Association Between Use of Sodium-Glucose Cotransporter 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

View a Copy of This Licence, Visit Tivecommons.Org/Licenses/By/4.0
Katakami et al. Cardiovasc Diabetol (2020) 19:110 https://doi.org/10.1186/s12933-020-01079-4 Cardiovascular Diabetology ORIGINAL INVESTIGATION Open Access Tofoglifozin does not delay progression of carotid atherosclerosis in patients with type 2 diabetes: a prospective, randomized, open-label, parallel-group comparative study Naoto Katakami1,2* , Tomoya Mita3, Hidenori Yoshii4, Toshihiko Shiraiwa5, Tetsuyuki Yasuda6, Yosuke Okada7, Keiichi Torimoto7, Yutaka Umayahara8, Hideaki Kaneto9, Takeshi Osonoi10, Tsunehiko Yamamoto11, Nobuichi Kuribayashi12, Kazuhisa Maeda13, Hiroki Yokoyama14, Keisuke Kosugi15, Kentaro Ohtoshi16, Isao Hayashi17, Satoru Sumitani18, Mamiko Tsugawa19, Kayoko Ryomoto20, Hideki Taki21, Tadashi Nakamura22, Satoshi Kawashima23, Yasunori Sato24, Hirotaka Watada3 and Iichiro Shimomura1 on behalf of the UTOPIA study investigators Abstract Background: This study aimed to investigate the preventive efects of tofoglifozin, a selective sodium-glucose cotransporter 2 (SGLT2) inhibitor, on atherosclerosis progression in type 2 diabetes (T2DM) patients without apparent cardiovascular disease (CVD) by monitoring carotid intima-media thickness (IMT). Methods: This prospective, randomized, open-label, blinded-endpoint, multicenter, parallel-group, comparative study included 340 subjects with T2DM and no history of apparent CVD recruited at 24 clinical units. Subjects were randomly allocated to either the tofoglifozin treatment group (n 169) or conventional treatment group using drugs other than SGLT2 inhibitors (n 171). Primary outcomes were changes= in mean and maximum common carotid IMT measured by echography during= a 104-week treatment period. Results: In a mixed-efects model for repeated measures, the mean IMT of the common carotid artery (mean- IMT-CCA), along with the right and left maximum IMT of the CCA (max-IMT-CCA), signifcantly declined in both the tofoglifozin ( 0.132 mm, SE 0.007; 0.163 mm, SE 0.013; 0.170 mm, SE 0.020, respectively) and the control group ( 0.140 mm,− SE 0.006; 0.190 mm,− SE 0.012; 0.190 mm,− SE 0.020, respectively). -

Supplementary Material
Supplementary material Table S1. Search strategy performed on the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL). 1. Randomi*ed study OR random allocation OR Randomi*ed controlled trial OR Random* Control* trial OR RCT Epidemiological study 2. sodium glucose cotransporter 2 OR sodium glucose cotransporter 2 inhibitor* OR sglt2 inhibitor* OR empagliflozin OR dapagliflozin OR canagliflozin OR ipragliflozin OR tofogliflozin OR ertugliflozin OR sotagliflozin OR sergliflozin OR remogliflozin 3. 1 AND 2 1 Table S2. Safety outcomes of empagliflozin and linagliptin combination therapy compared with empagliflozin or linagliptin monotherapy in treatment naïve type 2 diabetes patients Safety outcome Comparator 1 Comparator 2 I2 RR [95% CI] Number of events Number of events / / total subjects total subjects i. Empagliflozin + linagliptin vs empagliflozin monotherapy Empagliflozin + Empagliflozin linagliptin monotherapy ≥ 1 AE(s) 202/272 203/270 77% 0.99 [0.81, 1.21] ≥ 1 drug-related 37/272 38/270 0% 0.97 [0.64, 1.47] AE(s) ≥ 1 serious AE(s) 13/272 19/270 0% 0.68 [0.34, 1.35] Hypoglycaemia* 0/272 5/270 0% 0.18 [0.02, 1.56] UTI 32/272 25/270 29% 1.28 [0.70, 2.35] Events suggestive 12/272 13/270 9% 0.92 [0.40, 2.09] of genital infection i. Empagliflozin + linagliptin vs linagliptin monotherapy Empagliflozin + Linagliptin linagliptin monotherapy ≥ 1 AE(s) 202/272 97/135 0% 1.03 [0.91, 1.17] ≥ 1 drug-related 37/272 17/135 0% 1.08 [0.63, 1.84] AE(s) ≥ 1 serious AE(s) 13/272 2/135 0% 3.22 [0.74, 14.07] Hypoglycaemia* 0/272 1/135 NA 0.17 [0.01, 4.07] UTI 32/272 12/135 0% 1.32 [0.70, 2.49] Events suggestive 12/272 4/135 0% 1.45 [0.47, 4.47] of genital infection RR, relative risk; AE, adverse event; UTI, urinary tract infection. -

Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix
United States International Trade Commission Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix USITC Publication 4208 December 2010 U.S. International Trade Commission COMMISSIONERS Deanna Tanner Okun, Chairman Irving A. Williamson, Vice Chairman Charlotte R. Lane Daniel R. Pearson Shara L. Aranoff Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix Publication 4208 December 2010 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 15, 2010, set forth at the end of this publication, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the United States International Trade Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement changes to the Pharmaceutical Appendix, effective on January 1, 2011. Table 1 International Nonproprietary Name (INN) products proposed for addition to the Pharmaceutical Appendix to the Harmonized Tariff Schedule INN CAS Number Abagovomab 792921-10-9 Aclidinium Bromide 320345-99-1 Aderbasib 791828-58-5 Adipiplon 840486-93-3 Adoprazine 222551-17-9 Afimoxifene 68392-35-8 Aflibercept 862111-32-8 Agatolimod -

CDR Clinical Review Report for Soliqua
CADTH COMMON DRUG REVIEW Clinical Review Report Insulin glargine and lixisenatide injection (Soliqua) (Sanofi-Aventis) Indication: adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus inadequately controlled on basal insulin (less than 60 units daily) alone or in combination with metformin. Service Line: CADTH Common Drug Review Version: Final (with redactions) Publication Date: January 2019 Report Length: 118 Pages Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

Glucose Cotransporter 2 Inhibitor, Attenuates Body Weight Gain and Fat Accumulation in Diabetic and Obese Animal Models
OPEN Citation: Nutrition & Diabetes (2014) 4, e125; doi:10.1038/nutd.2014.20 & 2014 Macmillan Publishers Limited All rights reserved 2044-4052/14 www.nature.com/nutd ORIGINAL ARTICLE Tofogliflozin, a sodium/glucose cotransporter 2 inhibitor, attenuates body weight gain and fat accumulation in diabetic and obese animal models M Suzuki1, M Takeda1, A Kito1, M Fukazawa1, T Yata2, M Yamamoto1, T Nagata1, T Fukuzawa1, M Yamane1, K Honda1, Y Suzuki1 and Y Kawabe1 OBJECTIVE: Tofogliflozin, a highly selective inhibitor of sodium/glucose cotransporter 2 (SGLT2), induces urinary glucose excretion (UGE), improves hyperglycemia and reduces body weight in patients with Type 2 diabetes (T2D). The mechanisms of tofogliflozin on body weight reduction were investigated in detail with obese and diabetic animal models. METHODS: Diet-induced obese (DIO) rats and KKAy mice (a mouse model of diabetes with obesity) were fed diets containing tofogliflozin. Body weight, body composition, biochemical parameters and metabolic parameters were evaluated. RESULTS: In DIO rats tofogliflozin was administered for 9 weeks, UGE was induced and body weight gain was attenuated. Body fat mass decreased without significant change in bone mass or lean body mass. Food consumption (FC) increased without change in energy expenditure, and deduced total calorie balance (deduced total calorie balance ¼ FC À UGE À energy expenditure) decreased. Respiratory quotient (RQ) and plasma triglyceride (TG) level decreased, and plasma total ketone body (TKB) level increased. Moreover, plasma leptin level, adipocyte cell size and proportion of CD68-positive cells in mesenteric adipose tissue decreased. In KKAy mice, tofogliflozin was administered for 3 or 5 weeks, plasma glucose level and body weight gain decreased together with a reduction in liver weight and TG content without a reduction in body water content. -

Exendin-4 Peptide Analogues As Dual Glp-1/Gip Receptor Agonists
(19) TZZ¥ZZ_Z_T (11) EP 3 080 150 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07K 14/575 (2006.01) C07K 14/605 (2006.01) 01.08.2018 Bulletin 2018/31 (86) International application number: (21) Application number: 14828149.6 PCT/EP2014/077336 (22) Date of filing: 11.12.2014 (87) International publication number: WO 2015/086728 (18.06.2015 Gazette 2015/24) (54) EXENDIN-4 PEPTIDE ANALOGUES AS DUAL GLP-1/GIP RECEPTOR AGONISTS EXENDIN-4-PEPTIDANALOGA ALS DUALE GLP-1/GIP-REZEPTORAGONISTEN ANALOGUES PEPTIDIQUES D’EXENDINE-4 EN TANT QU’AGONISTES DU RÉCEPTEUR GIP/GLP-1 DOUBLE (84) Designated Contracting States: (74) Representative: Weickmann & Weickmann AL AT BE BG CH CY CZ DE DK EE ES FI FR GB PartmbB GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Postfach 860 820 PL PT RO RS SE SI SK SM TR 81635 München (DE) (30) Priority: 13.12.2013 EP 13306712 (56) References cited: WO-A1-2012/167744 WO-A2-2009/035540 (43) Date of publication of application: US-A1- 2011 166 062 US-A1- 2012 196 802 19.10.2016 Bulletin 2016/42 • JOHN L. KRSTENANSKY ET AL: "Importance of (73) Proprietor: SANOFI the 10-13 region of glucagon for its receptor 75008 Paris (FR) interactionsand activation of adenylate cyclase", BIOCHEMISTRY, vol. 25, no. 13, 1 July 1986 (72) Inventors: (1986-07-01), pages 3833-3839, XP055117918, • KADEREIT, Dieter ISSN: 0006-2960, DOI: 10.1021/bi00361a014 65926 Frankfurt am Main (DE) • VICTOR A. -

Renato Wilberto Zilli Eficácia Em Longo Prazo Das
RENATO WILBERTO ZILLI EFICÁCIA EM LONGO PRAZO DAS GLIFLOZINAS VERSUS GLIPTINAS NO TRATAMENTO DO DIABETES MELLITUS TIPO 2 APÓS FALÊNCIA DA METFORMINA COMO MONOTERAPIA: REVISÃO SISTEMÁTICA E METANÁLISE EM REDE Tese apresentada ao Programa de Ciências Médicas da Faculdade de Medicina da Universidade de São Paulo para obtenção do título de Doutor em Ciências. Área de Concentração: Processos Imunes e Infecciosos Orientador: Prof. Dr. Fabiano Pinheiro da Silva (Versão corrigida. Resolução CoPGr 6018/11, de 13 de outubro de 2011. A versão original está disponível na Biblioteca da FMUSP) São Paulo 2017 Dados Internacionais de Catalogação na Publicação (CIP) Preparada pela Biblioteca da Faculdade de Medicina da Universidade de São Paulo ©reprodução autorizada pelo autor Zilli, Renato Wilberto Eficácia em longo prazo das gliflozinas versus gliptinas no tratamento do diabetes mellitus tipo 2 após falência da metformina como monoterapia : revisão sistemática e metanálise em rede / Renato Wilberto Zilli ‐‐ São Paulo, 2017. Tese(doutorado)--Faculdade de Medicina da Universidade de São Paulo. Programa de Ciências Médicas. Área de concentração: Processos Imunes e Infecciosos. Orientador: Fabiano Pinheiro da Silva. Descritores: 1.Diabetes mellitus tipo 2 2.Metanálise 3.Terapia combinada 4.Falha de tratamento 5.Metformina 6.Inibidores da dipeptidil peptidase IV 7.Transportador 2 de glucose‐sódio/inibidores 8.Empagliflozina 9.Dapagliflozina 10.Saxagliptina USP/FM/DBD ‐302/17 Esta tese de doutorado está de acordo com as seguintes normas, em vigor no momento desta publicação: Referências: adaptado de International Committee of Medical Journals Editors (Vancouver). Guia de apresentação e dissertações, teses e monografias. Elaborado por Anneliese Cordeiro da Cunha, Maria Julia de A.L. -
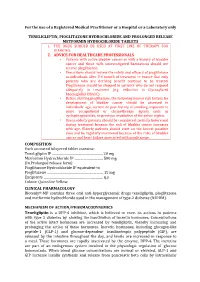
For the Use of a Registered Medical Practitioner Or a Hospital Or a Laboratory Only TENELIGLIPTIN, PIOGLITAZONE HYDROCHLORIDE AN
For the use of a Registered Medical Practitioner or a Hospital or a Laboratory only TENELIGLIPTIN, PIOGLITAZONE HYDROCHLORIDE AND PROLONGED RELEASE METFORMIN HYDROCHLORIDE TABLETS 1. THE DRUG SHOULD BE USED AT FIRST LINE OF THERAPY FOR DIABETES. 2. ADVICE FOR HEALTHCARE PROFESSIONALS • Patients with active bladder cancer or with a history of bladder cancer and those with uninvestigated haematuria should not receive pioglitazone. • Prescribers should review the safety and efficacy of pioglitazone in individuals after 3-6 month of treatment to ensure that only patients who are deriving benefit continue to be treated. Pioglitazone should be stopped in patients who do not respond adequately to treatment (e.g. reduction in Glycosylated haemoglobin HbA1C). • Before starting pioglitazone, the following known risk factors for development of bladder cancer should be assessed in individuals: age, current or past history of smoking, exposure to some occupational or chemotherapy agents such as cyclophosphamide, or previous irradiation of the pelvic region. • Use in elderly patients should be considered carefully before and during treatment because the risk of bladder cancer increases with age. Elderly patients should start on the lowest possible dose and be regularly monitored because of the risks of bladder cancer and heart failure associated with pioglitazone. COMPOSITION Each uncoated bilayered tablet contains: . 20 mg (InTeneligliptin Prolonged IP release .………………………..……………….. form) PioglitazoneMetformin Hydrochloride Hydrochloride IP IP …………………..…... equivalent to mg Pio . 15 mg .s Colour:glitazone Quinoline ………………………….…………………… Yellow Excipients ………………………….……………………..... q CLINICAL PHARMACOLOGY Biotenly®-MP contains three oral anti-hyperglycaemic drugs teneligliptin, pioglitazone and metformin hydrochloride used in the management of type-2 diabetes (NIDDM). MECHANISM OF ACTION/PHARMACODYNEMICS Teneligliptin is a DPP-4 inhibitor, which is believed to exert its actions in patients with type 2 diabetes by slowing the inactivation of incretin hormones. -

IJBCP International Journal of Basic & Clinical Pharmacology the Observational, Cross-Sectional Study of Drug Utilization
Print ISSN: 2319-2003 | Online ISSN: 2279-0780 IJBCP International Journal of Basic & Clinical Pharmacology DOI: http://dx.doi.org/10.18203/2319-2003.ijbcp20194771 Original Research Article The observational, cross-sectional study of drug utilization 90% and use of dipeptidyl peptidase-4 inhibitor in the patients with type 2 diabetes mellitus Prashant P. Shivgunde1*, Shantanu R. Joshi2, Archana D. Kodilkar1 1Department of University Research, Maharashtra ABSTRACT University of Health Sciences (MUHS), Mhasrul, Vani- Background: Diabetes is a chronic metabolic disease which affects the quality Dindori Road, Nashik, of life. It leads to multiple complications due to metabolic involvement. Out of Maharashtra, India multiple drugs used to treat diabetes, dipeptidyl peptidase 4 (DPP-4) inhibitors 2 Global Herbs Pharmaceuticals, are comparatively new drugs used for type-2-diabetes mellitus (DM) treatment. Pune-Satara Road, Pune, This study aimed to find out the drug utilization (DU) 90% and use of DPP-4 Maharashtra, India inhibitors in patients with type-2-DM. Methods: A prospective, cross-sectional, observational study was conducted at Received: 28 September 2019 a private healthcare clinic of an endocrinologist in Nashik. Type-2-DM patients Revised: 11 October 2019 of both sexes were selected and a total of 199 patients were enrolled in the Accepted: 14 October 2019 study. The consented patients were interviewed and prescription copies were collected. After studying them; statistical analysis was done and results and *Correspondence to: conclusions were drawn. Dr. Prashant P. Shivgunde, Results: Out of total prescribed drugs, 58.77% of drugs were anti-diabetics. It Email: prashantshivgunde@ was observed that the biguanides were most frequently (25.32%) prescribed gmail.com while the least prescribed drugs were meglitinide analogues (0.08%). -

Comparison of Tofogliflozin 20 Mg and Ipragliflozin 50 Mg Used Together
2017, 64 (10), 995-1005 Original Comparison of tofogliflozin 20 mg and ipragliflozin 50 mg used together with insulin glargine 300 U/mL using continuous glucose monitoring (CGM): A randomized crossover study Soichi Takeishi, Hiroki Tsuboi and Shodo Takekoshi Department of Diabetes, General Inuyama Chuo Hospital, Inuyama 484-8511, Japan Abstract. To investigate whether sodium glucose co-transporter 2 inhibitors (SGLT2i), tofogliflozin or ipragliflozin, achieve optimal glycemic variability, when used together with insulin glargine 300 U/mL (Glargine 300). Thirty patients with type 2 diabetes were randomly allocated to 2 groups. For the first group: After admission, tofogliflozin 20 mg was administered; Fasting plasma glucose (FPG) levels were titrated using an algorithm and stabilized at 80 mg/dL level with Glargine 300 for 5 days; Next, glucose levels were continuously monitored for 2 days using continuous glucose monitoring (CGM); Tofogliflozin was then washed out over 5 days; Subsequently, ipragliflozin 50 mg was administered; FPG levels were titrated using the same algorithm and stabilized at 80 mg/dL level with Glargine 300 for 5 days; Next, glucose levels were continuously monitored for 2 days using CGM. For the second group, ipragliflozin was administered prior to tofogliflozin, and the same regimen was maintained. Glargine 300 and SGLT2i were administered at 8:00 AM. Data collected on the second day of measurement (mean amplitude of glycemic excursion [MAGE], average daily risk range [ADRR]; on all days of measurement) were analyzed. Area over the glucose curve (<70 mg/dL; 0:00 to 6:00, 24-h), M value, standard deviation, MAGE, ADRR, and mean glucose levels (24-h, 8:00 to 24:00) were significantly lower in patients on tofogliflozin than in those on ipragliflozin. -

Populationsweite Utilisationsuntersuchung in Den Chronischen Krankheitsbildern Hypertonie, Hyperlipid¨Amieund Typ 2 Diabetes Mellitus –
Ruhr-Universit¨atBochum Prof. Dr. rer. nat. Hans J. Trampisch Dienstort: Abteilung f¨urMedizinische Informatik, Biometrie und Epidemiologie Populationsweite Utilisationsuntersuchung in den chronischen Krankheitsbildern Hypertonie, Hyperlipid¨amieund Typ 2 Diabetes Mellitus { Eine Studie des Projekts PUKO-BHD an der Medizinischen Universit¨atWien Inaugural-Dissertation zur Erlangung des Doktorgrades der Medizin einer Hohen Medizinischen Fakult¨at der Ruhr-Universit¨atBochum vorgelegt von: Lisanne M. Jandeck aus Herford 2014 Dekan: Prof. Dr. med. Albrecht Bufe Referent: Prof. Dr. rer. nat. Hans J. Trampisch Korreferent: Prof. Dr. med. J¨urgenWindeler Tag der M¨undlichen Pr¨ufung:09.02.2017 Abstract Jandeck Lisanne M. Populationsweite Utilisationsuntersuchung in den chronischen Krankheitsbildern Hypertonie, Hyperlipid¨amieund Typ 2 Diabetes Mellitus Problem: Hypertonie (HT), Hyperlipid¨amie(HL) und Typ 2 Diabetes Mellitus (DM) stellen die h¨aufigstenchronischen Erkrankungen in Osterreich¨ dar, besonders bei Uber-50j¨ahrigen.Die¨ Zielsetzung dieser Teilstudie Utilisation\ des Projekts mit " dem Titel PUKO-BHD { Pr¨avalenz, Utilisation, Kosten und Outcome bei Blut- " hochdruck, Hyperlipid¨amieund Typ 2 Diabetes Mellitus\ ist eine populationsweite epidemiologische Untersuchung zu der Utilisation von Arzneimitteln zur Behand- lung dieser Krankheiten, insbesondere in Bezug auf Mehrfachverschreibungen (dou- ble prescriptions, DP) und Verschreibungen von Kombinationen von Wirkstoffen, die (schwerwiegende) Wechselwirkungen erzeugen k¨onnen (drug-drug -

Clinical Comparison of Tofogliflozin and Empagliflozin Based on An
Obesity Medicine 14 (2019) 100088 Contents lists available at ScienceDirect Obesity Medicine journal homepage: www.elsevier.com/locate/obmed Original research Clinical comparison of tofogliflozin and empagliflozin based on an analysis of 24-h accumulated urine in Japanese patients with type 2 diabetes mellitus T ∗ Kazuo Kobayashia, , Masao Toyodab, Nobuo Hatoric a Kobayashi Clinic of Internal Medicine, Sagamihara, Japan b Division of Nephrology, Endocrinology and Metabolism, Department of Internal Medicine, Tokai University School of Medicine, Isehara, Japan c Kobayashi Hospital, Odawara, Japan ARTICLE INFO ABSTRACT Keywords: Aim: In Japan, six sodium-glucose co-transporter 2 inhibitors have been approved for use, and some agents are Tofogliflozin associated with a significant decrease in cardiovascular events. In this study, the effects of tofogliflozin and Empagliflozin empagliflozin were compared. 24-H accumulated urine Methods: Patients with type 2 diabetes mellitus who were administered tofogliflozin (n = 10) and empagliflozin Sodium-glucose co-transporter 2 inhibitor (n = 12) were extracted. The clinical parameters and 24-h accumulated urine samples before and after 48 weeks Hematocrit were analyzed with generalized linear mixed model. Results: Both groups showed significant differences in the following parameters: body weight (p < 0.0001), mean blood pressure (p = 0.006), glycated hemoglobinA1c (p < 0.0001), alanine aminotransferase (p < 0.0001), high-density lipoprotein cholesterol (p < 0.0001), homeostatic model assessment 2 (%S) (p = 0.006), volume of 24-h accumulated urine (p < 0.0001), and 24-h urine glucose excretion (p < 0.0001). The hematocrit differed significantly over the study period (p < 0.0001); however, empaglifozin had a sig- nificantly stronger effect on the hematocrit than tofoglifozin (p = 0.007).