A Sibling's Guide to Psychosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Placement of Children with Relatives
STATE STATUTES Current Through January 2018 WHAT’S INSIDE Placement of Children With Giving preference to relatives for out-of-home Relatives placements When a child is removed from the home and placed Approving relative in out-of-home care, relatives are the preferred placements resource because this placement type maintains the child’s connections with his or her family. In fact, in Placement of siblings order for states to receive federal payments for foster care and adoption assistance, federal law under title Adoption by relatives IV-E of the Social Security Act requires that they Summaries of state laws “consider giving preference to an adult relative over a nonrelated caregiver when determining a placement for a child, provided that the relative caregiver meets all relevant state child protection standards.”1 Title To find statute information for a IV-E further requires all states2 operating a title particular state, IV-E program to exercise due diligence to identify go to and provide notice to all grandparents, all parents of a sibling of the child, where such parent has legal https://www.childwelfare. gov/topics/systemwide/ custody of the sibling, and other adult relatives of the laws-policies/state/. child (including any other adult relatives suggested by the parents) that (1) the child has been or is being removed from the custody of his or her parents, (2) the options the relative has to participate in the care and placement of the child, and (3) the requirements to become a foster parent to the child.3 1 42 U.S.C. -

Post-Marital Residence Patterns Show Lineage-Specific Evolution
Evolution and Human Behavior xxx (xxxx) xxx–xxx Contents lists available at ScienceDirect Evolution and Human Behavior journal homepage: www.elsevier.com/locate/ens Post-marital residence patterns show lineage-specific evolution Jiří C. Moraveca, Quentin Atkinsonb, Claire Bowernc, Simon J. Greenhilld,e, Fiona M. Jordanf, Robert M. Rossf,g,h, Russell Grayb,e, Stephen Marslandi,*, Murray P. Coxa,* a Statistics and Bioinformatics Group, Institute of Fundamental Sciences, Massey University, Palmerston North, New Zealand b Department of Psychology, University of Auckland, Auckland, New Zealand c Department of Linguistics, Yale University, New Haven, CT 06511, USA d ARC Centre of Excellence for the Dynamics of Language, Australian National University, Canberra, ACT 0200, Australia e Max Planck Institute for the Science of Human History, Jena D-07745, Germany f Department of Anthropology and Archaeology, University of Bristol, Bristol BS8 1TH, UK g Institute for Cognitive and Evolutionary Anthropology, School of Anthropology and Museum Ethnography, University of Oxford, Oxford OX1 2JD, UK h ARC Centre of Excellence in Cognition and its Disorders, Department of Psychology, Royal Holloway, University of London, Surrey TW20 0EX, UK i School of Mathematics and Statistics, Victoria University of Wellington, Wellington, New Zealand ARTICLE INFO ABSTRACT Keywords: Where a newly-married couple lives, termed post-marital residence, varies cross-culturally and changes over Kinship time. While many factors have been proposed as drivers of this change, among them general features of human Post-marital residence societies like warfare, migration and gendered division of subsistence labour, little is known about whether Cross-cultural comparison changes in residence patterns exhibit global regularities. -

Delta-Notch Signaling: the Long and the Short of a Neuron’S Influence on Progenitor Fates
Journal of Developmental Biology Review Delta-Notch Signaling: The Long and the Short of a Neuron’s Influence on Progenitor Fates Rachel Moore 1,* and Paula Alexandre 2,* 1 Centre for Developmental Neurobiology, King’s College London, London SE1 1UL, UK 2 Developmental Biology and Cancer, University College London Great Ormond Street Institute of Child Health, London WC1N 1EH, UK * Correspondence: [email protected] (R.M.); [email protected] (P.A.) Received: 18 February 2020; Accepted: 24 March 2020; Published: 26 March 2020 Abstract: Maintenance of the neural progenitor pool during embryonic development is essential to promote growth of the central nervous system (CNS). The CNS is initially formed by tightly compacted proliferative neuroepithelial cells that later acquire radial glial characteristics and continue to divide at the ventricular (apical) and pial (basal) surface of the neuroepithelium to generate neurons. While neural progenitors such as neuroepithelial cells and apical radial glia form strong connections with their neighbours at the apical and basal surfaces of the neuroepithelium, neurons usually form the mantle layer at the basal surface. This review will discuss the existing evidence that supports a role for neurons, from early stages of differentiation, in promoting progenitor cell fates in the vertebrates CNS, maintaining tissue homeostasis and regulating spatiotemporal patterning of neuronal differentiation through Delta-Notch signalling. Keywords: neuron; neurogenesis; neuronal apical detachment; asymmetric division; notch; delta; long and short range lateral inhibition 1. Introduction During the development of the central nervous system (CNS), neurons derive from neural progenitors and the Delta-Notch signaling pathway plays a major role in these cell fate decisions [1–4]. -
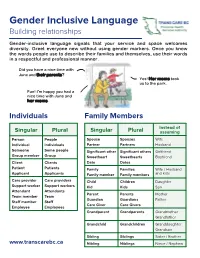
Gender Inclusive Language Building Relationships
Gender Inclusive Language Building relationships Gender-inclusive language signals that your service and space welcomes diversity. Greet everyone new without using gender markers. Once you know the words people use to describe their families and themselves, use their words in a respectful and professional manner. Did you have a nice time with June and their parents? Yes! Her moms took us to the park. Fun! I'm happy you had a nice time with June and her moms. Individuals Family Members Instead of Singular Plural Singular Plural assuming Person People Spouse Spouses Wife Individual Individuals Partner Partners Husband Someone Some people Significant other Significant others Girlfriend Group member Group Sweetheart Sweethearts Boyfriend Client Clients Date Dates Patient Patients Family Families Wife / Husband Applicant Applicants Family member Family members and kids Care provider Care providers Child Children Daughter Support worker Support workers Kid Kids Son Attendant Attendants Parent Parents Mother Team member Team Guardian Guardians Father Staff member Staff Care Giver Care Givers Employee Employees Grandparent Grandparents Grandmother Grandfather Grandchild Grandchildren Granddaughter Grandson Sibling Siblings Sister / Brother www.transcarebc.ca Nibling Niblings Niece / Nephew ii Pronouns (using they in the singular) If you are in a setting where your interactions with people are brief, you may not have time to get to know the person. Using the singular they in these situations can help to avoid pronoun mistakes. subject They They are waiting at the door. object Them The form is for them. possessive Their Their parents will pick them up at 3pm. adjective possessive Theirs They said the wheelchair is not theirs. -
Sister to Sister Compass | Special Edition | 2020-2021 You’Ve Got This in This Edition
GIRL SC ❧ UT STRONG Sister to Sister Compass | Special Edition | 2020-2021 You’ve Got This In this edition: And Girl Scouts of Maine is here for you through it all. Cheering you on, lifting you up, celebrating your strengths. Today, tomorrow, together—we’re on your team. Didn’t renew for 2021? Don’t worry, we have the solution! Starting on April 1, choose Extended Year Membership and renew for both 2021 and 2022 for just $55. Dont miss this opportunity, this is a 2021 exclusive offer! Renew by: Your Girl will get: 5/18 6/1 6/15 ✓ ✓ ✓ Eligibility to register for Celebrate Camp events* ✓ ✓ ✓ Free special GSME Early Renewal Patch for girls ✓ Free We’ve Got This Patch for girls ✓ ✓ $5 bonus for troop per girl renewed online** ✓ $2.50 bonus for troop per girl renewed online** *Spaces are limited for the Celebrate Camp events at Camp Pondicherry and Camp Natarswi and are first come, first served. You must renew to be eligible to register. Registration for Celebrate Camp starts April 1 and closes when full or by June 15 (whichever happens first). Cost for Celebrate Camp is $15/girl and $10/adult. **Must be PAID renewals. Not applicable if paper forms are used or membership assistance is provided. Need help? Contact our Customer Care team at 888-922-4763 or [email protected]. ❧ 2 C mpass A Letter Sister to Sister Edition 2021 from our CEO Editor: Laura Genese Designer: Rebecca Benoski Dear Girl Scouts, It has been a year. In the 400 or so days since a global In this edition: pandemic was declared, we have changed as people and been reshaped as families in many ways, large and small. -

Bereavement Leave
STATE OF CALIFORNIA - DEPARTMENT OF GENERAL SERVICE PERSONNEL OPERATIONS MANUAL SUBJECT: BEREAVEMENT LEAVE REPRESENTED EMPLOYEES Bereavement leave allows for up to three (3) eight-hour days (24 hours) per occurrence or three (3) eight-hour days (24 hours) in a fiscal year based on the family member. The following chart describes the family member and bereavement leave allowed per bargaining unit. Bargaining Unit Eligible family member - three (3) eight-hour days Eligible family member - three (3) (24 hours) per occurrence eight-hour days (24 hours) in a fiscal year 1, 4, 11, 14, 15 • Parent • Aunt • Stepparent • Uncle • Spouse • Niece • Domestic Partner • Nephew • Child • immediate family members of • Grandchild Domestic Partners • Grandparent • Brother • Sister • Stepchild • Mother-in-Law • Father-in-Law • Daughter-in-Law • Son-in-Law • Sister-in-Law • Brother-in-Law • any person residing in the immediate household 2 • Parent • Grandchild • Stepparent • Grandparent • Spouse • Aunt • Domestic Partner • Uncle • Child • Niece • Sister • Nephew • Brother • Mother-in-Law • Stepchild • Father-in-Law • any person residing in the immediate household • Daughter-in-Law • Son-in-Law • Sister-in-Law • Brother-in-Law • immediate family member 7 • Parent • Grandchild • Stepparent • Grandparent • Spouse • Aunt • Domestic Partner • Uncle STATE OF CALIFORNIA - DEPARTMENT OF GENERAL SERVICE PERSONNEL OPERATIONS MANUAL Bargaining Unit Eligible family member - three (3) eight-hour days Eligible family member - three (3) (24 hours) per occurrence eight-hour -

Sister Maura Therese Power, RSM Sisters of Mercy of Auburn, California
SACRAMENTO DIOCESAN ARCHIVE Vol 7 Father John E Boll No 2 Sister Maura Therese Power, RSM Sisters of Mercy of Auburn, California Maura Therese Power was born on October 8, 1937, in Killarney, County Kerry, Ireland. She and her twin brother John Joseph were born to Denis Power and Philomena Freeley. Two days later, Maura and John were baptized at the Cathedral in Killarney. In addition to her twin brother, she has an older brother Gerard and a younger sister Noreen. The last born child was Catherine “Riona” who died at the age of seven, having lived with Down syndrome. BEGINNING THE EDUCATION PROCESS All the children of the Power family began their education at age four at the Mercy Convent School in Killarney. After each child received First Holy Communion, the boys went to the Presentation Brothers School and the girls continued with the Mercy Sisters. FAMILY FORCED TO MOVE TO DUBLIN Maura’s father Denis worked in Hilliard’s Department Store. When labor disputes arose in the mid-1940s, Denis lost his job at the store and was forced to go to Dublin to look for another position. He secured a new job in Dublin and the family moved to Dublin in 1949. Since this was right after the end of World War II, life was difficult for everyone in Europe as well as the Power family in Ireland. After arriving in Dublin, the family settled in Clontarf along the coast in a new house that Maura’s father was able to purchase. She began secondary school with the Irish Sisters of Charity on King’s Inn Street. -
WILLIAM F. KEEGAN an ANTHROPOLOGICAL EVALUATION of TAINO KINSHIP INTRODUCTION This Is the Fourth in a Series of Papers in Which
WILLIAM F. KEEGAN AN ANTHROPOLOGICAL EVALUATION OF TAINO KINSHIP INTRODUCTION This is the fourth in a series of papers in which the social and political organizations of the Tainos are examined. The first paper, presented at the Society for American Archaeology meeting in 1987, explored the relationship between patterns of settlement and social organization (Keegan 1987). The second, published in American Anthropologist, is an archeo-ethnological collaboration in which ethnographic information was used to reconstruct Taino kinship and changes in Lucayan settlement patterns were used to examine Melvin Ember's (1974) model of the evolution of avunculocal residence (Keegan and MacLachlan 1989). The third paper, presented at the "Processual/Post-Processual Debate," further developed a materialist model of Taino social organization and described the research methodology used to explore that model (Keegan 1990). Rather than review those previous studies, I wish to begin the present paper with the assumption that Taino sociopolitical organization can be characterized as an avunculocal chiefdom. Assume, if you wish, that Rouse (1948) in the Handbook of South American Indians described the Tainos as practicing matrilineal descent, and avunculocal residence rather than patrilocal residence. That is the basis for the present paper, which is presented in three parts. First, I define what I mean by avunculocal chiefdom; second, I describe some of the more important behavioral implications; and third, I explore the archaeological implications of such an organization. AVUNCULOCAL CHIEFDOMS The term "avunculocal chiefdom" contains both social and political implications. Avunculocal residence involves the movement of males at adolescence to live with a real or classificatory maternal uncle where they are joined at marriage by their wives. -

Grandparents Day Supplement
2015 Grandparents Day Supplement A Hindu Cultural Center of Albany Hindu Temple Society’s Newsletter devoted to the Capital District’s Indian-American community particularly its seniors s Grandparents Day Celebration By Ram Chugh, Ph.D. on to us religious, cultural, moral, and social values they learned from The Hindu Cultural Center (HCC) Board deserves commendation for their own parents and grandparents. sponsoring the first Grandparents Day Celebration on Sunday, .September 13 from 12 to 5 PM to honor our grandparents. The ۰ In particular, they form special bonds with their grandchildren celebration coincided with the National Grandparents Day in the They share stories of their lives with them, play games, read books, United States. laugh and even cry with them. Over 200 people attended the ۰ While playing with their grandchildren, grandparents become event at the HCC, including about 80 children again. In the process, they enrich their own lives and those grandparents and 120 children and of their grandchildren. grandchildren. There were also six ۰ They also become distant observers of the cycle of life and the grandparents from outside the Capital passage of time. They think of their own childhood and of their own District in attendance. Most of them had grandparents. come from India to visit their children and grandchildren and happened to ۰ There is then a realization that, like their own grandparents who be in Albany on the day of the continue to live through them, they will continue to live in the minds celebration. and hearts of their grandchildren as well. The auditorium was decorated for I indicated that in his Grandparents Day message, President the occasion with a large Barrack Obama had said: “On National Grandparents Day, we “Grandparents Day” banner, colorful balloons, flowers, and posters honor the anchors of our families and recognize the immeasurable ways they enrich our lives.” I added that is exactly what we were containing pictures of grandchildren and messages written by them to their grandparents. -

JAMES/ALOYSIUS #1 SISTER JAMES: Well. What a Relief! He Cleared It
JAMES/ALOYSIUS #1 SISTER JAMES: Well. What a relief! He cleared it all up. SISTER ALOYSIUS: You believe him? SISTER JAMES: Of course. SISTER ALOYSIUS: Isn’t it more that it’s easier to believe him? SISTER JAMES: Be we can corroborate his story with Mr. McGinn! SISTER ALOYSIUS: Yes. These types of people are clever. They’re not so easily undone. SISTER JAMES: Well, I’m convinced. SISTER ALOYSIUS: You’re not. You just want things to be resolved so that you can have simplicity back. SISTER JAMES: I want no further part of this. SISTER ALOYSIUS: I’ll bring him down. With or without your help. SISTER JAMES: How can you be so sure he’s lying? SISTER ALOYSIUS: Experience. SISTER JAMES: You just don’t like him! You don’t like it that he uses a ballpoint pen. You don’t like it that he takes three lumps of sugar in his tea. You don’t like it that he likes “Frosty the Snowman.” And you’re letting that convince you of something terrible, just terrible! Well, I like “Frosty the Snowman”! And it would be nice if this school weren’t run like a prison! And I think it’s a good thing that I love to teach History and that I might inspire my students to love it, too! And if you judge that to mean I’m not fit to be a teacher, than so be it! SISTER ALOYSIUS: Sit down. (Sister James does.) In ancient Sparta, important matters were decided by who shouted loudest. -

Avunculocal Residence on Losap MOLLIEN,G
1024 A men"can Anthropologist [57, 1955] MINER) HORACE 1953 The primitive city of Timbuctoo. Princeton. Avunculocal Residence on Losap MOLLIEN, G. 1820 Travels in the interior of Mrica to the sources of the Senegal and Gambia, ed. T. E. J. L. FISCHER Bowdich. London. Excerpts provided by D. P. Gamble. Harvard University Moon,:, FRANCIS 1738 Travels into the inland parts of Mrica. London. HE purpose of this paper is to report a contemporary instance of avuncu P AlUC, MUNGO T local residence in Micronesia, on the island of Losap, Truk. District, and 1799 Travels in the interior districts of Africa. Reissued in Everyman's Library (1907). to discuss possible reasons for the presence of this trait on Losap, surrounded SAUGNIER, M. 1791 Relations de plusieurs voyages a la c6te d'Afrique, a Maroc, au Senegal, a Goree, a as it is by matrilocal societies to the north and south. Galam, etc. Paris. Losap Atoll is located about fifty miles southeast of Truk Lagoou iu the SELEcr COM1lollTTEE ON WEST COAST OF AFRICA east central Caroline Islands. The nearest land is the single coral island of 1842 Quotation provided by D. P. Gamble. Nama, about twelve miles to the northeast. Both Losap and Nama lie along THlLENIUS, G. a route between Truk and the Mortlock (also known as Ku or Nomoi) Islands, 1920 Primitives Geld. Archiv fur AnthropoJogie, n.s. 18:1-33. a group of atolls roughly 100 to 150 miles southeast of Truk. TauRNwALD, RICHARD 1932 Economics in primitive communities. London. Culturally, too, Losap is in many ways intermediate between Truk and the WYNDHAM, H. -

Implications of Human Evolution and Admixture for Mitochondrial Replacement Therapy Lavanya Rishishwar1,2,3 and I
RESEARCHARTICLE Open Access Implications of human evolution and admixture for mitochondrial replacement therapy Lavanya Rishishwar1,2,3 and I. King Jordan1,2,3* Abstract Background: Mitochondrial replacement (MR) therapy is a new assisted reproductive technology that allows women with mitochondrial disorders to give birth to healthy children by combining their nuclei with mitochondria from unaffected egg donors. Evolutionary biologists have raised concerns about the safety of MR therapy based on the extent to which nuclear and mitochondrial genomes are observed to co-evolve within natural populations, i.e. the nuclear-mitochondrial mismatch hypothesis. In support of this hypothesis, a number of previous studies on model organisms have provided evidence for incompatibility between nuclear and mitochondrial genomes from divergent populations of the same species. Results: We tested the nuclear-mitochondrial mismatch hypothesis for humans by observing the extent of naturally occurring nuclear-mitochondrial mismatch seen for 2,504 individuals across 26 populations, from 5 continental populations groups, characterized as part of the 1000 Genomes Project (1KGP). We also performed a replication analysis on mitochondrial DNA (mtDNA) haplotypes for 1,043 individuals from 58 populations, characterized as part of the Human Genome Diversity Project (HGDP). Nuclear DNA (nDNA) and mtDNA sequences from the 1KGP were directly compared within and between populations, and the population distributions of mtDNA haplotypes derived from both sequence (1KGP) and genotype (HGDP) data were evaluated. Levels of nDNA and mtDNA pairwise sequence divergence are highly correlated, consistent with their co-evolution among human populations. However, there are numerous cases of co-occurrence of nuclear and mitochondrial genomes from divergent populations within individual humans.