Colonoscopy Through the Stoma – a Patient’S Perspective
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -
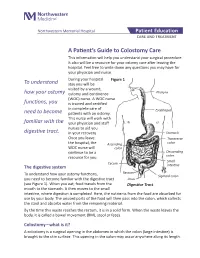
A Patient's Guide to Colostomy Care
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -

42 CFR Ch. IV (10–1–12 Edition) § 410.35
§ 410.35 42 CFR Ch. IV (10–1–12 Edition) the last screening mammography was (1) Colorectal cancer screening tests performed. means any of the following procedures furnished to an individual for the pur- [59 FR 49833, Sept. 30, 1994, as amended at 60 FR 14224, Mar. 16, 1995; 60 FR 63176, Dec. 8, pose of early detection of colorectal 1995; 62 FR 59100, Oct. 31, 1997; 63 FR 4596, cancer: Jan. 30, 1998] (i) Screening fecal-occult blood tests. (ii) Screening flexible § 410.35 X-ray therapy and other radi- sigmoidoscopies. ation therapy services: Scope. (iii) In the case of an individual at Medicare Part B pays for X-ray ther- high risk for colorectal cancer, screen- apy and other radiation therapy serv- ing colonoscopies. ices, including radium therapy and ra- (iv) Screening barium enemas. dioactive isotope therapy, and mate- (v) Other tests or procedures estab- rials and the services of technicians ad- lished by a national coverage deter- ministering the treatment. mination, and modifications to tests [51 FR 41339, Nov. 14, 1986. Redesignated at 55 under this paragraph, with such fre- FR 53522, Dec. 31, 1990] quency and payment limits as CMS de- termines appropriate, in consultation § 410.36 Medical supplies, appliances, with appropriate organizations and devices: Scope. (2) Screening fecal-occult blood test (a) Medicare Part B pays for the fol- means— lowing medical supplies, appliances (i) A guaiac-based test for peroxidase and devices: activity, testing two samples from (1) Surgical dressings, and splints, each of three consecutive stools, or, casts, and other devices used for reduc- (ii) Other tests as determined by the tion of fractures and dislocations. -

Double Barrel Wet Colostomy for Urinary and Fecal Diversion
Open Access Clinical Image J Urol Nephrol November 2017 Vol.:4, Issue:2 © All rights are reserved by Kang,et al. Journal of Double Barrel Wet Colostomy for Urology & Urinary and Fecal Diversion Nephrology Yu-Hao Xue and Chih-Hsiung Kang* Keywords: Double barrel wet colostomy; Urinary diversion; Fecal Department of Urology, Chang Gung Memorial Hospital-Kaohsiung diversion Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan, Republic of China Abstract Address for Correspondence A 60-year-old male who had a history of spinal cord injury received Chih-Hsiung Kang, Department of Urology, Chang Gung Memorial loop colostomy for fecal diversion and cystostomy for urinary diversion. Hospital - Kaohsiung Medical Center, Chang Gung University College Because he was diagnosed with muscle invasive bladder cancer, of Medicine, Taiwan, E- mail: [email protected] radical cystectomy and double barrel wet colostomy was conducted. Submission: 30 October, 2017 Computed tomography showed simultaneous urinary and fecal Accepted: 06 November, 2017 diversion and stone formation in the distal segment of colon conduit Published: 10 November, 2017 with urinary diversion. Copyright: © 2017 Kang CH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, Introduction provided the original work is properly cited. In patients with an advanced primary or recurrent carcinoma, double-barreled wet colostomy can be used for pelvic exenteration Bilateral hydroureters and mild hydronephrosis were noted and and urinary tract reconstruction. It is a technique that separate we suspected the calculi impacted in bilateral ureteto-colostomy urinary and fecal diversion with a single abdominal stoma. -

The Costs and Benefits of Moving to the ICD-10 Code Sets
CHILDREN AND ADOLESCENTS This PDF document was made available from www.rand.org as a public CIVIL JUSTICE service of the RAND Corporation. EDUCATION ENERGY AND ENVIRONMENT Jump down to document HEALTH AND HEALTH CARE 6 INTERNATIONAL AFFAIRS POPULATION AND AGING The RAND Corporation is a nonprofit research PUBLIC SAFETY SCIENCE AND TECHNOLOGY organization providing objective analysis and effective SUBSTANCE ABUSE solutions that address the challenges facing the public TERRORISM AND HOMELAND SECURITY and private sectors around the world. TRANSPORTATION AND INFRASTRUCTURE U.S. NATIONAL SECURITY Support RAND Purchase this document Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore RAND Science and Technology View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. This product is part of the RAND Corporation technical report series. Reports may include research findings on a specific topic that is limited in scope; present discus- sions of the methodology employed in research; provide literature reviews, survey instruments, modeling exercises, guidelines for practitioners and research profes- sionals, and supporting documentation; -

Abdominoperineal Excision of the Rectum Information
Abdominoperineal excision of the rectum Information Introduction Your consultant has recommended an abdominoperineal resection of the rectum because you require the removal of your rectum. A member of staff will explain everything in this leaflet to you, but if you have any questions, please ask us. The rectum (see Figure 1) is the storage organ at the end of the bowel and the anal canal is the exit from the bowel (the back passage). for patients Figure 1: the rectum and anal canal Figure 2: a colostomy What is an abdominoperineal excision of the rectum? Abdominoperineal excision of the rectum (often referred to as an AP or APER) is an operation to remove the rectum and anal canal. This will close the anus completely and permanently. A colostomy (stoma) is formed to enable you to empty your bowels (see Figure 2). The colostomy is the bowel, which is brought through a small opening on your abdomen. The faeces are collected into a colostomy appliance, which will adhere to your abdominal wall. The operation is performed by making several small keyhole cuts or a big abdominal incision (cut). There is also an incision around the anus, so that after the operation you will have several small scars or a long scar and a stoma on your abdomen and a scar between your buttocks where the anus has been closed. You will meet a stoma specialist nurse before your operation to discuss living with a colostomy. This can either be arranged at St Mark’s Hospital or you may like to meet your local stoma care nurse who will be helping you once you go home from hospital. -

Patient Education Series Managing Your Colostomy Colostomybooklet 8/6/2005 12:12 Page 1
Patient Education Series Managing Your Colostomy ColostomyBooklet 8/6/2005 12:12 Page 1 Table of contents About your colostomy • The human digestive system . 1 About your • What is a colostomy? . 3 colostomy •Types of colostomies . 4 • Three types of stoma constructions . 5 Every year, thousands of people have colostomy surgery. For some, the surgery is a lifesaving Colostomy pouching systems procedure. For others, the surgery relieves years of suffering from • One-piece system . 6 bowel disease. Whatever the •Two-piece system. 6 medical reason, anyone who is going to have colostomy surgery •Drainable pouch . 6 has many questions and concerns. •Closed pouch. 7 The purpose of this booklet is to • Irrigation . 7 answer some of your questions about colostomy surgery and to ease some of your concerns about Lifestyle living with a colostomy. It will help you manage and understand your • Skin care . 7 colostomy. It is important to • Diet . 8 remember that you are not alone. • Odour. 8 This booklet is provided to you by your health care team and • Gas. 9 supplements other information • Diarrhoea. 10 given to you by your doctor and ET nurse – a nurse who •Alcohol. 10 specialises in ostomy care. •Medication. 11 Remember to write down your questions and discuss these with • Bathing or showering . 11 your doctor or ET nurse. • Clothing . 11 • Returning to work and travelling. 12 • Exercise and sports . 12 Your ET nurse: •Sex and personal relationships . 12 .................................................. • Religion . 13 Contact numbers: • Routine care of your colostomy . 14 .................................................. .................................................. Glossary . 16 1 ColostomyBooklet 8/6/2005 12:12 Page 2 Oesophagus Stomach Colon Small Intestine Rectum Anus The human digestive system When you chew your food and swallow it, your food goes down your oesophagus into your stomach. -

FY 2009 Final Addenda ICD-9-CM Volume 3, Procedures Effective October 1, 2008
FY 2009 Final Addenda ICD-9-CM Volume 3, Procedures Effective October 1, 2008 Tabular 00.3 Computer assisted surgery [CAS] Add inclusion term That without the use of robotic(s) technology Add exclusion term Excludes: robotic assisted procedures (17.41-17.49) New code 00.49 SuperSaturated oxygen therapy Aqueous oxygen (AO) therapy SSO2 SuperOxygenation infusion therapy Code also any: injection or infusion of thrombolytic agent (99.10) insertion of coronary artery stent(s) (36.06-36.07) intracoronary artery thrombolytic infusion (36.04) number of vascular stents inserted (00.45-00.48) number of vessels treated (00.40-00.43) open chest coronary artery angioplasty (36.03) other removal of coronary obstruction (36.09) percutaneous transluminal coronary angioplasty [PTCA] (00.66) procedure on vessel bifurcation (00.44) Excludes: other oxygen enrichment (93.96) other perfusion (39.97) New Code 00.58 Insertion of intra-aneurysm sac pressure monitoring device (intraoperative) Insertion of pressure sensor during endovascular repair of abdominal or thoracic aortic aneurysm(s) New code 00.59 Intravascular pressure measurement of coronary arteries Includes: fractional flow reserve (FFR) Code also any synchronous diagnostic or therapeutic procedures Excludes: intravascular pressure measurement of intrathoracic arteries (00.67) 00.66 Percutaneous transluminal coronary angioplasty [PTCA] or coronary atherectomy Add code also note Code also any: SuperSaturated oxygen therapy (00.49) 1 New code 00.67 Intravascular pressure measurement of intrathoracic -

Development of the ICD-10 Procedure Coding System (ICD-10-PCS)
Development of the ICD-10 Procedure Coding System (ICD-10-PCS) Richard F. Averill, M.S., Robert L. Mullin, M.D., Barbara A. Steinbeck, RHIT, Norbert I. Goldfield, M.D, Thelma M. Grant, RHIA, Rhonda R. Butler, CCS, CCS-P The International Classification of Diseases 10th Revision Procedure Coding System (ICD-10-PCS) has been developed as a replacement for Volume 3 of the International Classification of Diseases 9th Revision (ICD-9-CM). The development of ICD-10-PCS was funded by the U.S. Centers for Medicare and Medicaid Services (CMS).1 ICD-10- PCS has a multiaxial seven character alphanumeric code structure that provides a unique code for all substantially different procedures, and allows new procedures to be easily incorporated as new codes. ICD10-PCS was under development for over five years. The initial draft was formally tested and evaluated by an independent contractor; the final version was released in the Spring of 1998, with annual updates since the final release. The design, development and testing of ICD-10-PCS are discussed. Introduction Volume 3 of the International Classification of Diseases 9th Revision Clinical Modification (ICD-9-CM) has been used in the U.S. for the reporting of inpatient pro- cedures since 1979. The structure of Volume 3 of ICD-9-CM has not allowed new procedures associated with rapidly changing technology to be effectively incorporated as new codes. As a result, in 1992 the U.S. Centers for Medicare and Medicaid Services (CMS) funded a project to design a replacement for Volume 3 of ICD-9-CM. -

Ascrs Position Statement on Preoperative Stoma Site Marking for Patients Undergoing Colostomy Or Ileostomy Surgery
WOCN SOCIETY AND ASCRS POSITION STATEMENT ON PREOPERATIVE STOMA SITE MARKING FOR PATIENTS UNDERGOING COLOSTOMY OR ILEOSTOMY SURGERY WOCN Society and ASCRS Position Statement on Preoperative Stoma Site Marking for Patients Undergoing Colostomy or Ileostomy Surgery Originated By: Wound, Ostomy and Continence Nurses Society’s (WOCN®) Stoma Site Marking Task Force in collaboration with the American Society of Colon and Rectal Surgeons (ASCRS) in 2007.1 Updated/Revised By: WOCN Society’s Stoma Site Marking Task Force in collaboration with the ASCRS and the American Urological Association (AUA). Contributing Authors: Task Force Chair • Ginger Salvadalena, PhD, RN, CWOCN, Principal Scientist, Global Clinical Affairs, Hollister Incorporated, Libertyville, Illinois Task Force Members • Samantha Hendren, MD, MPH, Associate Professor of Surgery, University of Michigan, Ann Arbor, Michigan • Linda McKenna, MSN, RN, CWOCN, Ostomy & Wound Specialist, Memorial Medical Center, Springfield, Illinois • Roberta Muldoon, MD, FACS, Assistant Professor of Surgery, Vanderbilt University Medical Center, Nashville, Tennessee • Debra Netsch, DNP, RN, CNP, FNP-BC, CWOCN, Mankato Clinic, Ltd, Mankato, Minnesota • Ian Paquette, MD, Assistant Professor of Surgery, University of Cincinnati College of Medicine, Cincinnati, Ohio • Joyce Pittman, PhD, ANP-BC, FNP-BC, CWOCN, Team Lead Wound/Ostomy Adjunct Assistant Professor, Indiana University School of Nursing, Indiana University Health-Methodist, Indianapolis, Indiana • Janet Ramundo, MSN, RN, CWOCN, WOC Nurse, Houston Methodist Hospital, Houston, Texas • Gary Steinberg, MD, The Beth and Bruce White Family Professor and Director of Urologic Oncology; Vice Chairman Section of Urology, The University of Chicago Medicine, Chicago, Illinois TM Wound, Ostomy and Continence Nurses Society (WOCN®) 2 Date Completed: June 2014 Date Approved by the WOCN Board of Directors: November 12, 2014 The WOCN Society suggests the following format for bibliographic citations: Wound, Ostomy and Continence Nurses Society. -

A Simple Test to Predict Faecal Continence Before Colostomy Closure M Brand, G J Oettle
SAJS General Surgery The dynamic continence challenge – a simple test to predict faecal continence before colostomy closure M Brand, G J Oettle Department of Surgery, University of the Witwatersrand, Johannesburg M Brand, MB ChB, FCS (SA), MRCS, MMed (Surg) G J Oettle, MB BCh, FRCS (Edin) Corresponding author: M Brand ([email protected]) Background. A common problem in clinical practice is predicting whether a patient will be continent after treatment of a severe perineal injury. Several tests have been described. Anal manometry is unreliable; continence can be normal with low pressures, and poor with high or normal pressures. Endo-anal ultrasound only illustrates anatomical sphincter integrity. The saline continence test involves the quite unphysiological instilling of saline into the rectum, and assessing seepage. What is needed in the prediction of continence is a normal stool simulator. Method. We propose the use of powdered instant mashed potato reconstituted with water to the consistency of faeces. About 100 - 150 ml is introduced into the rectum using a catheter-tipped syringe. The patient is instructed to walk around for half an hour. On return the underwear is examined for any soiling. If there is no leakage the colostomy may be reversed. Results. Over the past 15 years, 53 patients have undergone this test. In 47 patients there was no leakage, all had their stomas reversed, and none was incontinent during follow-up. Conclusion. The dynamic continence challenge is an accurate physiological test that allows clinicians to simulate the effects of colostomy reversal and assess a patient’s continence before actually proceeding to the reversal. -

Appendix 1: Emergency General Surgical Core Procedures* *Based on Shafi Et Al
Appendix 1: Emergency general surgical core procedures* *Based on Shafi et al. Journal of Trauma Gastrointestinal Stomach Incision, Excision 43500-43641 Laparoscopy Diagnostic 49230 Other Gastrojejunostomy 43830 Repair Perforated Gastric / Duodenal Ulcer 43840 Splenectomy, Open 38100 Splenorrhaphy 38115 Repair Paraesophageal / Diaphragmatic hernia 39502 Exploratory Laparotomy 49000 Excision Meckel’s Diverticulum 44800 Small Bowel Resection, Anastomosis 44120 Small Bowel Resection, Enterostomy 44125 Appendectomy 44950 Appendectomy, Drainage Abscess 44960 Exploratory Laparoscopy – with/without Biopsies 49321 Appendectomy, Laparoscopic 44970 Gastrotomy 43500 Gastrojejunostomy 43820 Suture Repair Bleeding Ulcer 43501 Gastric Wedge Resection 43610 Hemi-Gastrectomy with/out Vagotomy 43632, 43635 Total Gastrectomy 43621 Vagotomy and Pyloroplasty 43640 Highly Selective Vagotomy 43641 Repair Perforated Gastric / Duodenal Ulcer 43840 Enterolysis (Lysis of Adhesions) 44005 Reduction Intussusecption 44050 Inguinal – Adult 49505 Inguinal Hernia, Laparoscopic – Adult 49650 Umbilical – Adult 49585 Femoral 49550 Ventral – Incisional – Initial/Recurrent 49560, 49565 Remove Infected Abdominal Mesh 11008 Repair Paraesophageal / Diaphragmatic hernia 39502 Colectomy, Anastomosis 44140 Partial Colectomy, Colostomy (Hartmann) 44143 Creation Enterostomy (Jejunostomy or Ileostomy) 44310 Creation Colostomy 44320 Debride or Excise Perineal Infection 11004 Excision Pilonidal Cyst / Sinus 11771 Drainage Intra-Abdominal Abscess (Not Appendiceal) 49020 Repair Complex