February Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Book ^ Can's Tago Mago » E1MZS7WYAL2L
ZVIMZOGVKZMA < eBook < Can's Tago Mago Can's Tago Mago Filesize: 4.03 MB Reviews Simply no words to explain. It really is basic but shocks from the fifty percent of the ebook. I am just happy to explain how this is the finest pdf we have read within my personal life and could be he best ebook for possibly. (Blair Monahan) DISCLAIMER | DMCA K3QZLZZUT07P ^ Book < Can's Tago Mago CAN'S TAGO MAGO To get Can's Tago Mago PDF, please access the button under and save the file or get access to additional information that are in conjuction with CAN'S TAGO MAGO book. Bloomsbury Publishing Plc. Paperback. Book Condition: new. BRAND NEW, Can's Tago Mago, Alan Warner, Finally, a brilliant exploration of the German rock band Can's 1971 album Tago Mago. This hugely unique and influential album deserves close analysis from a fan, rather than a musicologist. Novelist Alan Warner details the concrete music we hear on the album, how it was composed, executed and recorded--including the history of the album in terms of its release, promotion and art work. This tale of Tago Mago is also the tale of a young man obsessed with record collecting in the dark and mysterious period of pop music before Google. Warner includes a backtracking of the history of the band up to that point and also some description of Can's unique recording approach taking into account their home studio set up. Interviews with the two surviving members: drummer Jaki Liebezeit, keyboardist Irmin Schmidt and bassist Holger Czukay make this a hilariously personal and illuminating picture of Can. -

Classic Albums: the Berlin/Germany Edition
Course Title Classic Albums: The Berlin/Germany Edition Course Number REMU-UT 9817 D01 Spring 2019 Syllabus last updated on: 23-Dec-2018 Lecturer Contact Information Course Details Wednesdays, 6:15pm to 7:30pm (14 weeks) Location NYU Berlin Academic Center, Room BLAC 101 Prerequisites No pre-requisites Units earned 2 credits Course Description A classic album is one that has been deemed by many —or even just a select influential few — as a standard bearer within or without its genre. In this class—a companion to the Classic Albums class offered in New York—we will look and listen at a selection of classic albums recorded in Berlin, or recorded in Germany more broadly, and how the city/country shaped them – from David Bowie's famous Berlin trilogy from 1977 – 79 to Ricardo Villalobos' minimal house masterpiece Alcachofa. We will deconstruct the music and production of these albums, putting them in full social and political context and exploring the range of reasons why they have garnered classic status. Artists, producers and engineers involved in the making of these albums will be invited to discuss their seminal works with the students. Along the way we will also consider the history of German electronic music. We will particularly look at how electronic music developed in Germany before the advent of house and techno in the late 1980s as well as the arrival of Techno, a new musical movement, and new technology in Berlin and Germany in the turbulent years after the Fall of the Berlin Wall in 1989, up to the present. -

FUTURE SOUNDS Wie Ein Paar Krautrocker Die Popwelt Revolutionierten
FVTVRE SOVNDS Wie ein paar »Krautrocker« Christoph Dallach die Popwelt revolutionierten Suhrkamp SV Christoph Dallach FUTURE SOUNDS Wie ein paar Krautrocker die Popwelt revolutionierten Suhrkamp Für Maria (MoisE) Erste Auflage 2021 suhrkamp taschenbuch 4598 Originalausgabe © Suhrkamp Verlag Berlin 2021 Suhrkamp Taschenbuch Verlag Alle Rechte vorbehalten, insbesondere das der Übersetzung, des öffentlichen Vortrags sowie der Übertragung durch Rundfunk und Fernsehen, auch einzelner Teile. Kein Teil des Werkes darf in irgendeiner Form (durch Fotografie, Mikrofilm oder andere Verfahren) ohne schriftliche Genehmigung des Verlages reproduziert oder unter Verwendung elektronischer Systeme verarbeitet, vervielfältigt oder verbreitet werden. Umschlaggestaltung : Büro Dirk Rudolph Druck : C.H.Beck, Nördlingen Printed in Germany ISBN 978-3-518-46598-1 Inhalt Vorwort von Christoph Dallach 7 Kraut 11 DIE FÜNFZIGER Nachkriegsjugend 21 Jazz 50 DIE SECHZIGER Beat 71 Haare 86 WGs 94 1968 103 Neuanfang 127 Drogen 143 Zodiak 153 Kluster 163 DIE SIEBZIGER Kessler 173 Tangerine Dream 187 Kommerz 211 Moog 215 Amon Düül 225 A. R & Machines 244 Eigenpfade 252 Weltenbummler 271 Faust 280 Austausch 314 Can 320 Plank 367 Kraftwerk 376 Neu ! 384 Forst 393 Ausland 404 Staatsfeinde 413 Rolf-Ulrich Kaiser 427 Deutsch 464 Ende 469 Heute 472 Für immer (always) 478 Biografische Notizen 493 Bildnachweise 511 Danksagung 512 Vorwort von Christoph Dallach Meine erste Krautrockplatte gewann ich in einem Preisaus- schreiben. Die Aufgabe bestand darin, innerhalb eines knap- pen Zeitfensters irgendwo anzurufen. Ich kam sofort durch. Vielleicht hatte ich Glück, vielleicht war ich aber auch der einzige Anrufer. Egal, eine Woche darauf war die Platte da : »Movies« von Holger Czukay, mit krakeliger Kugelschreiber- Signatur vom Künstler höchstpersönlich. -

Can Delay 1968 Mp3, Flac, Wma
Can Delay 1968 mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Electronic / Rock Album: Delay 1968 Country: Germany Released: 1981 Style: Krautrock, Psychedelic Rock, Experimental MP3 version RAR size: 1450 mb FLAC version RAR size: 1540 mb WMA version RAR size: 1282 mb Rating: 4.6 Votes: 357 Other Formats: VOC VOX MP1 WAV AIFF DMF MOD Tracklist A1 Butterfly 8:20 A2 Pnoom 0:26 A3 Nineteen Century Man 4:18 A4 Thief 5:03 B1 Man Named Joe 3:54 B2 Uphill 6:41 B3 Little Star Of Bethlehem 7:09 Companies, etc. Recorded At – Schloß Nörvenich Produced At – Inner Space Studio Credits Bass, Engineer, Edited By – Holger Czukay Drums – Jaki Liebezeit Guitar – Michael Karoli Keyboards – Irmin Schmidt Lacquer Cut By – J.C.* Layout [Hüllengestaltung] – Eveline Grunwald Management – Hildegard Schmidt Photography By – Walter Kirchberger Producer – Can Vocals – Malcolm Mooney Written-By – Czukay*, Schmidt*, Liebezeit*, Mooney*, Karoli* Notes Recorded 1968/69 at Schloss Nörvenich. Barcode and Other Identifiers Rights Society: GEMA Label Code: LC 7395 Matrix / Runout (Label side A): 66.22 735-01-1 Matrix / Runout (Label side B): 66.22 735-01-2 Matrix / Runout (Runout side A, hand-etched): -CAN- "DELAY" Side one 012-A Matrix / Runout (Runout side B, hand-etched): -CAN- "DELAY" Side Two 012-B J.C. Other versions Title Category Artist Label Category Country Year (Format) Spoon Records, Delay 1968 Warner CDSPOON 12, CDSPOON 12, Can (CD, Album, Music Germany 2007 5051442-3553-2-1 5051442-3553-2-1 RE, RM) Group Central Europe Delay 1968 Japan JAL-2301 Can (LP, -

Damo Suzuki & Robor
dossier de presse première suisse / création 2013 (jp / ch) damo suzuki & robor musiQue Un kamikaze vocal qui a fait le bonheur du krautrock de Can dans les années 70 et 80. Le Japonais Damo Suzuki a rejoint le groupe allemand le plus in- fluent avec Kraftwerk par hasard, en montant sur scène et en improvisant de façon hallucinée. Entre la virtuosité rock et électronique de Can et la folie punk de Suzuki, le mélange est explosif. Après avoir longtemps raccroché le micro, Suzuki est finalement revenu avec un projet givré inédit baptiséDamo Suzuki’s Network, où il improvise de A à Z avec des groupes toujours diffé- rents. A La Bâtie, ce sont les Genevois de Robor qui verront toutes leurs certitudes voler en éclat durant cette rencontre inédite placée sous le signe de l’inatten- du et de la spontanéité. L’entité electro composée de POL et Ghostape, qui production célèbre par l’improvisation les noces psychédéliques des vieux synthétiseurs Robor et des technologies modernes, devrait voir s’ajouter une corde délurée à son coproduction arc. Orageux. La Bâtie-Festival de Genève after Kraut Wave avec GLACE (perfo live/ch) & Djs en collaboration avec la gravière www.damosuzuki.com ©Matias Corral ve 6 sept 22h la gravière le projet Damo suzuki’s Network On stage in Seattle, I had a four track tape recorder Damo Suzuki’s Network is an assembly of musicians. that I would occasionally use much in the same way It’s a collective meeting place where like minded that Holger Czukay used dictaphones with Can. -

C.A.R. Presskit
C.A.R. Presskit We could go the long way around and talk about German post- war music history such as “Krautrock” , “Kosmische” and “Jazz- Rock” and what these terms mean to us. But we could also just say: “Hello, we are C.A.R. from Cologne and we play music as we like it: A little bit acoustic, a little bit electronic; on a trip, but without a specific destination; intense but not brutal; spherical, but not arbitrary; excessive, yet precise. Does this help you? No? Then stay a while and listen!” http://thisiscar.de https://www.facebook.com/thisiscar/ https://thisiscar.bandcamp.com/releases Contact Kenn Hartwig +49 176 23567404 [email protected] C.A.R. @ G5A, Mumbai, 2017 This is C.A.R. C.A.R. was founded in 2011 by Johannes Klingebiel and Kenn Hartwig in Cologne, Germany. After an early period of artistic orientation they released “Beyond The Zero” (2014), the “Interlude EP” (2017), “Look Behind You” (2018) and „Befunde ab 1999“ (2020). Originally playing experimental jazz, the media recently labeled their music as Krautrock, Kosmische, Electronica and experimental Pop. Among the highlights of the band´s career were gigs and residencies such as Fusion Festival, Jazzfest Kolkata and Casa Banchel in Madrid. By invitation of the Goethe Institute C.A.R. went on a four week long tour playing concerts in Pakistan, Sri Lanka and India in 2017. In November 2018 they went to China to play four concerts, taking part in the Jazz Improvise Meeting Festival. In 2019, C.A.R. curated and hosted the concert series “C.A.R. -

Eurythmics in the Garden Mp3, Flac, Wma
Eurythmics In The Garden mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Rock Album: In The Garden Country: Germany Released: 1981 Style: New Wave, Pop Rock, Synth-pop MP3 version RAR size: 1257 mb FLAC version RAR size: 1797 mb WMA version RAR size: 1520 mb Rating: 4.8 Votes: 770 Other Formats: VOX XM MP3 MPC AAC WMA RA Tracklist Hide Credits English Summer A1 4:00 Drums – Clem BurkeGuitar – Dave Stewart*, Roger Pomphrey Belinda A2 3:58 Drums – Robert GörlFrench Horn – Holger Czukay Take Me To Your Heart A3 3:32 Drums – Jaki Liebezeit She's Invisible Now A4 3:27 Drums – Clem Burke Your Time Will Come A5 Brass – Holger Czukay, Jaki Liebezeit, Marcus Stockhausen*Drums – Clem BurkeGuitar – 4:30 Holger Czukay, Roger Pomphrey Caveman Head B1 3:56 Drums – Clem BurkeGuitar, Other [Shouting] – Roger Pomphrey Never Gonna Cry Again B2 3:02 Drums – Jaki LiebezeitFrench Horn – Holger CzukaySaxophone – Sir Timothy Wheater* All The Young (People Of Today) B3 4:11 Drums – Jaki Liebezeit Sing-Sing B4 4:03 Drums – Clem BurkeGuitar – Roger Pomphrey Revenge B5 4:31 Drums – Clem BurkeOther [Laughing] – Krista Fast Companies, etc. Made By – RCA Schallplatten GmbH Phonographic Copyright (p) – Dilkusa Music B.V. Recorded At – Conny's Studio Phonographic Copyright (p) – RCA Ltd. Credits Bass, Keyboards, Synthesizer, Backing Vocals – Dave Stewart* Design – Rocking Russian Keyboards, Synthesizer, Percussion, Flute, Vocals – Annie Lennox Photography By – Peter Ashworth Producer – Conny Plank, Eurythmics Written-By – Annie Lennox, Dave Stewart*, Roger Pomphrey (tracks: A1, B1) Notes Recorded at Conny's studio, Cologne between February 81 & June 81. "Jaki Liebezeit" is credited as "Jackie Liebzeik" on the album credits. -

2017 CATALOGUE for Over Forty Years Omnibus Press Has Been Publishing the Stories That Matter from the Music World
2017 CATALOGUE For over forty years Omnibus Press has been publishing the stories that matter from the music world. Omnibus Press is the World’s/Europe’s largest specialist publisher devoted to music writing, with around thirty new titles a year, with a backlist of over two hundred and seventy titles currently in print and many more as digital downloads. Omnibus Press covers pop, rock, classical, metal, country, psyche, prog, electronic, dance, rap, jazz and many more genres, in a variety of formats. With books that tell stories through graphic art and photography, memoirs and biographies, Omnibus has constantly evolved its list to challenge what a music book can be and this year we are releasing our first talking books. Among Omnibus Press’ earliest acquisitions was Rock Family Trees, by acclaimed music archivist Pete Frame, three editions of which remain in print to this day and have been the basis of two BBC TV series. Over the following decades Omnibus published many best-selling, definitive biographies on some of rock’s greatest superstars. These include Morrissey & Marr: The Severed Alliance by Johnny Rogan, Dear Boy: The Life Of Keith Moon by Tony Fletcher, Uptight: The Velvet Underground Story by Victor Bockris, Catch A Fire: The Life of Bob Marley by Timothy White, Stevie Nicks - Visions, Dreams & Rumours by Zoë Howe, Without Frontiers The Life And Music Of Peter Gabriel by Daryl Easlea and Under The Ivy: The Life & Music of Kate Bush and George Harrison: Behind The Locked Door, both by Graeme Thomson, all of which are regularly cited by magazines and critics as being amongst the finest rock biographies ever published. -

Freier Download BA 85 Als
BAD 85 ALCHEMY ORWELLHUXLEYWELT SOFT POWER KRIKELKRAKEL L' IMPARFAIT MULTIPLE DE DIEU ANTHROPOZÄN THE SCIENCE OF SNOW DIE UNSICHTBAREN STÄDTE OLDMANESOX OPOSSUM PRAVDA IF, BWANA LEN!IN DADA PORTRAITS OF MELANCHOLICS SIMULAKREN DRITTER ORDNUNG ROGER CAILLOIS THE HORROR AS WE MOVE LIKE RAZOR BLADES IN THE DARK Urteile sind nur wertvoll, wenn sie bejahen. Wirklich wahr sind wir nur, wo wir anerkennen. Das Feststellen von ‚Fehlern’, und klinge es noch so fein und geistig, ist nicht Urteil, sondern Klatsch. Hermann Hesse There are worse crimes than burning books. One of them is not reading them. Ray Bradbury O Wort, du Wort, das mir fehlt: Henri Alain-Fournier - Der große Meaulnes Jaume Cabré - Das Schweigen des Sammlers Otto Flake - Fortunat; Ein Mann von Welt Marcel Proust - Sodom und Gomorra Sergio Toppi - The Collector 2 Artcore Action Heroes oder "Schlockmasters of the Universe" Für mich als 1,55 m kleinen Muck war es am 21. Februar 2015 höchste Zeit, dem Plastischen Theater Hobbit in Würzburg einen Besuch abzustatten. Aber was wird hier eigentlich gespielt oder anders gefragt: Wer spielt was? Drei Männer und eine Frau mit Gliederpuppen-Actionfiguren auf einer apokalyptischen Spielwiese. Das ist „Artcore Action Heroes“, dem kreativen Kopf des unterfränkischen Künstlers Felix „Schlock- master“ Weber entsprungen, der mit diesem eigenwilligen Theaterstück seine eigenen Comics adaptiert. Superhelden nicht wie ge- wöhnlich auf der großen Leinwand, sondern auf einer kleinen Kellerbühne. „Heidi ist die ALLERschönste! Heidi ist TOTAL toll!“ Heidi, die stärkste Frau der Welt, liebt die Elitesoldatin Jane. Jane ist aber mit dem Ex- Polizisten John verbandelt, der wiederum Heidi liebt. -

Keith Carlock
APRIZEPACKAGEFROM 2%!3/.34/,/6%"),,"25&/2$s.%/.42%%3 7). 3ABIANWORTHOVER -ARCH 4HE7ORLDS$RUM-AGAZINE 'ET'OOD 4(%$25--%23/& !,)#)!+%93 $!.'%2-/53% #/(%%$ 0,!.4+2!533 /.345$)/3/5.$3 34!249/52/7. 4%!#().'02!#4)#% 3TEELY$AN7AYNE+RANTZS ,&*5)$"3-0$,7(9(%34(%-!.4/7!4#( s,/52%%$34/.9h4(5.$%2v3-)4( s*!+),)%"%:%)4/&#!. s$/5",%"!3335"34)454% 2%6)%7%$ -/$%2.$25--%2#/- '2%43#(052%7//$"%%#(3/5,4/.%/,$3#(//,3*/9&5,./)3%%,)4%3.!2%3%6!.34/-0/7%2#%.4%23 Volume 35, Number 3 • Cover photo by Rick Malkin CONTENTS 48 31 GET GOOD: STUDIO SOUNDS Four of today’s most skilled recording drummers, whose tones Rick Malkin have graced the work of Gnarls Barkley, Alicia Keys, Robert Plant & Alison Krauss, and Coheed And Cambria, among many others, share their thoughts on getting what you’re after. 40 TONY “THUNDER” SMITH Lou Reed’s sensitive powerhouse traveled a long and twisting musical path to his current destination. He might not have realized it at the time, but the lessons and skills he learned along the way prepared him per- fectly for Reed’s relentlessly exploratory rock ’n’ roll. 48 KEITH CARLOCK The drummer behind platinum-selling records and SRO tours reveals his secrets on his first-ever DVD, The Big Picture: Phrasing, Improvisation, Style & Technique. Modern Drummer gets the inside scoop. 31 40 12 UPDATE 7 Walkers’ BILL KREUTZMANN EJ DeCoske STEWART COPELAND’s World Percussion Concerto Neon Trees’ ELAINE BRADLEY 16 GIMME 10! Hot Hot Heat’s PAUL HAWLEY 82 PORTRAITS The Black Keys’ PATRICK CARNEY 84 9 REASONS TO LOVE Paul La Raia BILL BRUFORD 82 84 96 -
View the Redux Book Here
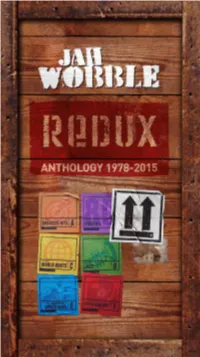
1 Photo: Alex Hurst REDUX This Redux box set is on the 30 Hertz Records label, which I started in 1997. Many of the tracks on this box set originated on 30 Hertz. I did have a label in the early eighties called Lago, on which I released some of my first solo records. These were re-released on 30 Hertz Records in the early noughties. 30 Hertz Records was formed in order to give me a refuge away from the vagaries of corporate record companies. It was one of the wisest things I have ever done. It meant that, within reason, I could commission myself to make whatever sort of record took my fancy. For a prolific artist such as myself, it was a perfect situation. No major record company would have allowed me to have released as many albums as I have. At the time I formed the label, it was still a very rigid business; you released one album every few years and ‘toured it’ in the hope that it became a blockbuster. On the other hand, my attitude was more similar to most painters or other visual artists. I always have one or two records on the go in the same way they always have one or two paintings in progress. My feeling has always been to let the music come, document it by releasing it then let the world catch up in its own time. Hopefully, my new partnership with Cherry Red means that Redux signifies a new beginning as well as documenting the past. -

Drum Innovator Liebezeit of Krautrock Band Can Dies
TUESDAY, JANUARY 24, 2017 l i f e s t y l e MUSIC & MOVIES Picture taken on December 1, 1971 shows members of the band “Can” (from left) Irmin Schmidt, Jaki Liebezeit, Picture shows German musicians Jaki Liebezeit (left, drums) and Marcus Schmickler performing during a festival in Michael Karoli, Ulli Gerlach, Holger Szukay and Damo Suzuki (foreground) posing in Hamburg, northern Germany. Moers, western Germany. — AFP photos Drum innovator Liebezeit of Krautrock band Can dies aki Liebezeit, the percussionist for German band Can who and early electronics. Liebezeit had his start in free jazz, moving the power of striking all drums with his arms rather than kicking want to say imperialistic, but it makes it so that you cannot think became an icon in avant-garde circles for a machine-like after his early studies to Barcelona where he notably played with with his feet and only sparingly used cymbals, while embracing in another way," he told the British cultural magazine The Jstyle that rejected standard drumsets, died Sunday. He was visiting trumpeting great Chet Baker. But Liebezeit grew disen- electronics and percussion instruments that are less common in Quietus in 2015. Can was nonetheless influenced by US avant- 78. His bandmates in Can, which he co-founded in Cologne in chanted with the jazz circuit. He sought to learn percussion from rock such as gongs. Liebezeit would explain that the standardi- garde music including rockers The Velvet Underground and min- 1968, said Liebezeit died suddenly from pneumonia. He died around the world and, with Can, developed a tight, metronome- zation of drumsets, contrary to popular imagination, was a imalist composer Steve Reich.