reaction is associated with progressive loss of periodontal ligament and alveolar bone and, eventually, with mobility and loss of teeth. Periodontal diseases are ecogenetic in the sense that, in subjects rendered susceptible by genetic or environmental factors (such as polymorphisms in the gene for interleukin 1, cigarette smoking, immune depression, and diabetes), the infection leads to more rapidly progressive disease. Osteoporosis also seems to have some effect on periodontal bone loss. The possible effects of periodontal disease on systemic Chronic marginal gingivitis showing erythematous oedematous appearance health, via pro-inflammatory cytokines, have been the focus of much attention. Studies to test the strength of associations with atherosclerosis, hypertension, coronary heart disease, cerebrovascular disease, and low birth weight, and any effects on diabetic control, are ongoing. Gingivitis Chronic gingivitis to some degree affects over 90% of the population. If treated, the prognosis is good, but otherwise it may progress to periodontitis and tooth mobility and loss. Marginal gingivitis is painless but may manifest with bleeding from the gingival crevice, particularly when brushing the teeth. The gingival margins are slightly red and swollen, eventually with mild gingival hyperplasia. Management—Unless plaque is assiduously removed and Gingivitis with hyperplasia kept under control by tooth brushing and flossing and, where necessary, by removal of calculus by scaling and polishing by dental staff, the condition will recur. -

Oral Health in Louisiana a Document on the Oral Health Status of Louisiana’S Population
Oral Health in Louisiana A Document on the Oral Health Status of Louisiana’s Population Rishu Garg, MD, MPH Oral Health Program Epidemiologist/Evaluator July 2010 628 N. 4th Street Baton Rouge, LA 70821-3214 Phone: (225) 342-2645 TABLE OF CONTENTS I. Executive Summary……………………………………..…………….…………….1 II. National and State Objectives on Oral Health……………………...………….2 III. The Burden of Oral Diseases……………………………………………………...4 A. Prevalence of Disease and Unmet Needs 1. Children…….……………………………….…….…………………4 2. Adults………………………..……………….……………….……...8 Dental Caries…………………… ……………..….....….…..8 Tooth Loss………… …………………………..….……...….9 Periodontal Diseases……………………….….....……..…..11 Oral Cancer………… ……………………….……….…..….12 B. Disparities 1. Racial and Ethnic Groups………………………………..………..19 2. Socioeconomic………………………………………………......….21 3. Women’s Health……………………………….... …………...……23 4. People with Disabilities……………………. ……………...…….26 C. Societal Impact of Oral Disease 1. Social Impact…………………………………….……..……..……29 2. Economic Impact…………………………….……… ………....…29 Direct Costs of Oral Diseases…..…………..………....….29 Indirect Costs of Oral Diseases………………….……….30 D. Oral Diseases and Other Health Conditions………….................……..31 IV. Risk and Protective Factors Affecting Oral Diseases A. Community Water Fluoridation…………………………………..……32 B. Topical Fluorides and Fluoride Supplements………..…...........…….34 C. Dental Sealants………………………………………...……….….….….35 D. Preventive Visits…………………………………...…………….........….37 E. Screening of Oral Cancer………………………………….…....….……39 F. Tobacco Control……………………………………………….......…..… -

Subgingival Debridement Is Effective in Treating Chronic Periodontitis
&&&&&& SUMMARY REVIEW/PERIODONTOLOGY 3A| 2C| 2B| 2A| 1B| 1A| Subgingival debridement is effective in treating chronic periodontitis Is subgingival debridement clinically effective in people who have chronic periodontitis? review comparing powered and manual scaling3 indicates that both Van der Weijden GA, Timmerman MF. A systematic review on are equally effective. The systematic review of adjunctive systemic the clinical efficacy of subgingival debridement in the treatment antimicrobials4 suggests benefit from their use. Together, these of chronic periodontitis. J Clin Periodontol 2002; 29(suppl. 3): three reviews begin to provide a new view of initial nonsurgical S55–S71. periodontal treatment. That is, scaling with powered instruments Data sources Sources were Medline and the Cochrane Oral Health followed by adjunctive systemic antimicrobials. This view is both Group Specialist Register up to April 2001. Only English-language traditional and progressive. The educational and clinical tradition- studies were included. alists might say that the clinical effectiveness of scaling with hand Study selection Controlled trials and longitudinal studies, with data instruments withstood the test of time and systemic antibiotics analysed at patient level, were chosen for consideration. raise other risks. So, why change? The educational and clinical Data extraction and synthesis Information about the quality and progressive might say that these approaches show promise, and characteristics of each study was extracted independently by two may improve outcomes while reducing clinical effort, time and reviewers. Kappa scores determined their agreement. Data were pooled costs. So, why not try them? when mean differences and standard errors were available using a fixed- Both views are defensible and valid. Thus, if evidence-based effects model. -

Management of Acute Periodontal Abscess Mimicking Acute Apical Abscess in the Anterior Lingual Region: a Case Report
Open Access Case Report DOI: 10.7759/cureus.5592 Management of Acute Periodontal Abscess Mimicking Acute Apical Abscess in the Anterior Lingual Region: A Case Report Omar A. Alharbi 1 , Muhammad Zubair Ahmad 1 , Atif S. Agwan 1 , Durre Sadaf 1 1. Conservative Dentistry, Qassim University, College of Dentistry, Buraydha, SAU Corresponding author: Muhammad Zubair Ahmad, [email protected] Abstract Purulent infections of periodontal tissues are known as periodontal abscesses localized to the region of the involved tooth. Due to the high prevalence rate and aggressive symptoms, it is considered a dental emergency; urgent care is mandatory to maintain the overall health and well being of the patient. This case report describes the management of a patient who presented with an acute periodontal abscess secondary to poor oral hygiene. Clinically and radiographically, the lesion was mimicking an acute apical abscess secondary to pulpal necrosis. Periodontal treatment was started after completion of antibiotic therapy. The clinical presentation of the condition and results of the recovery, along with a brief review of relevant literature are discussed. Categories: Pain Management, Miscellaneous, Dentistry Keywords: periodontal abscess, antimicrobial agents, dental pulp test, dental pulp necrosis, apical suppurative periodontitis Introduction Periodontium, as a general term, describes the tissues surrounding and supporting the tooth structure. A localized purulent infection of the periodontal tissues adjacent to a periodontal pocket, also known as a periodontal abscess, is a frequently encountered periodontal condition that may be characterized by the rapid destruction of periodontal tissues [1-2]. The symptoms generally involve severe pain, swelling of the alveolar mucosa or gingiva, a reddish blue or red appearance of the affected tissues, and difficulty in chewing [1-3]. -
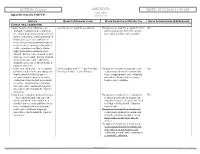
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief
Scottish Dental SD Clinical Effectiveness Programme cep Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief June 2014 Scottish Dental SD Clinical Effectiveness Programme cep The Scottish Dental Clinical Effectiveness Programme (SDCEP) is an initiative of the National Dental Advisory Committee (NDAC) in partnership with NHS Education for Scotland. The Programme provides user-friendly, evidence-based guidance on topics identified as priorities for oral health care. SDCEP guidance aims to support improvements in patient care by bringing together, in a structured manner, the best available information that is relevant to the topic and presenting this information in a form that can be interpreted easily and implemented. Supporting the provision of safe, effective, person-centred care Scottish Dental SD Clinical Effectiveness Programme cep Prevention and Treatment of Periodontal Diseases in Primary Care Guidance in Brief June 2014 Prevention and Treatment of Periodontal Diseases in Primary Care Cover image: Colour-enhanced photomicrograph of oral bacterial colonies growing on an agar plate. Derren Ready, Wellcome Images. © Scottish Dental Clinical Effectiveness Programme SDCEP operates within NHS Education for Scotland. You may copy or reproduce the information in this document for use within NHS Scotland and for non-commercial educational purposes. Use of this document for commercial purposes is permitted only with written permission. ISBN 978 1 905829 18 7 Published June 2014 Scottish Dental Clinical Effectiveness Programme Dundee Dental Education Centre, Frankland Building, Small’s Wynd, Dundee DD1 4HN Email [email protected] Tel 01382 425751 / 425771 Website www.sdcep.org.uk Prevention and Treatment of Periodontal Diseases in Primary Care Introduction Prevention and Treatment of Periodontal Diseases in Primary Care is designed to assist and support primary care dental teams in providing appropriate care for patients both at risk of and with periodontal diseases. -

Review: Differential Diagnosis of Drug-Induced Gingival Hyperplasia and Other Oral Lesions
ISSN: 2469-5734 Moshe. Int J Oral Dent Health 2020, 6:108 DOI: 10.23937/2469-5734/1510108 Volume 6 | Issue 2 International Journal of Open Access Oral and Dental Health REVIEW ARTICLE Review: Differential Diagnosis of Drug-Induced Gingival Hyper- plasia and Other Oral Lesions Einhorn Omer Moshe* Private Dental Office, Israel Check for *Corresponding author: Einhorn Omer Moshe, Private Dental Office, Dr. Einhorn, 89 Medinat Hayehudim updates street, Herzliya, Israel tooth discoloration, alteration of taste sensation and Abstract even appearance of lesions on the tissues of the oral Chronic medication usage is a major component of the cavity. Early recognition and diagnosis of these effects medical diagnosis of patients. Nowadays, some of the most common diseases such as cancer, hypertension, diabetes can largely assist in the prevention of further destruc- and etc., are treated with drugs which cause a variety of oral tive consequences in patients’ health status. As life ex- side-effects including gingival over growth and appearance pectancy increases, the number of elderly patients in of lesions on the tissues of the oral cavity. As such, drug-in- the dental practice also rises. Individuals of this popula- duced oral reactions are an ordinary sight in the dental prac- tice. This review will point out the main therapeutic agents tion are usually subjected to chronic medication intake causing gingival hyperplasia and other pathologic lesions which requires the clinician to be aware of the various in the oral cavity. Some frequently used medications, in side-effects accompanying these medications. This re- particular antihypertensives, nonsteroidal anti-inflammatory view will point out the main therapeutic agents causing drugs and even antibiotics, can lead to overgrowth of the gingival hyperplasia and other pathologic lesions in the gingiva and to the multiple unwanted conditions, namely: Lupus erythematosus, erythema multiforme, mucositis, oral oral cavity. -

Mechanical Debridement with Antibiotics in the Treatment of Chronic Periodontitis: Effect on Systemic Biomarkers—A Systematic Review
International Journal of Environmental Research and Public Health Review Mechanical Debridement with Antibiotics in the Treatment of Chronic Periodontitis: Effect on Systemic Biomarkers—A Systematic Review Sudhir L. Munasur 1, Eunice B. Turawa 1, Usuf M.E. Chikte 2 and Alfred Musekiwa 1,* 1 Division of Epidemiology and Biostatistics, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town 7530, South Africa; [email protected] (S.L.M.); [email protected] (E.B.T.) 2 Division of Health Systems and Public Health, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town 7530, South Africa; [email protected] * Correspondence: [email protected] Received: 5 June 2020; Accepted: 25 June 2020; Published: 3 August 2020 Abstract: In this systematic review, we assessed the effectiveness of systemic antibiotics as an adjunctive therapy to mechanical debridement in improving inflammatory systemic biomarkers, as compared to mechanical debridement alone, among adults with chronic periodontitis. We searched relevant electronic databases for eligible randomized controlled trials. Two review authors independently screened, extracted data, and assessed risk of bias. We conducted meta-analysis, assessed heterogeneity, and assessed certainty of evidence using GRADEPro software. We included 19 studies (n = 1350 participants), representing 18 randomized controlled trials and found very little or no impact of antibiotics on inflammatory biomarkers. A meta-analysis of eight studies demonstrated a mean reduction of 0.26 mm in the periodontal pockets at three months (mean difference [MD] 0.26, 95%CI: 0.36 to 0.17, n = 372 participants, moderate certainty of evidence) in favor of the − − − antibiotics. -

Orofacial Granulomatosis Presenting As Gingival Enlargement – Report of Three Cases
Open Access Journal of Dentistry & Oral Disorders Case Report Orofacial Granulomatosis Presenting as Gingival Enlargement – Report of Three Cases Savithri V*, Janardhanan M, Suresh R and Aravind T Abstract Department of Oral Pathology & Microbiology, Amrita Orofacial Granulomatosis (OFG) is an uncommon disease characterized School of Dentistry, Amrita VishwaVidyapeetham, Amrita by non-caseating granulomatous inflammation in the oral and maxillofacial University, India region. They present clinically as labial enlargement, perioral and/or mucosal *Corresponding author: Vindhya Savithri, swelling, angular cheilitis, mucosal tags, vertical fissures of lips, lingua plicata, Department of Oral Pathology & Microbiology, Amrita oral ulcerations and gingival enlargement. The term OFG was introduced by School of Dentistry, Amrita VishwaVidyapeetham, Amrita Wiesenfeld in 1985. The diagnosis of OFG is done by the clinical presentation University, India and histological picture and this may be further complicated by the fact that OFG may be the oral manifestation of a systemic condition, such as Crohn’s Received: October 16, 2017; Accepted: November 27, disease, sarcoidosis, or, more rarely, Wegener’s granulomatosis. In addition, 2017; Published: December 04, 2017 several conditions, including tuberculosis, leprosy, systemic fungal infections, and foreign body reactions may show granulomatous inflammation on histologic examination. They have to be excluded out by appropriate investigations. They have to be excluded out by appropriate investigations. -

Chronic Inflammatory Gingival Enlargement and Treatment: a Case Report
Case Report Adv Dent & Oral Health Volume 9 Issue 4- July 2018 Copyright © All rights are reserved by Mehmet Özgöz DOI: 10.19080/ADOH.2018.09.555766 Chronic Inflammatory Gingival Enlargement and Treatment: A Case Report Mehmet Özgöz1* and Taner Arabaci2 1Department of Periodontology, Akdeniz University, Turkey 2Department of Periodontology, Atatürk University, Turkey Submission: June 14, 2018; Published: July 18, 2018 *Corresponding author: Özgöz, Department of Periodontology, Akdeniz University Faculty of Dentistry, Antalya, Turkey, Fax:+902423106967; Email: Abstract Gingival enlargement is a common feature in gingival disease. If gingival enlargement isn’t treated, it may some aesthetic problems, plaque accumulation,Keywords: Gingival gingival enlargement; bleeding, and Periodontal periodontitis. treatments; In this paper, Etiological inflammatory factors; Plasma gingival cell enlargement gingivitis and treatment was presented. Introduction and retention include poor oral hygiene, abnormal relationship of Gingival enlargement is a common feature in gingival disease adjacent teeth, lack of tooth function, cervical cavities, improperly contoured dental restorations, food impaction, nasal obstruction, connection with etiological factors and pathological changes [3-5]. [1,2]. Many types of gingival enlargement can be classified in orthodontic therapy involving repositioning of the teeth, and habits such as mouth breathing and pressing the tongue against the gingival [18-20]. a)b) InflammatoryDrug-induced enlargement:enlargement [7-12]. chronic and acute [6]. c) Gingival enlargements associated with systemic diseases: patients to maintain oral hygiene [9,21]. Surgical correction of Overgrowth of the gingival tissue makes it more difficult for i. Conditioned enlargement (pregnancy, puberty, vitamin the gingival overgrowth is still the most frequent treatment. Such treatment is only advocated when the overgrowth is severe.