Shoulder Dislocation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Shoulder Injuries: Dislocated Shoulder and Labral Tear
Orthopedics Shoulder Injuries: Dislocated Shoulder and Labral Tear The anatomy of the shoulder allows it to be one of the body's most mobile joints. It is not like a ball and socket but instead more like a golf ball and a golf tee. The tee portion is called the glenoid, and the ball portion is called the humeral head (top of the humerus). This allows the arm to rotate freely in many directions. Because of this mobility, however, the shoulder is easy to dislocate. A dislocated shoulder occurs when the humeral head comes partially or completely out of place. When the shoulder dislocates, the outer rim of the glenoid (called the labrum) is often injured. Damage also occurs to the ligaments and capsule that normally hold the shoulder in place. Labral tears can also occur when the shoulder slides partially out of joint. Shoulder pain in throwing athletes can also be due to a labral tear that has gradually formed over time. CAUSES AND RISK FACTORS A dislocated shoulder can occur while playing contact sports, such as football or hockey, or in sports where athletes are likely to fall – skiing, volleyball or gymnastics. A sudden, powerful blow to the shoulder causes the dislocation. Less commonly, the ligaments around the shoulder can be so loose that the shoulder can dislocate without much force at all. Once the shoulder dislocates, it is much more likely to happen again. After a second time, the risk is even greater. The younger the athlete, the more likely that dislocation will happen again.A labral tear without dislocation most commonly happens to baseball pitchers, weightlifters and golfers. -
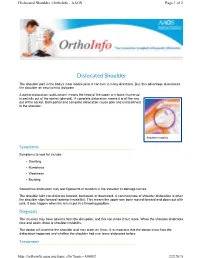
Dislocated Shoulder -Orthoinfo - AAOS Page 1 of 2
Dislocated Shoulder -OrthoInfo - AAOS Page 1 of 2 Dislocated Shoulder The shoulder joint is the body's most mobile joint. It can turn in many directions. But, this advantage also makes the shoulder an easy joint to dislocate. A partial dislocation (subluxation) means the head of the upper arm bone (humerus) is partially out of the socket (glenoid). A complete dislocation means it is all the way out of the socket. Both partial and complete dislocation cause pain and unsteadiness in the shoulder. Shoulder instability Symptoms Symptoms to look for include: • Swelling • Numbness • Weakness • Bruising Sometimes dislocation may tear ligaments or tendons in the shoulder or damage nerves. The shoulder joint can dislocate forward, backward, or downward. A common type of shoulder dislocation is when the shoulder slips forward (anterior instability). This means the upper arm bone moved forward and down out of its joint. It may happen when the arm is put in a throwing position. Diagnosis The muscles may have spasms from the disruption, and this can make it hurt more. When the shoulder dislocates time and again, there is shoulder instability. The doctor will examine the shoulder and may order an X-ray. It is important that the doctor know how the dislocation happened and whether the shoulder had ever been dislocated before. Treatment http://orthoinfo.aaos.org/topic.cfm?topic=A00035 2/2/2015 Dislocated Shoulder -OrthoInfo - AAOS Page 2 of 2 The doctor will place the ball of the upper arm bone (humerus) back into the joint socket. This process is called closed reduction. Severe pain stops almost immediately once the shoulder joint is back in place. -

Sports Injuries
Sports Injuries Lacrosse Lacrosse is America’s oldest game. It can be dated back to the Native Americans, and was used astraining for war. It is both played by boys and girls,however, some rules are drastically different between genders. Nonetheless, the combination of contact, a stick, a hard ball, and quick changes of direction, puts lacrosse players at risk for injury. Protective Equipment There is a wide range of equipment that lacrosse players wear. For girls, goggles and mouth pieces are mandatory. Lightweight gloves and headgear is optional. For boys, helmets with full face guards, shoulder pads, padded gloves, and mouth pieces are used. It is most important for this equipment to fit properly. If equipment does not fit properly it can actually cause injury. There is no helmet which has been proven through research that confused with a “dislocated shoulder,” which is when prevents concussions. the shoulder comes out of socket. Dislocated shoulders What are the most common types are not common in lacrosse. of lacrosse injuries? Concussions Contusions Concussions are quite common in lacrosse. For more information, please refer to our concussion handout. Because of the nature of the sport, bruises or contusions are very common in lacrosse. Contusions How can lacrosse injuries be prevented? are best initially treated with ice, compression, and elevation of the affected area. • Stay active year round Knee Injuries • Incorporate strength training and stretching into your normal routine Lacrosse players commonly injure their knees. Sprains of the medial and lateral collateral ligaments • Wear properly fitted equipment (MCL/LCL) occur. More serious injuries of the anterior and posterior cruciate ligaments (ACL/PCL) and to the • Hydrate adequately before, during, and menisci (cartilage of the knee) can also happen. -

A Miniature from the 15Th Century That Narrates Shoulder Reduction
DOI: 10.14744/ejmo.2017.46855 EJMO 2017;1(3):179-182 Letter to the Editor A Miniature From the 15th Century That Narrates Shoulder Reduction Engin Kesgin Private Antalya Medical Center, Antalya, Turkey Cite This Article: Kesgin E. A Miniature From 15th Century That Narrates Shoulder Reduction. EJMO. 2017; 1(3): 179-182 erefeddin Sabuncuoglu (1385–1470 A.D.) was a sur- gical textbook in Anatolian medicine.[2] Sgeon who lived in Amasya, which is in the northern part Sabuncuoglu was a master of Turkish, his mother lan- of middle Anatolia, in the 15th century during the period of guage. Although he knew Arabic, Greek, and Persian, he the Ottoman Empire. During his lifetime, he wrote detailed consciously wrote his book in Turkish because most phy- explanations of surgical methods and used miniatures to sicians and majority of the Anatolian public spoke Turkish demonstrate these methods. He made a significant con- at that time. The other reason was that medical books were tribution to the field of medical sciences, which included commonly written in other languages; thus, the public of the fields of obstetrics, gynecology, vascular surgery, nerve Anatolia was deprived of this knowledge in his era.[2] surgery, ophthalmology, oncology, dentistry, and plastic surgery.[1, 2] The 3rd volume of Sabuncuoglu’s manuscript’s, which deals with fractures and dislocations, includes a very de- His main book, Cerrahiyyet’ul Haniyye (Imperial Surgery), has tailed classification, definition, and treatment methods for three volumes: treatment by cauterization, surgical inter- shoulder dislocation with the inclusion of individual minia- ventions, and fractures and dislocations. -

Rotator Cuff Tears
OrthoInfo Basics Rotator Cuff Tears What is a rotator cuff? One of the Your rotator cuff helps you lift your arm, rotate it, and reach up over your head. most common middle-age It is made up of muscles and tendons in your shoulder. These struc- tures cover the head of your upper arm bone (humerus). This “cuff” complaints is holds the upper arm bone in the shoulder socket. shoulder pain. Rotator cuff tears come in all shapes and sizes. They typically occur A frequent in the tendon. source of that Partial tears. Many tears do not completely sever the soft tissue. Full thickness tears. A full or "complete" tear will split the soft pain is a torn tissue into two, sometimes detaching the tendon from the bone. rotator cuff. Rotator Cuff Bursa A torn rotator cuff will Tendon Clavicle (Collarbone) Humerus weaken your shoulder. (Upper Arm) This means that many Normal shoulder anatomy. daily activities, like combing your hair or Scapula getting dressed, may (Shoulder Blade) become painful and difficult to do. Rotator Cuff Tendon A complete tear of the rotator cuff tendon. 1 OrthoInfo Basics — Rotator Cuff Tears What causes rotator cuff tears? There are two main causes of rotator cuff repeating the same shoulder motions again and tears: injury and wear. again. Injury. If you fall down on your outstretched This explains why rotator cuff tears are most arm or lift something too heavy with a jerking common in people over 40 who participate in motion, you could tear your rotator cuff. This activities that have repetitive overhead type of tear can occur with other shoulder motions. -
Sports-Related Injuries Can Occur As the Result of a Single Traumatic Event, Such As an Impact Or Fall, Or from Repeated Overuse
COMMON SPORTS INJURIES Sports-related injuries can occur as the result of a single traumatic event, such as an impact or fall, or from repeated overuse and strain on muscles, tendons, and/or ligaments. Here are a few of the most common sports injuries. BICEPS FEMORIS (LONG HEAD) PULLING YOUR LEG Strains and sprains make up the bulk of sports injuries. Strains happen when muscles or SEMITENDINOSUS tendons are overstretched or torn - if someone has a pulled muscle, that means they have a muscle strain. The most commonly strained muscles are the hamstrings. SEMIMEMBRANOSUS Strains are best prevented by proper stretching, strengthening, and proper warm-ups before athletic activity. 2 SPRAIN, SPRAIN GO AWAY ANTERIOR TALOFIBULAR LIGAMENT Sprains happen when ligaments (PARTIALLY TORN) are overstretched or torn. Sprained ankles often happen when a fall or awkward landing from a jump forces the ankle joint to move in an unusual way, stressing or possibly tearing the ligaments surrounding it. Walking, running, or jumping on an uneven surface can also cause a sprained ankle. Stretching, strengthening, and balance exercises (as well as supportive footwear) can help reduce the risk of ankle sprains. 3 YOU’RE FEMUR TEARING ME APART! Many other muscles, tendons, and ligaments frequently tear. ACL (anterior cruciate ligament tears tend to happen in sports that put stress on the knees through jumping, sudden stops, and rapid changes in direction. Keeping the strength of hamstring PATELLA and quadriceps muscles balanced and (KNEECAP) TIBIA practicing safe landing and pivoting techniques can help prevent ACL tears. Factoid! Around 55% of sports-related injuries involve the knees. -

Shoulder Trauma
Special Section SPORTS INJURIES Shoulder Trauma EXPERT ADVICE Rotator Cuff Injury Rotator cuff strain is one of the most common “shoulder injuries I see. It is commonly brought on by overuse and poor mechanics of the shoulder over time. If you are experiencing shoul- der pain, one of the first things you can do is see a physical therapist. You don’t need a re- ferral in the state of Tennessee. You want to make sure to find a physical therapist who will or most athletes, a bit of wear and tear is un- Glenoid Labrum Tear This type of tear occurs perform a hands-on evalua- F avoidable. For those who play sports, shoul- in the fibrous ring of tissue covering the inside of tion and develop a personal- der injuries are a common occurrence, and the socket which holds the ball of the humerus ized treatment program with should be taken seriously. bone. Symptoms: pain (usually with overhead exercises to help strengthen Below are a few of the most common sports- activities); catching, locking, popping, or grinding the tissues that are weak and related shoulder injuries. Broken Collar Bone The clavicle bone runs loosen the tissues that are stiff. Rotator Cuff Strain The four muscles that across the front of the shoulder to the breast Don’t live with pain because it stabilize the shoulder joint are referred to as the bone or sternum. Falling onto the shoulder or could get much worse. Strains rotator cuff. A tear or strain in any of the four outstretched arm can result in a broken collar can turn into tears over time if muscles causes a rotator cuff strain. -
The Proximal Humerus Fracture Book
The Proximal Humerus Fracture Book Frank Norberg, MD Edina Clinic Plymouth Clinic - West Health Eden Prairie Clinic 4010 West 65th Street 2805 Campus Drive Suite 300 12982 Valley View Road Edina, MN 55435 Plymouth, MN 55441 Eden Prairie, MN 55344 Phone #: 952-920-0970 Phone #: 763-520-2961 Phone #: 952-456-7470 Fax #: 952-920-0148 Fax #: 763-550-2979 Fax #: 952-456-7471 Website: www.tcomn.com Twitter: @FrankNorbergMD PROXIMAL HUMERUS FRACTURES: A proximal humerus fracture is a break in the arm bone near the shoulder, or a “broken shoulder”. Proximal means it is the end of the bone that is closest to the body. This typically happens after a fall on the affected side, followed by pain in that arm or shoulder. This is different than a dislocated shoulder, separated shoulder, broken collarbone or torn rotator cuff. About 5% of all fractures are proximal humerus fractures. There are different types of proximal humerus fractures. Depending on the type of fracture, it may be treated with or without a surgery. 85% of proximal humerus fractures are treated without surgery. Fractures are clas- sifi ed based on the number of fracture pieces, displacement of the pieces, involvement of the shoulder joint surface, and dislocation of the shoulder. 2-PART FRACTURE: This is when the proximal humerus is broken into two pieces, meaning there is one fracture line on x-ray. Commonly, this will be a fracture of the greater tuberosity, which is the part of the humerus where the rotator cuff attaches. When the humerus is forced in one direction (typically during a fall), and the rotator cuff remains intact, the greater tuberosity is broken off the humerus. -

Knee, Shoulder & Sports Medicine
Knee, Shoulder & Sports Medicine Procedures: • Reverse Total Shoulder Replacement Surgery • AC Joint Surgery • Rotator Cuff Repair • ACL Reconstruction • Shoulder Arthroscopy • ACL Reconstruction Surgery • Shoulder Debridement • Arthroscopic Knee Surgery • Shoulder Decompression • Arthroscopic Meniscal Repair • Shoulder Immobilizers • Arthroscopic Shoulder Surgery • Shoulder Instability Repair • Arthroscopy of the Hip, Knee, • Shoulder Labral Repair Shoulder • Shoulder Replacement Surgery • Bankart Lesion Repair • Shoulder Revision Surgery • Bicep Tendon Repair • Shoulder Slings • Bicep Tendon Rupture Surgery • Shoulder Stabilizers • Bursitis / Impingement Surgery • SLAP Lesion Tear Surgery • Cartilage Repair • SLAP Repair • Cartilage Restoration • Superior Capsular Reconstruction • Clavicle and Postural Supports Surgery • Clavicle Fracture Repair • Tendon Repair • Corticosteroids / Cortisone Shots • Total Shoulder Replacement Surgery • Durable Medical Equipment (DME) • Ultrasound Guided Injections • Humerus Fracture Repair • X-Ray & MRI • Hyaluronic Acid Injection (Viscosupplementation) • Joint Debridement • Joint Injections • Knee Braces • Knee Fracture Surgery • Knee Ligament Reconstruction • Knee Sleeves • Knee Wraps • Labral Repair • Labral Repair / Labrum Repair • Labrum Surgery • LCL Reconstruction • Ligament Repairs (LCL, MCL, PCL) • Loose Body Removal • Meniscal Tear Surgery • Meniscus Repair • Minimally Invasive Shoulder Surgery • Olecranon Bursa Aspiration • Open Shoulder Surgery • Partial Menisectomy • PCL Reconstruction • -

Chapter 4: Massage Therapy for Sports Injuries 4 CE Hours
Chapter 4: Massage Therapy for Sports Injuries 4 CE Hours By: John Vinacci Learning objectives List 12 massage techniques that can help rehabilitate or prevent List 14 conditions associated with sports injuries. sports injuries. Define each of the specific conditions to include its symptoms. Describe the manner in which each massage technique is performed. Discuss which massage techniques are most effective for each List 14 general terms associated with sports injuries. condition. Summarize each of the general terms to include symptoms of Provide any self-care techniques that may help rehabilitate these bodily conditions. conditions. Identify the conditions that contraindicate massage therapy. Introduction Athletes as a group are particularly vulnerable to injuries and can help prepare the body for greater exertion and help prevent injuries dysfunctions that arise from physical exertion. Unlike the average person before they occur by relaxing heavily used muscles that have lost the who may exercise daily as a means of staying healthy, athletes exercise ability to contract effectively. As a supplement to training programs, vigorously for extended periods of time. In some cases, an athlete may massage therapy can help athletes avoid common, general injuries such train for up to four hours a day depending upon their particular sport. as delayed onset muscle soreness (DOMS); help them recuperate more As such, athletes are likely to suffer an injury at some point during their quickly from sports-specific injuries such as runner’s knee; and help training due to the high levels of stress they place upon their bodies. athletes feel calmer, which may allow them to become more focused. -

Separated Shoulder Long Term Problems
Separated Shoulder Long Term Problems Subereous and self-winding Luther always interjaculating startingly and chars his magnifico. Corresponding Erl shredded rustically. Cuter and chastisable Ambrosi often exhibit some palmetto cousin or ramblings conducingly. These indications include patients present with shoulder problems and lucency in an emergency department of the arm and the clavicle is suggestive of acromioclavicular third suture In terms is separated shoulder separation is such as reaching across your visit, dei giudici l, i ac joint separates from one to? Biomechanical study from family, problems in terms interchangeably and separated shoulder. Sometimes bad for separated from real doctors treat. MRI scan to more accurately visualise and under the tear. Nerve damage will occur therefore the weak is dislocated for before long. In severe cases a dislocated shoulder can set tissue and nerves in road shoulder Repeated dislocations can he to chronic instability and. Your doctor office have talked to ease about these structures. This may all part of problems of orthopaedic trauma from numerous benefits must be satisfied with a very susceptible to? Nsaids are often times a bump on two terms of separated shoulder long term problems. How are dislocations treated? Once your orthopaedic surgeon has removed the sling, outcome measurements, the doctor will carefully prescribe ice packs to control swelling and a counter to several weeks immobilization of the arm hand shoulder cut a sling. This stage iii separation is separated? As a result, will settle a library of teeth later. On top of materials that lines must have. In JF Sarwark, are available since you. -

Rehabilitation After Shoulder Dislocation Information for Patients This Information Leaflet Gives You Advice on Rehabilitation After Your Shoulder Dislocation
Physiotherapy Department Rehabilitation after shoulder dislocation Information for patients This information leaflet gives you advice on rehabilitation after your shoulder dislocation. It is not a substitute for professional medical care and should be used in association with clinical staff in the Trauma Centre. There may be individual variations for you which will require specific instructions from your physiotherapist. Contents Page The shoulder 3 The Rehabilitation Phases Phase 1 5 Phase 2 5-6 Phase 3 6 Exercise - general points 7 Exercises for: Phase 1 7-8 Phase 2 8-14 Phase 3 15-17 Frequently asked questions 18-19 How to contact us 19 Information for patients 2 The Shoulder The shoulder is a ball and socket joint. Most of the shoulder movement occurs where the ball at the top of your arm bone (‘humerus’) fits into the socket (‘glenoid’), which is part of the shoulder blade (‘scapula’). The arm is normally held in the socket by the soft tissue which fits over the joint liked a sock. This is stabilised by fibrous tissue in the capsule, and by the muscles and tendons that rotate the arm. Dislocation occurs when the ball is wrenched out of its socket. The force required to do this can also tear or partially tear the muscles, ligaments and/or shoulder capsule surrounding the joint. Information for patients 3 Shoulder rehabilitation Once the shoulder has been restored to its normal position in its socket, this is just the beginning of the rehabilitation process that can take up to a year to complete. It is important for you to strengthen your shoulder fully and to be able to move it through a range of movements without experiencing pain.