Confidential Notes WESSEX CLINICAL SENATE COUNCIL STUDY DAY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2017 Re-Audit of Red Cell & Platelet Transfusion in Adult Haematology
2016 Re-Audit of Patient Blood Management in adults undergoing elective, scheduled surgery 2017 Re-Audit of Red Cell & Platelet Transfusion in Adult Haematology patients South West RTC 2016 Re-Audit of Patient Blood Management in adults undergoing elective, scheduled surgery South West RTC Method • For this repeat audit, sites were asked to – identify all patients who were admitted and transfused in Sept, Oct and Nov 2016 for one or more of 14 selected surgical procedures – audit all consecutive cases with the minimum target of 45 patients, and a maximum of 70 • A list of OPCS4 codes was provided to help with patient identification Sample size: 339 patients from 15 sites Site Cases Dorset County Hospital NHS Foundation Trust 2 Gloucestershire Hospitals NHS Foundation Trust 11 Great Western Hospitals NHS Foundation Trust 38 North Bristol NHS Trust 31 Northern Devon Healthcare NHS Trust 9 Plymouth Hospitals NHS Trust 5 Poole Hospital NHS Foundation Trust 14 Royal Cornwall Hospitals NHS Trust 29 Royal Devon and Exeter NHS Foundation Trust 38 Royal United Hospitals Bath NHS Foundation Trust 25 Taunton and Somerset NHS Foundation Trust 23 The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust 21 University Hospitals Bristol NHS Foundation Trust 40 Weston Area Health NHS Trust 37 Yeovil District Hospital NHS Foundation Trust 16 Type of surgical procedure audited (1) e n ir o h l ev rs to e is D t r rn es B e c h h le u rt rt o lo o o o Type of surgical procedure (n=3897) National Dorset G Great Western N N Plymouth P Primary unilateral total hip replacement 16% (610) 0 6 13 4 2 0 0 Primary bilateral total hip replacement 1% (30) 0 0 0 0 0 0 0 Primary unilateral total knee replacement 9% (341) 0 0 4 2 0 0 0 Primary bilateral total knee replacement 1% (27) 0 0 0 0 0 0 0 Unilateral revision hip replacement 7% (258) 0 0 1 1 0 1 4 Unilateral revision knee replacement 2% (67) 0 0 0 4 0 0 0 Colorectal resection for any indication (open or laparoscopic) 8% (300) 0 0 1 0 0 0 1 Open arterial surgery e.g. -

Pacman TEMPLATE
Updated May 2020 National Cardiac Arrest Audit Participating Hospitals The total number of hospitals signed up to participate in NCAA is 194. England Birmingham and Black Country Participant Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital University Hospital Birmingham NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital University Hospital Birmingham NHS Foundation Trust Hereford County Hospital Wye Valley NHS Trust Manor Hospital Walsall Healthcare NHS Trust New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital University Hospital Birmingham NHS Foundation Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Central England Participant George Eliot Hospital George Eliot Hospital NHS Trust Glenfield Hospital University Hospitals of Leicester NHS Trust Kettering General Hospital Kettering General Hospital NHS Foundation Trust Leicester General Hospital University Hospitals of Leicester NHS Trust Leicester Royal Infirmary University Hospitals of Leicester NHS Trust Northampton General Hospital Northampton General Hospital NHS Trust Hospital of St Cross, Rugby University Hospitals Coventry and Warwickshire NHS Trust University Hospital Coventry University Hospitals Coventry -

National Cardiac Arrest Audit Participating Hospitals
Updated June 2018 National Cardiac Arrest Audit Participating Hospitals The total number of hospitals signed up to participate in NCAA is 197. England Birmingham and Black Country Non-participant New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Participant Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital Heart of England NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital Heart of England NHS Foundation Trust Hereford County Hospital Wye Valley NHS Trust Manor Hospital Walsall Healthcare NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital Heart of England NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Central England Participant George Eliot Hospital George Eliot Hospital NHS Trust Glenfield Hospital University Hospitals of Leicester NHS Trust Kettering General Hospital Kettering General Hospital NHS Foundation Trust Leicester General Hospital University Hospitals of Leicester NHS Trust Leicester Royal Infirmary University Hospitals of Leicester NHS Trust Northampton General Hospital Northampton General Hospital NHS Trust Hospital of St Cross, Rugby University Hospitals Coventry and Warwickshire NHS Trust University Hospital Coventry University Hospitals Coventry and Warwickshire NHS Trust -

Dorset Health Authority
FOREST HOLME HOSPICE REFERRAL FORM Phone Forest Holme on (01202 44) 8118 if you wish to discuss with a member of the team Email: [email protected] Patient’s name: Telephone number: Mobile number: Patient’s address with post code: Date of birth: NHS number: Hospital number: Access problems (key safe number etc.): Current location of patient: Patients must be aware of and agree to the referral. If patients lack capacity to consent, referral must be judged to be in their best interests. Patient aware of referral: yes no GP and GP surgery: GP aware of referral: yes no Main carer’s name: Relationship to patient: Contact number: Primary diagnosis: Date of diagnosis: Patient aware of diagnosis? yes no Estimated prognosis: less than 16 weeks more than 16 weeks Current problems or needs (see notes overleaf; tick all that apply): symptom control psychological support other Please specify particular symptoms or problem: Urgency: within 24 hours within 72 hours non-urgent What services would you like in the first instance? (tick all appropriate boxes) home visit by specialist nurse outpatient appointment with doctor home visit by doctor hospital inpatient assessment assessment by community palliative care occupational therapist admission to specialist palliative care unit advice by telephone – please phone 01202 448118 Referred by: Contact number: Date: Name: Position: 1 FOREST HOLME HOSPICE REFERRAL FORM Phone Forest Holme on (01202 44) 8118 if you wish to discuss with a member of the team Email: [email protected] The Palliative Care Service based at Forest Holme Hospice Forest Holme Hospice is a purpose built specialist palliative care unit which is part of Poole Hospital NHS Foundation Trust. -
ABCD Nationwide Audit of Freestyle Libre (FSL)
ABCD nationwide audit of FreeStyle Libre (FSL) Dr Harshal Deshmukh MRCP MPH PhD NIHR Clinical Lecturer in Endocrinology and Diabetes Dr Emma Wilmot Dr Chris Walton Dr Bob Ryder Prof Thozhukat Sathyapalan ABCD nationwide audit of FreeStyle Libre DISCLOSURES Disclosures • EW has received personal fees from Abbott Diabetes Care, Dexcom, Diasend, Eli Lilly, Medtronic, Novo Nordisk, Sanofi Aventis • BR has received speaker fees, and/or consultancy fees and/or educational sponsorships from AstraZeneca, BioQuest, GI Dynamics, Janssen, Novo Nordisk, Sanofi-Aventis and Takeda • HD TS and CW have no relevant disclosures Funding The ABCD nationwide Freestyle Libre audit is supported by a grant from Abbott UK. The audit was independently initiated and performed by ABCD, and the authors remain independent in the analysis and preparation of this report. ABCD nationwide audit of FreeStyle Libre • FreeStyle Libre is a flash glucose monitoring system which monitors interstitial glucose levels • Consists of a sensor with a microfilament, worn on the back of the arm and a hand- held reader • When the reader unit is passed over the sensor, it shows the interstitial glucose levels • The sensor lasts for 14 days, then needs to be replaced ABCD nationwide audit of FreeStyle Libre ABCD FSL Audit Main Objectives The ABCD FSL Audit aims to explore the impact of the FSL on the following: . HbA1c . Hypoglycaemia awareness . Resource utilisation: hospital admissions . User satisfaction . Diabetes related distress . Discontinuation rate and causes ABCD nationwide audit of FreeStyle Libre Methods ABCD nationwide audit of FreeStyle Libre • Audit conducted in 114 centres in the UK • A secure IT tool was developed on the NHS computer network, N3, to make this process as easy and user friendly as possible ABCD nationwide audit of FreeStyle Libre . -

List 2018 a 18/0347 8 Abelia Close, West End, Woking, Surrey, GU24 9PG 18/0115 24 Academy Close, Camberley, Surrey, GU15 4BU
List 2018 A 18/0347 8 Abelia Close, West End, Woking, Surrey, GU24 9PG 18/0115 24 Academy Close, Camberley, Surrey, GU15 4BU 18/0491 Units 1-5 Admiralty Way, Camberley, Surrey, GU15 3DT 18/0694 Unit 7, Phase 4 Albany Park, Camberley, Surrey, GU16 7PL 18/0806 16 Albert Road, Bagshot, Surrey, GU19 5QJ 18/0630 1 Alexandra Avenue, Camberley, Surrey, GU15 3BG 18/1015 Sandhurst Chalet, Alfriston Road, Deepcut, Camberley, Surrey, GU16 6QS 18/0521 The Surgery, 39 All Saints Road, Lightwater, Surrey, GU18 5SQ 18/0383 22 Alpha Road, Chobham, Woking, Surrey, GU24 8NF 18/0860 5 Alphington Avenue, Frimley, CAMBERLEY, GU16 8LA 18/0024 31 Alphington Avenue, Frimley, Camberley, Surrey, GU16 8LL 18/0063 45 Alphington Avenue, Frimley, Camberley, Surrey, GU16 8LL 18/0717 8 Amber Hill, Camberley, Surrey, GU15 1EB 18/0673 27 Ambleside Close, Mytchett, Camberley, Surrey, GU16 6DG 18/0394 1 Ambleside Road, Lightwater, Surrey, Gu18 5TA 18/0844 25 Ambleside Road, Lightwater, GU18 5TA 18/0199 27 Ambleside Road, Lightwater, Surrey, GU16 6DG 18/0392 32A Ambleside Road, Lightwater, Surrey, GU16 5TA 18/0657 32A Ambleside Road, Lightwater, Surrey, GU16 5TA 18/0271 87 Ambleside Road, Lightwater, Surrey, GU18 5UH 18/0699 137 Ambleside Road, Lightwater, GU18 5UL 18/0345 142 Ambleside Road, Lightwater, Surrey, GU18 5UN 18/0037 153 Ambleside Road, Lightwater, Surrey, GU18 5UN 18/0577 11 Anderson Place, Bagshot, Surrey, GU19 5LX 18/0060 6 Ardrossan Avenue, Camberley, Surrey, GU15 1DD 18/0830 15 Arthur Close, Bagshot, GU19 5QT 18/0889 16 Arundel Road, Camberley, GU15 1DL -

Royal Bournemouth and Poole Hospitals Mitigate Cyber Risk Through a ‘Single Pane of Glass’ Network View and Near Real-Time Risk Reporting
Royal Bournemouth and Poole Hospitals mitigate cyber risk through a ‘single pane of glass’ network view and near real-time risk reporting NHS IT teams typically employ a variety of tools and Customer Poole Hospital NHS Foundation Trust technologies to identify risks and test the effectiveness (PHFT) and The Royal Bournemouth and of their security controls. As a result, ‘moment-in- Christchurch Hospitals NHS Foundation Trust (RBCH). time’ reports are pulled from disparate systems that require data to be cobbled together to understand the Type of NHS Organisation organisation’s overall security posture. It’s an approach Two acute trusts with a shared IT which is reactive, labour-intensive and leaves the function. organisation open to risk. The IT team at Poole Hospital Customer Since NHS Foundation (PHFT) and The Royal Bournemouth 2007. and Christchurch Hospitals NHS Foundation Trust (RBCH) wanted to reduce its reliance on such an Challenge PHFT and RBCH wanted to stop its approach and find a more proactive way to manage its reliance on point-in-time reports from cyber security. disparate systems to reduce its exposure to cyber risk, as well as find a better way to manage and track its stock inventory. Solution An intuitive dashboard provides a single source of near real-time insight into the Trusts’ devices, applications and security controls enabling time-savings, enhanced security and greater understanding of the Trusts’ overall risk posture, whilst also displacing legacy inventory systems. Customer Case Study | Poole Hospital NHS Foundation Trust and The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust Poole Hospital NHS Foundation Trust (PHFT) is an acute general hospital with a 24-hour major accident and emergency department. -

UK Clinical Teaching Fellows Forum 2019
UK Clinical Teaching Fellows Forum 2019 In partnership with The Academy of Medical Educators Saturday 8 June 2019 Postgraduate Education Centre, Frimley Park Hospital, Surrey IMPROVING CARE THROUGH TEACHING EXCELLENCE Academy of Medical Educators, Neuadd Meirionnydd, Heath Park, Cardiff CF14 4YS Email: [email protected] Telephone: 02920 687206 Charity no: 1128988 Company no: 5965178 www.medicaleducators.org Programme Time Speaker Session Venue 9.15 - 9.45 Registration and coffee (Entrance hall) 9.45 – 10.00 Dr James Fisher & Introduction Lecture Dr Lewis Hendon-John Theatre Frimley Health NHS Foundation Trust 10.00– 10.15 Neil Dardis Welcome Talk - Engaging the board Lecture Theatre Chief Executive, Frimley Health NHS Foundation Trust 10.15 - 10.35 Professor Jacky Hayden The Current State of Medical Education Lecture Theatre President Academy of Medical Educators 10.35 - 11.05 Short Presentations (plenary) Lecture Theatre The Great Escape: Exploring the impact of escape rooms in medical education Webster R, Durkan N, Leylabi R, Smethurst K, Royal Victoria Infirmary Implementing wilderness medicine training for undergraduate medical education: a success story Schulz J, Warrington J, Maguire C, Georgi T, Hearn R, King’s College London Immersive Confusional Experience of Delirium (ICED): The use of an interactive, web-based game to teach undergraduates about delirium Webb L, van't Hoff C, Jacobs C, Finnegan D, Ipe A, Jones K, Great Western Hospital 11.05 – 11.15 Rapid Poster Summary Session (plenary) 11.15 – 11.45 Coffee and biscuits, -
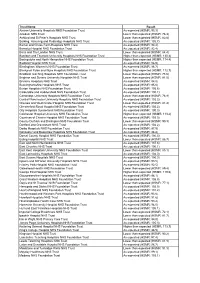
HSMR June09 Choices
Trust Name Result Aintree University Hospitals NHS Foundation Trust As expected (HSMR: 93.3) Airedale NHS Trust Lower than expected (HSMR: 76.3) Ashford and St Peter's Hospitals NHS Trust Lower than expected (HSMR: 82.8) Barking, Havering and Redbridge Hospitals NHS Trust As expected (HSMR: 105.7) Barnet and Chase Farm Hospitals NHS Trust As expected (HSMR: 94.4) Barnsley Hospital NHS Foundation Trust As expected (HSMR: 92.4) Barts and The London NHS Trust Lower than expected (HSMR: 84.4) Basildon and Thurrock University Hospitals NHS Foundation Trust Higher than expected (HSMR: 130.4) Basingstoke and North Hampshire NHS Foundation Trust Higher than expected (HSMR: 114.4) Bedford Hospital NHS Trust As expected (HSMR: 96.9) Birmingham Women's NHS Foundation Trust As expected (HSMR: 96.7) Blackpool Fylde and Wyre Hospitals NHS Foundation Trust Higher than expected (HSMR: 112.7) Bradford Teaching Hospitals NHS Foundation Trust Lower than expected (HSMR: 78.6) Brighton and Sussex University Hospitals NHS Trust Lower than expected (HSMR: 81.5) Bromley Hospitals NHS Trust As expected (HSMR: 94.0) Buckinghamshire Hospitals NHS Trust As expected (HSMR: 95.6) Burton Hospitals NHS Foundation Trust As expected (HSMR: 105.6) Calderdale and Huddersfield NHS Foundation Trust As expected (HSMR: 100.1) Cambridge University Hospitals NHS Foundation Trust Lower than expected (HSMR: 78.9) Central Manchester University Hospitals NHS Foundation Trust As expected (HSMR: 102.2) Chelsea and Westminster Hospital NHS Foundation Trust Lower than expected (HSMR: -

Suspected Cancer Fast Track Referral
Suspected Cancer Frimley Health Fast Track Referral NHS Foundation Trust IMPORTANT information about your appointment Your doctor/dentist has requested you are Hospital addresses seen by a specialist or have a test within the next two weeks. You will be seen at one of the following hospitals: You may be offered the opportunity to book an Frimley Park Sites: appointment before you leave the surgery, or will be offered an appointment by telephone Frimley Park Hospital at the earliest opportunity. Portsmouth Road, Surrey, GU16 7UJ It is important you make yourself available Aldershot Centre for Health and attend this appointment. Hospital Hill, Aldershot, Hampshire GU11 1AY Should I be worried? Fleet Community Hospital The need for an early appointment does not mean Church Road, Fleet, Hampshire, GU51 4LZ you have cancer, however your doctor/dentist would like you to be seen by a specialist as soon as Farnham Hospital possible. Hale Road, Farnham, Surrey, GU9 9QL What is a Suspected Cancer The Bracknell Clinic Fast Track referral? Eastern Gate, Brants Bridge, Bracknell, Berkshire This referral is to ensure anyone with symptoms/ RG12 9BG initial test results that may be suspicious of cancer will be seen by a specialist or have a specialist test Heatherwood and Wexham Sites: within two weeks. Wexham Park Hospital, The aim is to exclude cancer or provide diagnosis, Wexham Street, Slough, SL2 4HL intervention and treatment, if required, at the earliest opportunity. Heatherwood Hospital, London Road, Ascot, SL5 8AA What happens now? King Edward VII Hospital, St Leonards Road, Windsor, SL4 3DP • You will be helped to book an appointment before you leave the surgery or you may receive St Mark’s Hospital, an appointment by telephone, please accept a St Mark’s Road, Maidenhead, SL6 6DU telephone call from an unknown number. -

Poole Hospital NHS Foundation Trust
Poole Hospital NHS Foundation Trust Use of Resources report Date of site visit: Longfleet Road, Poole, Dorset BH15 2JB 6 October 2017 Tel: 01202 665511 Date of publication: www.poole.nhs.uk 2 August 2018 This report describes NHS Improvement’s assessment of how effectively this trust uses its resources. It is based on a combination of data on the trust’s performance over the previous 12 months, our local intelligence, the trust’s commentary on its performance, and qualitative evidence collected during a site visit comprised of a series of structured conversations with the trust's leadership team. How effectively is the trust using its resources? Good How we carried out this assessment The aim of Use of Resources assessments is to understand how effectively providers are using their resources to provide high quality, efficient and sustainable care for patients. The assessment team has, according to the published framework, examined the trust’s performance over the previous 12 months against a small number of initial metrics, alongside local intelligence from NHS Improvement’s day-to-day interactions with the trust, and the trust’s own commentary and information on its performance. The team conducted a dedicated site visit to engage with key staff using key lines of enquiry (KLOEs) and prompt questions in the areas of clinical services; people; clinical support services; corporate services, procurement, estates and facilities; and finance. All KLOEs, initial metrics and prompts can be found in the Use of Resources assessment framework. We visited the trust on 6 October 2017 where we met the trust’s leadership for discussions based on key lines of enquiry and prompts. -

Poole Hospital N.H.S
Dorset Family Information Directory My Shortlist 0 Children & Young People's Epilepsy Service - Poole Hospital N.H.S. Epilepsy is a common chronic neurological condition and can happen at any age. In the UK there are an estimated 60,000 children and young people under the age of 18 years that have epilepsy.Many children and young people will grow out of their epilepsy. It is a hospital based service with community support delivered by the epilepsy specialist nurse. We hold a wide range of children and young perople's epiliepsy clinics. We work with children up to the age of 16 if they attend main stream schools and young people with special needs up to the age of 19. Contact Website http://www.poole.nhs.uk/a-z-services/c/childrens- epilepsy-service.aspx Venue Venue address Poole General Hospital Longfleet Road Poole Dorset Postcode BH15 2JB Locality East Dorset Service Details Additional Please see our website for further information including Information referrals, services and clinics. Referral We welcome referrals from all health care services and information health professionals including your GP, the emergency department, following acute hospital admission or other general and community consultants. If you have any concerns about your child, contact your GP who can refer you to a specialist. Related Links Epilepsy Action Epilepsy Society Medicines for Children Some activities and family support services listed in our directory may be cancelled, postponed, or running in a different way due to coronavirus restrictions. Please contact providers to check for information about any changes..