UK Clinical Teaching Fellows Forum 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Cardiac Arrest Audit Participating Hospitals
Updated June 2018 National Cardiac Arrest Audit Participating Hospitals The total number of hospitals signed up to participate in NCAA is 197. England Birmingham and Black Country Non-participant New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Participant Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital Heart of England NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital Heart of England NHS Foundation Trust Hereford County Hospital Wye Valley NHS Trust Manor Hospital Walsall Healthcare NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital Heart of England NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Central England Participant George Eliot Hospital George Eliot Hospital NHS Trust Glenfield Hospital University Hospitals of Leicester NHS Trust Kettering General Hospital Kettering General Hospital NHS Foundation Trust Leicester General Hospital University Hospitals of Leicester NHS Trust Leicester Royal Infirmary University Hospitals of Leicester NHS Trust Northampton General Hospital Northampton General Hospital NHS Trust Hospital of St Cross, Rugby University Hospitals Coventry and Warwickshire NHS Trust University Hospital Coventry University Hospitals Coventry and Warwickshire NHS Trust -
ABCD Nationwide Audit of Freestyle Libre (FSL)
ABCD nationwide audit of FreeStyle Libre (FSL) Dr Harshal Deshmukh MRCP MPH PhD NIHR Clinical Lecturer in Endocrinology and Diabetes Dr Emma Wilmot Dr Chris Walton Dr Bob Ryder Prof Thozhukat Sathyapalan ABCD nationwide audit of FreeStyle Libre DISCLOSURES Disclosures • EW has received personal fees from Abbott Diabetes Care, Dexcom, Diasend, Eli Lilly, Medtronic, Novo Nordisk, Sanofi Aventis • BR has received speaker fees, and/or consultancy fees and/or educational sponsorships from AstraZeneca, BioQuest, GI Dynamics, Janssen, Novo Nordisk, Sanofi-Aventis and Takeda • HD TS and CW have no relevant disclosures Funding The ABCD nationwide Freestyle Libre audit is supported by a grant from Abbott UK. The audit was independently initiated and performed by ABCD, and the authors remain independent in the analysis and preparation of this report. ABCD nationwide audit of FreeStyle Libre • FreeStyle Libre is a flash glucose monitoring system which monitors interstitial glucose levels • Consists of a sensor with a microfilament, worn on the back of the arm and a hand- held reader • When the reader unit is passed over the sensor, it shows the interstitial glucose levels • The sensor lasts for 14 days, then needs to be replaced ABCD nationwide audit of FreeStyle Libre ABCD FSL Audit Main Objectives The ABCD FSL Audit aims to explore the impact of the FSL on the following: . HbA1c . Hypoglycaemia awareness . Resource utilisation: hospital admissions . User satisfaction . Diabetes related distress . Discontinuation rate and causes ABCD nationwide audit of FreeStyle Libre Methods ABCD nationwide audit of FreeStyle Libre • Audit conducted in 114 centres in the UK • A secure IT tool was developed on the NHS computer network, N3, to make this process as easy and user friendly as possible ABCD nationwide audit of FreeStyle Libre . -

List 2018 a 18/0347 8 Abelia Close, West End, Woking, Surrey, GU24 9PG 18/0115 24 Academy Close, Camberley, Surrey, GU15 4BU
List 2018 A 18/0347 8 Abelia Close, West End, Woking, Surrey, GU24 9PG 18/0115 24 Academy Close, Camberley, Surrey, GU15 4BU 18/0491 Units 1-5 Admiralty Way, Camberley, Surrey, GU15 3DT 18/0694 Unit 7, Phase 4 Albany Park, Camberley, Surrey, GU16 7PL 18/0806 16 Albert Road, Bagshot, Surrey, GU19 5QJ 18/0630 1 Alexandra Avenue, Camberley, Surrey, GU15 3BG 18/1015 Sandhurst Chalet, Alfriston Road, Deepcut, Camberley, Surrey, GU16 6QS 18/0521 The Surgery, 39 All Saints Road, Lightwater, Surrey, GU18 5SQ 18/0383 22 Alpha Road, Chobham, Woking, Surrey, GU24 8NF 18/0860 5 Alphington Avenue, Frimley, CAMBERLEY, GU16 8LA 18/0024 31 Alphington Avenue, Frimley, Camberley, Surrey, GU16 8LL 18/0063 45 Alphington Avenue, Frimley, Camberley, Surrey, GU16 8LL 18/0717 8 Amber Hill, Camberley, Surrey, GU15 1EB 18/0673 27 Ambleside Close, Mytchett, Camberley, Surrey, GU16 6DG 18/0394 1 Ambleside Road, Lightwater, Surrey, Gu18 5TA 18/0844 25 Ambleside Road, Lightwater, GU18 5TA 18/0199 27 Ambleside Road, Lightwater, Surrey, GU16 6DG 18/0392 32A Ambleside Road, Lightwater, Surrey, GU16 5TA 18/0657 32A Ambleside Road, Lightwater, Surrey, GU16 5TA 18/0271 87 Ambleside Road, Lightwater, Surrey, GU18 5UH 18/0699 137 Ambleside Road, Lightwater, GU18 5UL 18/0345 142 Ambleside Road, Lightwater, Surrey, GU18 5UN 18/0037 153 Ambleside Road, Lightwater, Surrey, GU18 5UN 18/0577 11 Anderson Place, Bagshot, Surrey, GU19 5LX 18/0060 6 Ardrossan Avenue, Camberley, Surrey, GU15 1DD 18/0830 15 Arthur Close, Bagshot, GU19 5QT 18/0889 16 Arundel Road, Camberley, GU15 1DL -
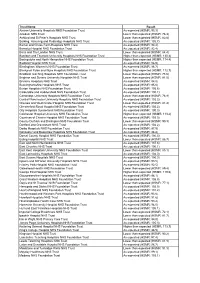
HSMR June09 Choices
Trust Name Result Aintree University Hospitals NHS Foundation Trust As expected (HSMR: 93.3) Airedale NHS Trust Lower than expected (HSMR: 76.3) Ashford and St Peter's Hospitals NHS Trust Lower than expected (HSMR: 82.8) Barking, Havering and Redbridge Hospitals NHS Trust As expected (HSMR: 105.7) Barnet and Chase Farm Hospitals NHS Trust As expected (HSMR: 94.4) Barnsley Hospital NHS Foundation Trust As expected (HSMR: 92.4) Barts and The London NHS Trust Lower than expected (HSMR: 84.4) Basildon and Thurrock University Hospitals NHS Foundation Trust Higher than expected (HSMR: 130.4) Basingstoke and North Hampshire NHS Foundation Trust Higher than expected (HSMR: 114.4) Bedford Hospital NHS Trust As expected (HSMR: 96.9) Birmingham Women's NHS Foundation Trust As expected (HSMR: 96.7) Blackpool Fylde and Wyre Hospitals NHS Foundation Trust Higher than expected (HSMR: 112.7) Bradford Teaching Hospitals NHS Foundation Trust Lower than expected (HSMR: 78.6) Brighton and Sussex University Hospitals NHS Trust Lower than expected (HSMR: 81.5) Bromley Hospitals NHS Trust As expected (HSMR: 94.0) Buckinghamshire Hospitals NHS Trust As expected (HSMR: 95.6) Burton Hospitals NHS Foundation Trust As expected (HSMR: 105.6) Calderdale and Huddersfield NHS Foundation Trust As expected (HSMR: 100.1) Cambridge University Hospitals NHS Foundation Trust Lower than expected (HSMR: 78.9) Central Manchester University Hospitals NHS Foundation Trust As expected (HSMR: 102.2) Chelsea and Westminster Hospital NHS Foundation Trust Lower than expected (HSMR: -

Suspected Cancer Fast Track Referral
Suspected Cancer Frimley Health Fast Track Referral NHS Foundation Trust IMPORTANT information about your appointment Your doctor/dentist has requested you are Hospital addresses seen by a specialist or have a test within the next two weeks. You will be seen at one of the following hospitals: You may be offered the opportunity to book an Frimley Park Sites: appointment before you leave the surgery, or will be offered an appointment by telephone Frimley Park Hospital at the earliest opportunity. Portsmouth Road, Surrey, GU16 7UJ It is important you make yourself available Aldershot Centre for Health and attend this appointment. Hospital Hill, Aldershot, Hampshire GU11 1AY Should I be worried? Fleet Community Hospital The need for an early appointment does not mean Church Road, Fleet, Hampshire, GU51 4LZ you have cancer, however your doctor/dentist would like you to be seen by a specialist as soon as Farnham Hospital possible. Hale Road, Farnham, Surrey, GU9 9QL What is a Suspected Cancer The Bracknell Clinic Fast Track referral? Eastern Gate, Brants Bridge, Bracknell, Berkshire This referral is to ensure anyone with symptoms/ RG12 9BG initial test results that may be suspicious of cancer will be seen by a specialist or have a specialist test Heatherwood and Wexham Sites: within two weeks. Wexham Park Hospital, The aim is to exclude cancer or provide diagnosis, Wexham Street, Slough, SL2 4HL intervention and treatment, if required, at the earliest opportunity. Heatherwood Hospital, London Road, Ascot, SL5 8AA What happens now? King Edward VII Hospital, St Leonards Road, Windsor, SL4 3DP • You will be helped to book an appointment before you leave the surgery or you may receive St Mark’s Hospital, an appointment by telephone, please accept a St Mark’s Road, Maidenhead, SL6 6DU telephone call from an unknown number. -

The Royal Bank of Scotland Hospital List for Gold Option
GEN3461_97000805.qxp:GEN3461_97000805 13/7/12 16:13 Page 1 The Royal Bank of Scotland Hospital List for Gold Option England Cheshire Bedfordshire Cheadle BMI The Alexandra Hospital Chester Nuffield Health Grosvenor Hospital Bedford Bedford Hospital (Chester) Biddenham BMI The Manor Hospital Crewe BMI The South Cheshire Private Luton Luton & Dunstable Hospital - Cobham Hospital Clinic Macclesfield Spire Regency Hospital Berkshire Warrington Spire Cheshire Hospital Reading Berkshire Independent Hospital Cleveland Spire Dunedin Hospital Norton Nuffield Health Tees Hospital Slough Spire Thames Valley Hospital Wexham Park Hospital Cornwall - Paragon Suite Truro Duchy Hospital Windsor BMI The Princess Margaret Hospital Cumbria Bristol Carlisle Caldew Hospital Bristol Spire Bristol Hospital Whitehaven West Cumberland Hospital Eye Hospital - Cumbrian Clinic General Hospital Nuffield Health Bristol Hospital Derbyshire Royal Hospital for Sick Children Derby Nuffield Health Derby Hospital Royal Infirmary Devon Buckinghamshire Barnstaple North Devon District Hospital Aylesbury Stoke Mandeville Hospital - Roborough Suite Great Missenden BMI The Chiltern Hospital Exeter Nuffield Health Exeter Hospital High Wycombe BMI The Shelburne Hospital Royal Devon & Exeter Hospital Plymouth Derriford Hospital - The Meavy Clinic Milton Keynes BMI The Saxon Clinic Nuffield Health Plymouth Hospital Cambridgeshire Torquay Mount Stuart Hospital Cambridge Addenbrookes Hospital Spire Cambridge Lea Hospital Dorset Nuffield Health Cambridge Hospital Bournemouth Nuffield Health Bournemouth -

National Cardiac Arrest Audit Participating Hospitals List England
Updated June 2014 National Cardiac Arrest Audit Participating hospitals list The total number of hospitals signed up to participate in NCAA is 177. England Avon, Gloucestershire and Wiltshire NCAA participants Cheltenham General Hospital Gloucestershire Hospitals NHS Foundation Trust Gloucestershire Royal Hospital Gloucestershire Hospitals NHS Foundation Trust Royal United Hospital Royal United Hospital Bath NHS Trust Southmead Hospital, Bristol North Bristol NHS Trust The Great Western Hospital Great Western Hospitals NHS Foundation Trust University Hospitals Bristol NHS Foundation Trust University Hospitals Bristol NHS Foundation Trust Non-NCAA participants Weston General Hospital Weston Area Health NHS Trust Birmingham and Black Country NCAA participants Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital Heart of England NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital Heart of England NHS Foundation Trust Manor Hospital Walsall Healthcare NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital Heart of England NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Non-NCAA participants Hereford County Hospital Wye Valley NHS Trust New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Supported by Resuscitation -

COVID-19 Briefing 19 June 2020
COVID-19 briefing 19 June 2020 This week: Face coverings for hospital settings Gordon’s Alive! - Veteran actor Brian Blessed praises NHS Men’s Health Week - Take Action on COVID-19 Learning Disability Week- Friendships during COVID-19 A Royal delivery to Frimley Life expectancy report highlights inequality Face coverings or masks now mandatory for all hospital settings and confined public spaces Frimley Health NHS Foundation Trust has introduced new measures to help prevent COVID-19 transmission amongst visitors, patients and staff. As of Monday, June 15, all patients and visitors must wear face coverings at all times at Frimley Park Hospital in Surrey; Wexham Park Hospital in Slough; Heatherwood Hospital in Ascot and all other community services run by the Trust. This follows an announcement made by the Secretary of State for Health and Social Care, whereby he said that all visitors and outpatients must wear face coverings while in a hospital setting, to reduce the risk of transmission in hospitals (nosocomial transmission). He also said that staff in hospitals in England must wear face masks. People infected with COVID-19 may have very mild symptoms, or none at all (asymptomatic) but can still transmit the virus to others without being aware of it. The new measures are therefore being introduced to keep visitors, patients, and staff safe. What does this mean for me? We can all play a role in reducing the spread of coronavirus and keeping our hospitals safe. If you are coming to hospital as a visitor or for planned outpatient care, it is important that you wear a face covering at all times. -

Centre Town/City Course
Centre Town/City Course Aberdeen Royal Infirmary ABERDEEN ATLS Addenbrookes Hospital CAMBRIDGE ATLS Airedale General Hospital KEIGHLEY ATLS Alexandra Hospital REDDITCH ATLS Ashford Hospital ASHFORD ATLS Basildon and Thurrock University Hospitals NHS Foundation Trust BASILDON ATLS Bedford Hospital BEDFORD ATLS Bradford Royal Infirmary BRADFORD ATLS Broomfield Hospital CHELMSFORD ATLS Chelsea and Westminster Hospital LONDON ATLS Cheltenham General Hospital CHELTENHAM ATLS Conquest Hospital ST. LEONARDS-ON-SEA ATLS Countess of Chester Hospital CHESTER ATLS County Durham and Darlington NHS Foundation Trust DURHAM ATLS Craigavon Area Hospital CRAIGAVON ATLS Crosshouse Hospital KILMARNOCK ATLS Croydon University Hospital THORNTON HEATH ATLS Cumberland Infirmary CARLISLE ATLS Dorset County Hospital DORCHESTER ATLS East Lancashire Hospitals NHS Trust BLACKBURN ATLS East Surrey Hospital REDHILL ATLS Eastbourne District General Hospital EASTBOURNE ATLS Frimley Park Hospital CAMBERLEY ATLS Glan Clwyd Hospital RHYL ATLS Glangwili General Hospital CARMARTHEN ATLS Guy's & St Thomas' NHS Foundation Trust LONDON ATLS Hillingdon Hospitals NHS Foundation Trust UXBRIDGE ATLS Hull University Teaching Hospitals NHS Trust HULL ATLS Ipswich Hospital NHS Trust IPSWICH ATLS James Cook University Hospital MIDDLESBROUGH ATLS James Paget University Hospital GREAT YARMOUTH ATLS King's College Hospital LONDON ATLS Kings Mill Hospital SUTTON-IN-ASHFIELD ATLS Kirklands Hospital GLASGOW ATLS Leeds Teaching Hospitals NHS Trust LEEDS ATLS Leicester Royal Infirmary LEICESTER -

Full Text Decision
Anticipated acquisition of Heatherwood and Wexham Park Hospitals NHS Foundation Trust by Frimley Park Hospital NHS Foundation Trust ME/6432-14 Summary 1. The parties notified the anticipated merger to the Office of Fair Trading (OFT) on 28 March 2014. The merger was investigated under the OFT’s administrative timetable1 by the Competition and Markets Authority (CMA) from 1 April.2 2. Frimley Park Hospital NHS Foundation Trust (FPH) and Heatherwood and Wexham Park Hospitals NHS Foundation Trust (HWPH) (together, the 'parties') both supply a range of hospital-based services (including elective and non- elective inpatient services) and diagnostics and outpatient services to patients across a wide area, including Hampshire, Surrey, and Berkshire. They also both provide some specialised services and private (fee-paying) services to patients. 3. The parties signed a memorandum of understanding on 7 May 2013 relating to a possible acquisition of HWPH by FPH (the 'merger'), following which heads of terms were signed on 1 May 2014. The parties engage in activities which constitute 'enterprises' within the meaning of the Enterprise Act 2002 (the 'Act') and which will cease to be distinct as a result of the Merger. In addition, the income of HWPH exceeded £70 million in the UK in 2012/13, thus the turnover test is met. The CMA therefore believes that it is or may be the case that arrangements are in progress or in contemplation which, if carried into effect, will result in the creation of a relevant merger situation. The CMA assessed the merger against the conditions of competition prevailing pre-merger. -

Alcohol Secondary Care Pathway
Alcohol services for Hampshire residents Secondary care pathway The most effective treatment for higher risk drinkers is specialist support Patient attends secondary care Patient admitted to secondary Screen for alcohol use using care who is also identified as AUDIT-C having Alcohol Dependence and/alcohol related disorders Patient is assessed for Patient has Patient has medical detoxification AUDIT score <8 AUDIT score 8+ (Lower Risk) Offer referral to Alcohol Give Brief Advice Nurse Service (ANS) who Give Brief Advice will oversee detox whilst in Offer referral to hospital and ensure referral Congratulate and Alcohol Nurse to Inclusion on discharge reinforce benefits Service (ANS) of lower risk drinking Patient rejects referral to Alcohol Nurse Service Signpost to NHS Patient accepts Choices, referral to Alcohol Change4Life Nurse Service Provide patient with “Choose Less option to self refer to Booze” Inclusion Patient receives support from ANS Signpost to online resources. Offer Extended Brief Intervention • Patients in hospital can be referred to the Alcohol Specialist Nurse Service – Royal County Hospital – Tel: 01962 825944 – Basingstoke and North Hampshire Hospital – Tel: 01256 313518 – Frimley Park Hospital » ED - 01252 649208 (Internal number 3208) » Wards - 01252 64209 (Internal number 3209) – Southampton General Hospital – Tel: 02381 205721 – Queen Alexandra Hospital – Tel: 02392 286000 Ext: 5403 • Patients can also self refer to Inclusion Recovery Hampshire Tel: 0300 124 0103 Email: [email protected] www.hants.gov.uk/publichealthservices -

Confidential Notes WESSEX CLINICAL SENATE COUNCIL STUDY DAY
Confidential Notes WESSEX CLINICAL SENATE COUNCIL STUDY DAY Notes of the Wessex Clinical Senate Council Study Day held on 13th March 2013 in the RNLI headquarters, Poole Present: Professor William Roche (WR) Clinical Senate Chair, Wessex Area Team, Stuart Ward (SW) Medical Director, NHS England Wessex, Nigel Watson (NW) GP, Frank Rust (FR) Patient & Public, Lesley Ayling, (LA) Clinical Director for Children and Families, West Hampshire CCG, , David Phillips (DP) Director of Public Health Dorset, Andrew Mortimore (AM) Director of Public Health, Southampton City Council, Simon Plint (SP) Dean, Health Education Wessex, Richard Jones (RJ) SCN Clinical Director, Cardiovascular Strategic Clinical Network, Matthew Hayes (MH) SCN Clinical Director, Cancer Strategic Clinical Network, Gary Connett (GC) Wessex Academic Health Science Network, Ranjit Mahanta (RM), Consultant Psychiatrist, Frimley Park Hospital, Suzanne Cunningham, (SC) Consultant Midwife, University Hospital, Southampton, Alyson O’Donnell, (AO) SCN Clinical Director, Maternity, Children and Young people Invitees: Dr David Phillips,(DP) Director of Public Health, Dorset, Margaret Allen, (MA) Deputy Director Review, Design & Delivery, NHS Dorset Clinical Commissioning Group, Jean O’Callaghan (JO) Jean O’Callaghan Chief Executive, Dorset County Hospital NHS Foundation Trust, Patricia Miller (PM) Director of Operations, Dorset County Hospital, Dr Angus Wood (AW) Deputy Medical Director, Poole Hospital NHS Foundation Trust, Dr Steve Wadams (SW) Consultant in Paediatrics, Poole Hospital