Sight Loss in Older People the Essential Guide for General Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

College News October 2018
30 YEARS 1988 - 2018 QUARTERLY MAGAZINE OCTOBER EDITION 2018 Congratulations to this year’s Honorary Fellows, Professor Harminder Dua, Miss Marcia Zondervan and the diplomates receiving their award at the RCOphth Admissions Ceremony in September. PAGE 4 A SAS perspective Jugnoo Rahi Trainee Knowledge PAGE 6 New PAGE 15 New PAGE 18 How to to the NHS Chair, Academic mix research with subcommittee clinical training college news Dear fellow members, “Treating clinicians can lawfully choose Avastin for ophthalmic use on grounds of cost” Contents The 21st of September 2018 will live long in the memory of those who have campaigned 3 Awards galore! to be allowed to use Avastin (bevacizumab) 5 2018 Admissions as treatment for wet age-related macular Ceremony degeneration (ARMD). The landmark ruling by 6 New to the NHS - A Mrs Justice Whipple has brought clarity to the SAS Perspective interpretation of the national and European 7 Focus Managing legislation and should be read in full by all refractive surprise ophthalmologists. The College has issued a briefing note via Eye- 11 Museum Piece Mail to help answer some of the comments Births and Books in Whilst some may consider this a victory and concerns raised by members and I wish Ophthalmology 1818 over ‘Big Pharma’, we must not forget that members to continue to contribute to the 15 Jugnoo Rahi pharmaceutical companies are responsible discussions around Avastin. - New Academic for the development of the drugs we now use subcommittee chair to prevent blindness. It is essential that we Please do contact me at president@rcophth. 17 Ophthalmologists in recognise their vital role in eye health and ac.uk and I will do my best to answer your Training continue to work closely with them in future. -

UK Eye Care Services Project Phase One: Systematic Review of the Organisation of UK Eye Care Services
UK Eye Care Services Project Phase One: Systematic Review of the Organisation of UK Eye Care Services University of Warwick September 2010 (Revised February 2011) Dr Carol Hawley Helen Albrow Dr Jackie Sturt Lynda Mason UK Eye Care Services Project Contents Phase One: Systematic Review of the Organisation of UK Eye Care Services Study team i Acknowledgements i Glossary of abbreviations ii Executive Summary 1 1. Background to current organisation of UK eye care services 4 Devolution in Scotland and Wales 6 Global thinking surrounding eye care services and the UK response 8 Other ophthalmic roles 9 Generalisability of care pathways 11 Report Aim 11 2. Methods 12 2.1 Data searches 12 2.2 Data Extraction 14 3. Results 15 3.1 Report organisation 15 3.2 Summary of ‘black’ literature 17 Optometrists in primary care 18 Optometrists within the HES 19 Combined eye examination and referral initiatives for all eye conditions 22 Referral initiatives for all eye conditions 23 Referral quality and frequencies for all eye conditions 25 Glaucoma 28 Ocular Hypertension (OHT) 40 Cataract 41 Posterior Capsular Opacification 47 Diabetic Retinopathy (DR) 49 Blood Glucose screening 60 Optometric Prescribing 61 Low Vision Services 64 Paediatric eye care services 67 Melanoma 71 Flashes and floaters 72 Critique of the COSI concept (Community Optometrists with a Special Interest) 74 Optometric technological comparison studies 75 4. Conclusions from the literature 76 5. References 78 UK Eye Care Services Project Appendices Phase One: Systematic Review of the Organisation -

Crafting Alliances
05-Wei-45241.qxd 2/14/2007 5:16 PM Page 191 CHAPTER 5 Crafting Alliances egardless of how successful a social enterprise is at mobilizing funds, most R organizations will inevitably face resource and capacity constraints as a limiting factor to achieving their mission. The resources that any single organi- zation brings to bear on a social problem are often dwarfed by the magnitude and complexity of most social problems. Thus, social entrepreneurs often pursue alliance approaches as a means to mobilizing resources, financial and nonfinan- cial, from the larger context and beyond their own organizational boundaries, to achieve increased mission impact. Social enterprise alliances among nonprofits, nonprofits and business, nonprofits and government, and even across all sectors in the form of tripartite alliances between nonprofit, government, and business have become increasingly common in recent years. Because alliances capitalize on the resources and capacities of more than one organization and capture syn- ergies that would otherwise often go unrealized, they have the potential to gen- erate mission impact far beyond what the individual contributors could achieve independently. This chapter first describes some alliance trends in the social sec- tor and illustrates them with case examples. Next, we introduce a conceptual framework that can be helpful for developing an alliance strategy. Finally, we briefly introduce the chapter’s two case studies, which offer readers an opportu- nity for in-depth analysis of a range of alliance approaches. ALLIANCE TRENDS Increased Competition Increased competition due to a growing number of nonprofits coupled with recent overall declines in social sector funding have contributed to a dramatic 191 05-Wei-45241.qxd 2/14/2007 5:16 PM Page 192 192 Entrepreneurship in the Social Sector increase in the number and form of social enterprise alliances. -
Fight for Sight Is the UK's Largest Charity Funding Pioneering Eye
Fight for Sight is the UK’s largest charity funding pioneering eye research since 1965. Our mission Fight for Sight funds pioneering research to prevent sight loss and treat eye disease. Our vision A future everyone can see. Fight£3.3m for Sight committed to research in 2017/18 Fight£8m for Sight commitment to active research projects Number of active research projects 166 Number of funded institutions 49 5 49 49 2 49 7 49 3 49 3 49 2 49 7 49 1 49 10 49 5 49 4 Numbers of patients in clinical studies funded by Fight for Sight Number16,230 of patients Number87 of studies recruited into NIHR on the NIHR CRN supported studies funded portfolio funded partly partly or wholly by or wholly by Fight for Sight Fight for Sight between between April 2008 April 2008 and and January 2018 January 2018 Number71 of sites Number23 of studies from which NIHR has open on the NIHR recruited participants for CRN portfolio studies funded partly or funded partly or wholly wholly by Fight for Sight by Fight for Sight between April 2008 as of January 2018 and January 2018 National Institute for Health Research (NIHR) Clinical Research Network (CRN) Charity partners Fight for Sight is very pleased to be collaborating with other charities in the sector. Fight for Sight is the UK’s largest charity funding pioneering eye research since 1965. Estimated prevalence of main eye diseases in the UK Age-related macular degeneration 600,000 people Glaucoma 500,000 people Cataract 500,000 people Diabetic retinopathy 144,000 people How many people fear losing their sight? of25% the adult population are not having an eye test of people78% stated every 2E years. -

Eye Research Charity Looking for Pioneering Researchers in Scotland Fight for Sight Partners with Chief Scientist Office to Fund Research in Scotland
Immediate release Eye research charity looking for pioneering researchers in Scotland Fight for Sight partners with Chief Scientist Office to fund research in Scotland Fight for Sight, the UK’s leading eye research charity, has partnered with the Scottish Government’s Chief Scientist Office (CSO) to help address age-related eye diseases. The charity is calling for research applications from Scottish based researchers for a grant of up to £200,000 for up to three years. The grant will support research to help address age- related eye diseases and conditions as well as projects focusing on the association of visual impairment with other long-term conditions, such as dementia, stroke or diabetes. The closing date for Fight for Sight/ CSO Project grant applications is 5pm on 1 November 2017. Supporting Quote: Dr Alan McNair, Senior Research Manager at the Scottish Government Chief Scientist Office “CSO is delighted to partner with Fight for Sight in this exciting research funding initiative. Age related eye diseases can severely impact patients and those close to them. Research is essential if we are to develop a better understanding of the impact of these conditions and develop effective new treatments”. Michele Acton, Chief Executive of Fight for Sight “It is only through funding eye research that we will be able to address age-related sight loss. Partnering with the CSO will bring us closer to our goals to the benefit of people in Scotland and worldwide.” Online Resources: W: http://www.fightforsight.org.uk/apply-for-funding/funding-opportunities/fight-for-sight-cso- project-grant/ T: @fightforsightUK F: https://www.facebook.com/fightforsightuk ENDS About Fight for Sight 1. -
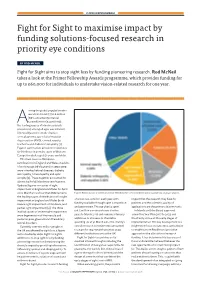
Fight for Sight to Maximise Impact by Funding Solutions-Focused Research in Priority Eye Conditions
25 YEARS IN OPHTHALMOLOGY Fight for Sight to maximise impact by funding solutions-focused research in priority eye conditions BY ROD MCNEIL Fight for Sight aims to stop sight loss by funding pioneering research. Rod McNeil takes a look at the Primer Fellowship Awards programme, which provides funding for up to £60,000 for individuals to undertake vision-related research for one year. mong the global population who were blind in 2015 (36.0 million [80% uncertainty interval A12·9 million to 65.4 million]), the leading causes of blindness (crude prevalence) among all ages was cataract, followed by uncorrected refractive error, glaucoma, age-related macular degeneration (AMD), corneal opacity, trachoma and diabetic retinopathy [1]. Figure 1 summarises prevalence estimates for blindness in 2015 by cause in Western Europe for adults aged 50 years and older. The main causes of blindness certifications in England and Wales in adults of working age (16-64 years) in 2009-2010 were inherited retinal diseases, diabetic retinopathy / maculopathy and optic atrophy [2]. These together accounted for almost half of all blindness certifications. Updated figures on causes of sight impairment in England and Wales for April 2012-March 2013 show that AMD remains Figure 1: Western Europe: projected prevalence of blindness (VA <3/60 in the better eye) by cause among adults ≥50 years [1]. the leading cause of certifications for sight of around £3-4 million each year, with impact that the research may have for impairment in England and Wales (both funding available through open competition patients and the scientific quality of severe sight impairment or blindness, and partial sight impairment) [3]. -

Causes of Vision Loss Worldwide, 1990€“2010: a Systematic Analysis
Articles Causes of vision loss worldwide, 1990–2010: a systematic analysis Rupert R A Bourne*, Gretchen A Stevens*, Richard A White, Jennifer L Smith, Seth R Flaxman, Holly Price, Jost B Jonas, Jill Keeff e†, Janet Leasher†, Kovin Naidoo†, Konrad Pesudovs†, Serge Resnikoff †, Hugh R Taylor†, on behalf of the Vision Loss Expert Group Summary Background Data on causes of vision impairment and blindness are important for development of public health Lancet Glob Health 2013; policies, but comprehensive analysis of change in prevalence over time is lacking. 1: e339–49 Published Online Methods We did a systematic analysis of published and unpublished data on the causes of blindness (visual acuity in November 11, 2013 http://dx.doi.org/10.1016/ the better eye less than 3/60) and moderate and severe vision impairment ([MSVI] visual acuity in the better eye less S2214-109X(13)70113-X than 6/18 but at least 3/60) from 1980 to 2012. We estimated the proportions of overall vision impairment attributable See Comment page e311 to cataract, glaucoma, macular degeneration, diabetic retinopathy, trachoma, and uncorrected refractive error in Copyright © Bourne et al. Open 1990–2010 by age, geographical region, and year. Access article distributed under the terms of CC BY Findings In 2010, 65% (95% uncertainty interval [UI] 61–68) of 32·4 million blind people and 76% (73–79) of *RRAB and GAS contributed 191 million people with MSVI worldwide had a preventable or treatable cause, compared with 68% (95% UI 65–70) of equally to writing of the paper 31·8 million and 80% (78–83) of 172 million in 1990. -
Sight Loss and Vision Priority Setting Partnership
Sight Loss and Vision Priority Setting Partnership Setting Priorities for Eye Research Final Report www.sightlosspsp.org.uk October 2013 Acknowledgements Contents Partners Forewords 4 The following organisations provided funding Earl Howe, Parliamentary Under Secretary of and/or in-kind support for this initiative: State for Quality at the Department of Health College of Optometrists Professor Ruairidh Milne, Head of NIHR Evaluation, Trials and Studies Co-ordinating Centre Fight for Sight James Lind Alliance Executive summary 6 NIHR Moorfields BRC Introduction RNIB Methodology Royal College of Ophthamologists Results UK Vision Strategy Next steps Introduction 8 Why set priorities for eye research? Background James Lind Alliance Limitations Methodology 12 Flowchart of the process Establishing the Sight Loss and Vision Priority Setting Partnership survey Data assessment Interim prioritisation Final prioritisation Results 18 Next Steps 36 Working with: How to get involved Disclosures 38 References 39 Appendices 40 2 Sight Loss and Vision Priority Setting Partnership Sight Loss and Vision Priority Setting Partnership 3 Forewords Foreword by Earl Howe Foreword by Professor Ruairidh Milne Sight is the sense that most people fear losing the most and Earlier this year we were delighted to complete the transfer any loss or impairment can reduce a person’s quality of life of the James Lind Alliance (JLA) to the NIHR Evaluation, substantially. Sight loss affects adults and children and as we Trials and Studies Coordinating Centre (NETSCC). The JLA live longer the number of people affected will increase. Priority Setting Partnerships bring together patients, relatives, carers and health professionals to identify priorities for Encouraging people’s awareness of eye health and improving the research. -

Annual Report 2012
THE ROYAL COLLEGE OF OPHTHALMOLOGISTS ANNUAL REPORT 2012 Eye doctors setting the standards for patients - 1 - THE ROYAL COLLEGE OF OPHTHALMOLOGISTS Eye Doctors setting the standards for patients Welcome to the 2012 Annual Report of The Royal College of Ophthalmologists. We are always keen to hear from ophthalmologists who would like to join the College, from members who would like to participate more fully in College activities and from members of the general public who wish to support the College with donations to the Research Fund or the John Lee Fellowship. Do please email the Chief Executive, Kathy Evans by using our Contact Form. ANNUAL REPORT 2012 Contents The President 4 The Chief Executive 6 The Strategic Plan 8 The Professional Standards Committee 11 The Scientific Committee 18 The Education Committee 22 The Training Committee 28 The Examinations Committee 32 The Academic Group 34 The International Subcommittee 35 The European Subcommittee 36 The Staff and Associate Specialist Ophthalmologists’ Group 38 The Ophthalmic Trainees’ Group 41 The Lay Advisory Group 43 The Equality and Diversity Committee 45 The Museum and Library 47 - 2 - The Honorary Secretary 48 The Honorary Treasurer 56 The Auditors’ Report 58 Statement of Financial Activities 60 Balance Sheet 61 - 3 - THE PRESIDENT Professor Harminder Dua ‘Time flies when you are having fun’, whoever said that for the first time must have felt exactly like I have felt over the last year. ‘There has never been a dull moment’, to borrow another phrase. Writing the president’s piece for the annual report provides me with the opportunity to reflect on the bygone year, dwell on the job at hand and look ahead. -

A World Everyone Can
A WORLD EVERYONE CAN SEE Restoring sight through revolutionary science Research Strategy 2017 - 2022 Fight for Sight Research Strategy 2017 - 2022 Background It is estimated that there are two million people in the UK living with sight loss1 that affects their daily lives. For half of these people, their sight loss is avoidable, primarily by getting an eye test and a prescription for glasses or contact lenses. For the other half it is not so straightforward. There are many different eye diseases and conditions that we cannot currently prevent, treat or reverse the sight loss that they cause. Our Vision and our Goals Fight for Sight’s vision is simple. We believe in a future everyone can see. We want to stop sight loss. To meet our aim of stopping sight loss, our goals are to: 1) Increase understanding of how eye diseases and conditions start and develop; 2) Prevent eye diseases and conditions; 3) Enable eye diseases and conditions to be detected earlier; 4) Develop new and improved treatments for eye diseases and conditions; 5) Improve the public’s understanding of how to reduce the risk of sight loss; and 6) Provide information to people affected by sight loss. Delivering Our Goals Fight for Sight’s primary way of delivering its goals is through funding the highest quality medical research. We enhance our impact by considering new and innovative solutions for patients, providing information, influencing opinion and shaping policy. Where possible, we work collaboratively to develop innovative partnerships to maximise opportunities to meet our long term goals. The Eye Research Landscape Eye disease is a significantly under-funded area of research in the UK. -

A Minimum Job Description Is Described Below
ACF Ophthalmology Job Description HENW (Mersey) Academic Clinical Fellow – Ophthalmology ST1, 2 or 3 1. Job title Academic Clinical Fellow in Ophthalmology 2. Duration of post, and what happens at the end of the post if candidate successful or unsuccessful in obtaining a research fellowship The ACF post will be for up to 3 years and during this time the fellow will be expected to apply to an external funding agency such as MRC, Wellcome Trust, Fight for Sight or other charities and organisations for a Clinical Research Training Fellowship. If successful in obtaining such a fellowship, the postholder will study for a MD or PhD and then potentially progress to a Clinical Lecturer post within The Mersey Deanery. If applications for a Clinical Research Training Fellowship or any alternative source of funding to complete a MD or PhD are unsuccessful, the post- holder will return to the Specialist Trainee programme in The Mersey Deanery, providing clinical aspects of training are progressing satisfactorily (as monitored by ARCPs etc). 3. Confirmation that the post attracts an NTN (a) Yes 4. Hospitals in which training will take place Clinical training during the 3 year ACF component will take place predominantly within St Paul’s Eye Unit at The Royal Liverpool and Broadgreen University University Hospitals NHS Trust. Given the research content of the post and the particular need to be in close proximity to the University, it is expected that the Academic Clinical Fellow, will fulfil most of their training requirements within the Royal Liverpool University Hospital. Outside rotation is however, expected, but will depend on specific training needs, for example, paediatric Ophthalmology at Alder Hey Childrens NHS Trust Hospital or oculoplastics and neuro-ophthalmology at Aintree University Hospital. -
Sight Loss and Vision Priority Setting Partnership
Sight Loss and Vision Priority Setting Partnership Setting Priorities for Eye Research Executive Summary www.sightlosspsp.org.uk October 2013 The full report is available at www.sightlosspsp.org.uk Introduction Methodology Despite on-going research activity in the UK and worldwide, A survey collected unanswered questions about the prevention, there are still many questions about the prevention, diagnosis diagnosis and treatment of sight loss and eye conditions from and treatment of sight loss and eye conditions that remain patients, relatives, carers and eye health professionals. unanswered. Funding for research is limited, so it is important for research funders to understand the unanswered questions The questions were analysed, formatted and categorised into of greatest importance to patients, carers and eye health disease specific groups. Searches were then undertaken to professionals so that future research can be consolidated and ascertain whether or not each question could be answered targeted accordingly. by an up-to-date systematic review, those which could were then removed. All unanswered questions were allocated The Sight Loss and Vision Priority Setting Partnership (PSP) has to 12 different eye disease/condition categories and similar captured these vital views to identify what research into sight or duplicate submissions were combined. loss and eye conditions should be addressing. It is rare that those with direct experience of conditions are able to influence A series of interim prioritisation exercises was conducted the research agenda. to reduce the number of questions for categories which had a large number of submissions. This resulted in a shortlist The Sight Loss and Vision PSP was overseen by the James Lind of questions for each category.