Abdominoperineal Resection of Rectum Consent Rectum of Resection Abdominoperineal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Continent Urostomy Guide
$POUJOFOU6SPTUPNZ(VJEF "QVCMJDBUJPOPGUIF6OJUFE0TUPNZ"TTPDJBUJPOTPG"NFSJDB *OD i4FJ[FUIF 0QQPSUVOJUZw CONTINENT UROSTOMY GUIDE Ilene Fleischer, MSN, RN, CWOCN, Author Patti Wise, BSN, RN, CWOCN, Author Reviewed by: Authors and Victoria A.Weaver, RN, MSN, CETN Revised 2009 by Barbara J. Hocevar, BSN,RN,CWOCN, Manager, ET/WOC Nursing, Cleveland Clinic © 1985 Ilene Fleischer and Patti Wise This guidebook is available for free, in electronic form, from United Ostomy Associations of America (UOAA). UOAA may be contacted at: www.ostomy.org • [email protected] • 800-826-0826 CONTENTS INTRODUCTION . 3 WHAT IS A CONTINENT UROSTOMY? . 4 THE URINARY TRACT . 4 BEFORE THE SURGERY . .5 THE SURGERY . .5 THE STOMA . 7 AFTER THE SURGERY . 7 Irrigation of the catheter(s) 8 Care of the drainage receptacles 9 Care of the stoma 9 Other important information 10 ROUTINE CARE AT HOME . 10 Catheterization schedule 11 How to catheterize your pouch 11 Special considerations when catheterizing 11 Care of the catheter 12 Other routine care 12 HELPFUL HINTS . .13 SUPPLIES FOR YOUR CONTINENT UROSTOMY . 14 LIFE WITH YOUR CONTINENT UROSTOMY . 15 Clothing 15 Diet 15 Activity and exercise 15 Work 16 Travel 16 Telling others 17 Social relationships 17 Sexual relations and intimacy 17 RESOURCES . .19 GLOSSARY OF TERMS . 20 BIBLIOGRAPHY . .21 1 INTRODUCTION Many people have ostomies and lead full and active lives. Ostomy surgery is the main treatment for bypassing or replacing intestinal or urinary organs that have become diseased or dysfunctional. “Ostomy” means opening. It refers to a number of ways that bodily wastes are re-routed from your body. A urostomy specifi cally redirects urine. -

A Practical Guide for Stoma Problems Developed by the Ostomy Forum
A practical guide for Stoma problems Developed by the Ostomy Forum Dedicated to Stoma Care A practical guide for Stoma and Peristomal skin problems A practical guide for Stoma Developed by: Frances McKenzie, Amanda Smith, Doreen Woolley, Beverley Colton, Bart Tappe and Global Clinical Marketing, Dansac A/S. The practical guide is based on the Observation Index developed by the Ostomy Forum group (a specialized group of ET nurses from Sweden, Norway, The Netherlands, Poland, Japan, UK and Denmark) and is Normal Stoma made to help you manage common stoma and peristomal skin problems you might come across in your nursing practice. Stoma is a Greek word that means opening or mouth. It is a surgically created opening that can be temporary or permanent and allows for the Sharing best practice by use of this educational tool will lead to early excretion of faecal waste (colostomy, ileostomy) or urine (urostomy). detection and appropriate intervention to secure a high standard of stoma care. A stoma is a surgically made opening of the bowel: • The bowel is brought out through the abdominal wall This tool should be used in consultation with your Stoma Care Specialist. • It is matured and sutured subcutaneously • Faeces and urine will pass and be collected in a specially designed Disclaimer: ostomy pouch. We recognize that nurses in other practices will have different ways of treating the identified problems. The scope of this guide is to give first In the following pages you will find examples of different stoma problems step, easy to use, practical advice that is recognized and accepted and concrete suggestions for intervention and management of the stoma. -

Adjustable Gastric Banding
7 Review Article Page 1 of 7 Adjustable gastric banding Emre Gundogdu, Munevver Moran Department of Surgery, Medical School, Istinye University, Istanbul, Turkey Contributions: (I) Conception and design: All authors; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Emre Gündoğdu, MD, FEBS. Assistant Professor of Surgery, Department of Surgery, Medical School, Istinye University, Istanbul, Turkey. Email: [email protected]; [email protected]. Abstract: Gastric banding is based on the principle of forming a small volume pouch near the stomach by wrapping the fundus with various synthetic grafts. The main purpose is to limit oral intake. Due to the fact that it is a reversible surgery, ease of application and early results, the adjustable gastric band (AGB) operation has become common practice for the last 20 years. Many studies have shown that the effectiveness of LAGB has comparable results with other procedures in providing weight loss. Early studies have shown that short term complications after LAGB are particularly low when compared to the other complicated procedures. Even compared to RYGB and LSG, short-term results of LAGB have been shown to be significantly superior. However, as long-term results began to emerge, such as failure in weight loss, increased weight regain and long-term complication rates, interest in the procedure disappeared. The rate of revisional operations after LAGB is rapidly increasing today and many surgeons prefer to convert it to another bariatric procedure, such as RYGB or LSG, for revision surgery in patients with band removed after LAGB. -

Information for Patients Having a Sigmoid Colectomy
Patient information – Pre-operative Assessment Clinic Information for patients having a sigmoid colectomy This leaflet will explain what will happen when you come to the hospital for your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. Your surgeon will have already discussed your treatment with you and will give advice about what to do when you get home. What is a sigmoid colectomy? This operation involves removing the sigmoid colon, which lies on the left side of your abdominal cavity (tummy). We would then normally join the remaining left colon to the top of the rectum (the ‘storage’ organ of the bowel). The lines on the attached diagram show the piece of bowel being removed. This operation is done with you asleep (general anaesthetic). The operation not only removes the bowel containing the tumour but also removes the draining lymph glands from this part of the bowel. This is sent to the pathologists who will then analyse each bit of the bowel and the lymph glands in detail under the microscope. This operation can often be completed in a ‘keyhole’ manner, which means less trauma to the abdominal muscles, as the biggest wound is the one to remove the bowel from the abdomen. Sometimes, this is not possible, in which case the same operation is done through a bigger incision in the abdominal wall – this is called an ‘open’ operation. It does take longer to recover with an open operation but, if it is necessary, it is the safest thing to do. -
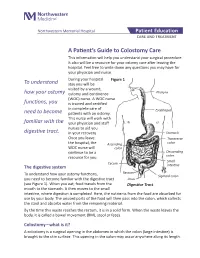
A Patient's Guide to Colostomy Care
Northwestern Memorial Hospital Patient Education CARE AND TREATMENT A Patient’s Guide to Colostomy Care This information will help you understand your surgical procedure. It also will be a resource for your ostomy care after leaving the hospital. Feel free to write down any questions you may have for your physician and nurse. During your hospital Figure 1 To understand stay you will be visited by a wound, how your ostomy ostomy and continence Pharynx (WOC) nurse. A WOC nurse functions, you is trained and certified in complete care of Esophagus need to become patients with an ostomy. This nurse will work with familiar with the your physician and staff nurses to aid you digestive tract. in your recovery. Stomach Once you leave Transverse the hospital, the Ascending colon WOC nurse will colon continue to be a Descending resource for you. colon Small Cecum The digestive system intestine Rectum To understand how your ostomy functions, Sigmoid colon you need to become familiar with the digestive tract Anus (see Figure 1). When you eat, food travels from the Digestive Tract mouth to the stomach. It then moves to the small intestine, where digestion is completed. Here, the nutrients from the food are absorbed for use by your body. The unused parts of the food will then pass into the colon, which collects the stool and absorbs water from the remaining material. By the time this waste reaches the rectum, it is in a solid form. When the waste leaves the body, it is called a bowel movement (BM), stool or feces. -
Hints and Tips
Hernia Simon, colostomy since 2010 Hints & Tips Dedicated to Stoma Care Dedicated to Stoma Care FOREWORD & ACKNOWLEDGEMENTS This booklet offers guidance to the person undergoing surgery which will result in stoma formation or for those post-operatively who may be at risk of or perhaps already have developed a parastomal hernia. Please discuss the content with your Stomal Therapy Nurse (STN) if you require additional advice or support. CONTENT What is a parastomal hernia? .........................................3 Am I at risk of developing a parastomal hernia? ������������4 What is my ideal weight? ................................................5 Practical hints & tips to reduce risk of developing a parastomal hernia .....................................6 I think I’ve developed a hernia - what should I do? ���������7 Parastomal hernia management �������������������������������������8 Exercise ..........................................................................9 Dansac would like to thank the following for their invaluable contribution to this booklet: Sharon Colman BSc (Hons) Community Stoma Nurse Specialist, Norfolk. Kevin Hayles Dip HE, RN Queens Hospital Romford, Essex. Debbie Johnson RGN, Stoma Specialist, Dansac UK, London Community. Jacqui North RGN BSc(Hons), Senior Clinical Nurse Specialist, Stoma Care, SE London Community. Jo Sica Clinical Nurse Specialist, Stoma Care, Kingston CCG. 2 WHAT IS A PARASTOMAL HERNIA? Parastomal hernia is a common complication which can affect some people following stoma formation. Research has shown that as many as 10-50% of patients may go on to develop a hernia.6, 9, 10 During your surgery an incision is made through the abdominal wall and muscle. This can result in a weakness in the muscle surrounding your stoma which may lead to a noticeable bulge behind or around the stoma. -

42 CFR Ch. IV (10–1–12 Edition) § 410.35
§ 410.35 42 CFR Ch. IV (10–1–12 Edition) the last screening mammography was (1) Colorectal cancer screening tests performed. means any of the following procedures furnished to an individual for the pur- [59 FR 49833, Sept. 30, 1994, as amended at 60 FR 14224, Mar. 16, 1995; 60 FR 63176, Dec. 8, pose of early detection of colorectal 1995; 62 FR 59100, Oct. 31, 1997; 63 FR 4596, cancer: Jan. 30, 1998] (i) Screening fecal-occult blood tests. (ii) Screening flexible § 410.35 X-ray therapy and other radi- sigmoidoscopies. ation therapy services: Scope. (iii) In the case of an individual at Medicare Part B pays for X-ray ther- high risk for colorectal cancer, screen- apy and other radiation therapy serv- ing colonoscopies. ices, including radium therapy and ra- (iv) Screening barium enemas. dioactive isotope therapy, and mate- (v) Other tests or procedures estab- rials and the services of technicians ad- lished by a national coverage deter- ministering the treatment. mination, and modifications to tests [51 FR 41339, Nov. 14, 1986. Redesignated at 55 under this paragraph, with such fre- FR 53522, Dec. 31, 1990] quency and payment limits as CMS de- termines appropriate, in consultation § 410.36 Medical supplies, appliances, with appropriate organizations and devices: Scope. (2) Screening fecal-occult blood test (a) Medicare Part B pays for the fol- means— lowing medical supplies, appliances (i) A guaiac-based test for peroxidase and devices: activity, testing two samples from (1) Surgical dressings, and splints, each of three consecutive stools, or, casts, and other devices used for reduc- (ii) Other tests as determined by the tion of fractures and dislocations. -

Double Barrel Wet Colostomy for Urinary and Fecal Diversion
Open Access Clinical Image J Urol Nephrol November 2017 Vol.:4, Issue:2 © All rights are reserved by Kang,et al. Journal of Double Barrel Wet Colostomy for Urology & Urinary and Fecal Diversion Nephrology Yu-Hao Xue and Chih-Hsiung Kang* Keywords: Double barrel wet colostomy; Urinary diversion; Fecal Department of Urology, Chang Gung Memorial Hospital-Kaohsiung diversion Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan, Republic of China Abstract Address for Correspondence A 60-year-old male who had a history of spinal cord injury received Chih-Hsiung Kang, Department of Urology, Chang Gung Memorial loop colostomy for fecal diversion and cystostomy for urinary diversion. Hospital - Kaohsiung Medical Center, Chang Gung University College Because he was diagnosed with muscle invasive bladder cancer, of Medicine, Taiwan, E- mail: [email protected] radical cystectomy and double barrel wet colostomy was conducted. Submission: 30 October, 2017 Computed tomography showed simultaneous urinary and fecal Accepted: 06 November, 2017 diversion and stone formation in the distal segment of colon conduit Published: 10 November, 2017 with urinary diversion. Copyright: © 2017 Kang CH, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, Introduction provided the original work is properly cited. In patients with an advanced primary or recurrent carcinoma, double-barreled wet colostomy can be used for pelvic exenteration Bilateral hydroureters and mild hydronephrosis were noted and and urinary tract reconstruction. It is a technique that separate we suspected the calculi impacted in bilateral ureteto-colostomy urinary and fecal diversion with a single abdominal stoma. -

“Eating with an Ostomy” Nutrition Guide
1 EATING WITH AN OSTOMY A Comprehensive Nutrition Guide for Those Living with an Ostomy First Edition by Joanna Burgess-Stocks BSN, RN, CWOCN A publication of UOAA, United Ostomy Associations of America 2 The printing of this publication was made possible by generous contributions from Sherry Lessard, George & Linda Salamy and the San Francisco (Golden Gate) Affiliated Support Group. Copyright © 2020 UOAA. All Rights Reserved. Disclaimer: This document contains information developed by United Ostomy Associations of America. This information does not replace medical advice from your health care provider. You are a unique individual and your experiences may differ from that of other patients. Talk to your health care provider if you have any questions about this document, your condition, or your treatment plan. Table of Contents 4 Acknowledgements 7 Introduction 9 The Role of the Registered Dietitian 11 Nutrition 101—The Basics 20 Ostomy and the Digestive System 26 Ostomy and the Urinary System 31 Post-Operative Nutritional Guidelines: The First 4–6 Weeks 35 Ileostomy: Specific Post-Op Guidelines 38 Nutrition after Recovery and Beyond 41 Hydration, Fluids, and Electrolytes 45 Ostomy and Medications 52 Guidelines for a Continent Fecal Diversion 55 Short Bowel Syndrome 60 Resources 63 Glossary of Terms 70 Appendix: Food Journal Food and Their Effects Chart References Testimonials Acknowledgements Thank you to all who worked diligently in the creation of this nutrition guide for people living with or facing ostomy surgery. This document came to fruition with the help and expertise of registered dietitians, wound ostomy and continence nurses, medical educators, and patient reviewers. -

Intestinal Stomas Proximal the Ileostomy
INTESTINAL total water and sodium in the body. This is accentuated the more Intestinal stomas proximal the ileostomy. In the early stages, a distal ileostomy typically discharges 1000–2000 ml/day, but can increase to Richard N Saunders 5000–6000 ml/day in exceptional circumstances, leading to dehy- David Hemingway dration and electrolyte abnormalities. Occasionally, this is driven by proximal disease (e.g. Crohn’s disease), but a cause is not identified in many cases. The output can usually be reduced to 250–750 ml/day with supportive care and antidiarrhoeal agents. In the longer term, the systemic effects of an ileostomy include an increased incidence of renal tract calculi (60% composed of uric acid). Some studies also suggest a threefold increase in the incidence of gallstones, but this remains controversial. Abstract Intestinal stomas are frequently necessary after abdominal surgery. A Principles of stoma formation thorough understanding of this less than glamorous area of surgical practice can prevent complications and make a significant difference Discussion – the possibility of a stoma should be discussed to patients. The first part of this review focuses on the basic principles with patients undergoing elective or emergency colorectal sur- underpinning the management of intestinal stomas (i.e. physiology, for- gery. A Stoma Nurse should be involved as early as possible. The mation, common complications). The second part comments briefly on location and construction of the stoma is critical in ensuring good specific types of stoma and their role in current clinical practice. quality of life and avoiding management problems. Assessment – preoperatively, patients are assessed lying Keywords colostomy; ileostomy; intestinal surgery; stoma down, sitting and standing, and the best sites marked. -

The Costs and Benefits of Moving to the ICD-10 Code Sets
CHILDREN AND ADOLESCENTS This PDF document was made available from www.rand.org as a public CIVIL JUSTICE service of the RAND Corporation. EDUCATION ENERGY AND ENVIRONMENT Jump down to document HEALTH AND HEALTH CARE 6 INTERNATIONAL AFFAIRS POPULATION AND AGING The RAND Corporation is a nonprofit research PUBLIC SAFETY SCIENCE AND TECHNOLOGY organization providing objective analysis and effective SUBSTANCE ABUSE solutions that address the challenges facing the public TERRORISM AND HOMELAND SECURITY and private sectors around the world. TRANSPORTATION AND INFRASTRUCTURE U.S. NATIONAL SECURITY Support RAND Purchase this document Browse Books & Publications Make a charitable contribution For More Information Visit RAND at www.rand.org Explore RAND Science and Technology View document details Limited Electronic Distribution Rights This document and trademark(s) contained herein are protected by law as indicated in a notice appearing later in this work. This electronic representation of RAND intellectual property is provided for non-commercial use only. Permission is required from RAND to reproduce, or reuse in another form, any of our research documents for commercial use. This product is part of the RAND Corporation technical report series. Reports may include research findings on a specific topic that is limited in scope; present discus- sions of the methodology employed in research; provide literature reviews, survey instruments, modeling exercises, guidelines for practitioners and research profes- sionals, and supporting documentation; -

Pdfs–For–Download/Ostomy–Care/Whats–Right–For– Me–-–Ileostomy 907602-806.Pdf on October 2, 2019
cancer.org | 1.800.227.2345 Ileostomy Guide Ileostomy surgery is done for many different diseases and problems. Some conditions that can lead to ileostomy surgery include ulcerative colitis, Crohn’s disease, familial polyposis, and cancer. Sometimes an ileostomy is only needed for a short time (temporary), or it may be needed for the rest of a person's life (permanent). For the thousands of people who have serious digestive diseases, an ileostomy can be the start of a new and healthier life. If you’ve had a chronic (long-term) problem or a life- threatening disease like cancer, you can look forward to feeling better after you recover from ileostomy surgery. You can also look forward to returning to most, if not all of the activities you enjoyed in the past. This guide will help you better understand ileostomy – what it is, why it’s needed, how it affects the normal digestive system1, and what changes it brings to a person’s life. ● What Is an Ileostomy? ● Types of Ileostomies and Pouching Systems ● Caring for an Ileostomy What Is an Ileostomy? An ileostomy is an opening in the belly (abdominal wall) that’s made during surgery. It's usually needed because a problem is causing the ileum to not work properly, or a disease is affecting that part of the colon and it needs to be removed. The end of the ileum (the lowest part of the small intestine) is brought through this opening to form a 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 stoma, usually on the lower right side of the abdomen.