Poole Hospital NHS Foundation Trust
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2017 Re-Audit of Red Cell & Platelet Transfusion in Adult Haematology
2016 Re-Audit of Patient Blood Management in adults undergoing elective, scheduled surgery 2017 Re-Audit of Red Cell & Platelet Transfusion in Adult Haematology patients South West RTC 2016 Re-Audit of Patient Blood Management in adults undergoing elective, scheduled surgery South West RTC Method • For this repeat audit, sites were asked to – identify all patients who were admitted and transfused in Sept, Oct and Nov 2016 for one or more of 14 selected surgical procedures – audit all consecutive cases with the minimum target of 45 patients, and a maximum of 70 • A list of OPCS4 codes was provided to help with patient identification Sample size: 339 patients from 15 sites Site Cases Dorset County Hospital NHS Foundation Trust 2 Gloucestershire Hospitals NHS Foundation Trust 11 Great Western Hospitals NHS Foundation Trust 38 North Bristol NHS Trust 31 Northern Devon Healthcare NHS Trust 9 Plymouth Hospitals NHS Trust 5 Poole Hospital NHS Foundation Trust 14 Royal Cornwall Hospitals NHS Trust 29 Royal Devon and Exeter NHS Foundation Trust 38 Royal United Hospitals Bath NHS Foundation Trust 25 Taunton and Somerset NHS Foundation Trust 23 The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust 21 University Hospitals Bristol NHS Foundation Trust 40 Weston Area Health NHS Trust 37 Yeovil District Hospital NHS Foundation Trust 16 Type of surgical procedure audited (1) e n ir o h l ev rs to e is D t r rn es B e c h h le u rt rt o lo o o o Type of surgical procedure (n=3897) National Dorset G Great Western N N Plymouth P Primary unilateral total hip replacement 16% (610) 0 6 13 4 2 0 0 Primary bilateral total hip replacement 1% (30) 0 0 0 0 0 0 0 Primary unilateral total knee replacement 9% (341) 0 0 4 2 0 0 0 Primary bilateral total knee replacement 1% (27) 0 0 0 0 0 0 0 Unilateral revision hip replacement 7% (258) 0 0 1 1 0 1 4 Unilateral revision knee replacement 2% (67) 0 0 0 4 0 0 0 Colorectal resection for any indication (open or laparoscopic) 8% (300) 0 0 1 0 0 0 1 Open arterial surgery e.g. -

Pacman TEMPLATE
Updated May 2020 National Cardiac Arrest Audit Participating Hospitals The total number of hospitals signed up to participate in NCAA is 194. England Birmingham and Black Country Participant Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital University Hospital Birmingham NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital University Hospital Birmingham NHS Foundation Trust Hereford County Hospital Wye Valley NHS Trust Manor Hospital Walsall Healthcare NHS Trust New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital University Hospital Birmingham NHS Foundation Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Central England Participant George Eliot Hospital George Eliot Hospital NHS Trust Glenfield Hospital University Hospitals of Leicester NHS Trust Kettering General Hospital Kettering General Hospital NHS Foundation Trust Leicester General Hospital University Hospitals of Leicester NHS Trust Leicester Royal Infirmary University Hospitals of Leicester NHS Trust Northampton General Hospital Northampton General Hospital NHS Trust Hospital of St Cross, Rugby University Hospitals Coventry and Warwickshire NHS Trust University Hospital Coventry University Hospitals Coventry -

Dorset Health Authority
FOREST HOLME HOSPICE REFERRAL FORM Phone Forest Holme on (01202 44) 8118 if you wish to discuss with a member of the team Email: [email protected] Patient’s name: Telephone number: Mobile number: Patient’s address with post code: Date of birth: NHS number: Hospital number: Access problems (key safe number etc.): Current location of patient: Patients must be aware of and agree to the referral. If patients lack capacity to consent, referral must be judged to be in their best interests. Patient aware of referral: yes no GP and GP surgery: GP aware of referral: yes no Main carer’s name: Relationship to patient: Contact number: Primary diagnosis: Date of diagnosis: Patient aware of diagnosis? yes no Estimated prognosis: less than 16 weeks more than 16 weeks Current problems or needs (see notes overleaf; tick all that apply): symptom control psychological support other Please specify particular symptoms or problem: Urgency: within 24 hours within 72 hours non-urgent What services would you like in the first instance? (tick all appropriate boxes) home visit by specialist nurse outpatient appointment with doctor home visit by doctor hospital inpatient assessment assessment by community palliative care occupational therapist admission to specialist palliative care unit advice by telephone – please phone 01202 448118 Referred by: Contact number: Date: Name: Position: 1 FOREST HOLME HOSPICE REFERRAL FORM Phone Forest Holme on (01202 44) 8118 if you wish to discuss with a member of the team Email: [email protected] The Palliative Care Service based at Forest Holme Hospice Forest Holme Hospice is a purpose built specialist palliative care unit which is part of Poole Hospital NHS Foundation Trust. -

Royal Bournemouth and Poole Hospitals Mitigate Cyber Risk Through a ‘Single Pane of Glass’ Network View and Near Real-Time Risk Reporting
Royal Bournemouth and Poole Hospitals mitigate cyber risk through a ‘single pane of glass’ network view and near real-time risk reporting NHS IT teams typically employ a variety of tools and Customer Poole Hospital NHS Foundation Trust technologies to identify risks and test the effectiveness (PHFT) and The Royal Bournemouth and of their security controls. As a result, ‘moment-in- Christchurch Hospitals NHS Foundation Trust (RBCH). time’ reports are pulled from disparate systems that require data to be cobbled together to understand the Type of NHS Organisation organisation’s overall security posture. It’s an approach Two acute trusts with a shared IT which is reactive, labour-intensive and leaves the function. organisation open to risk. The IT team at Poole Hospital Customer Since NHS Foundation (PHFT) and The Royal Bournemouth 2007. and Christchurch Hospitals NHS Foundation Trust (RBCH) wanted to reduce its reliance on such an Challenge PHFT and RBCH wanted to stop its approach and find a more proactive way to manage its reliance on point-in-time reports from cyber security. disparate systems to reduce its exposure to cyber risk, as well as find a better way to manage and track its stock inventory. Solution An intuitive dashboard provides a single source of near real-time insight into the Trusts’ devices, applications and security controls enabling time-savings, enhanced security and greater understanding of the Trusts’ overall risk posture, whilst also displacing legacy inventory systems. Customer Case Study | Poole Hospital NHS Foundation Trust and The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust Poole Hospital NHS Foundation Trust (PHFT) is an acute general hospital with a 24-hour major accident and emergency department. -

Poole Hospital N.H.S
Dorset Family Information Directory My Shortlist 0 Children & Young People's Epilepsy Service - Poole Hospital N.H.S. Epilepsy is a common chronic neurological condition and can happen at any age. In the UK there are an estimated 60,000 children and young people under the age of 18 years that have epilepsy.Many children and young people will grow out of their epilepsy. It is a hospital based service with community support delivered by the epilepsy specialist nurse. We hold a wide range of children and young perople's epiliepsy clinics. We work with children up to the age of 16 if they attend main stream schools and young people with special needs up to the age of 19. Contact Website http://www.poole.nhs.uk/a-z-services/c/childrens- epilepsy-service.aspx Venue Venue address Poole General Hospital Longfleet Road Poole Dorset Postcode BH15 2JB Locality East Dorset Service Details Additional Please see our website for further information including Information referrals, services and clinics. Referral We welcome referrals from all health care services and information health professionals including your GP, the emergency department, following acute hospital admission or other general and community consultants. If you have any concerns about your child, contact your GP who can refer you to a specialist. Related Links Epilepsy Action Epilepsy Society Medicines for Children Some activities and family support services listed in our directory may be cancelled, postponed, or running in a different way due to coronavirus restrictions. Please contact providers to check for information about any changes.. -

BMC Neurology
BMC Neurology This Provisional PDF corresponds to the article as it appeared upon acceptance. Fully formatted PDF and full text (HTML) versions will be made available soon. Multi-centre parallel arm randomised controlled trial to assess the effectiveness and cost-effectiveness of a group-based cognitive behavioural approach to managing fatigue in people with multiple sclerosis. BMC Neurology 2010, 10:43 doi:10.1186/1471-2377-10-43 Peter W Thomas ([email protected]) Sarah Thomas ([email protected]) Paula Kersten ([email protected]) Rosemary Jones ([email protected]) Alison Nock ([email protected]) Vicky Slingsby ([email protected]) Colin Green ([email protected]) Roger Baker ([email protected]) Kathleen Galvin ([email protected]) Charles Hillier ([email protected]) ISSN 1471-2377 Article type Study protocol Submission date 28 March 2010 Acceptance date 16 June 2010 Publication date 16 June 2010 Article URL http://www.biomedcentral.com/1471-2377/10/43 Like all articles in BMC journals, this peer-reviewed article was published immediately upon acceptance. It can be downloaded, printed and distributed freely for any purposes (see copyright notice below). Articles in BMC journals are listed in PubMed and archived at PubMed Central. For information about publishing your research in BMC journals or any BioMed Central journal, go to http://www.biomedcentral.com/info/authors/ © 2010 Thomas et al. , licensee BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. -

TRUST BOARD MEETING in PUBLIC Wednesday 25 March 2020 at 09
TRUST BOARD MEETING IN PUBLIC Wednesday 25 March 2020 At 09:30 VENUE: Queen Alexandra Hospital, Southwick Hill Road, Cosham, Portsmouth PLEASE NOTE: Public attendance is not allowed at this event given current guidance 1 of 133 2 of 133 TRUST BOARD MEETING IN PUBLIC Wednesday 25th March 2020 09:30 – 12.30 Oasis Centre, Queen Alexandra Hospital, Southwick Hill Road, Cosham PO6 3LY A G E N D A Item Time Item Enclosure Presented No. Y/N & by Number 048.20 09.30 Welcome, Apologies and Declaration of N Chair Interests (to ascertain whether any Board Member has any conflict of interest with any items on the Agenda) Minutes of the last meeting – 26th February 049.20 09.32 1 Chair 2020 050.20 09.35 Matters Arising/Summary of agreed actions 2 Chair 051.20 09.42 Notification of any other business N/A Chair 052.20 09.45 Chair’s opening remarks N/A Chair 053.20 09.55 Chief Executive’s Report 3 CEO STRATEGY 054.20 10.10 Operating Plan 2020 – 21 4 DSP 055.20 10.30 NHS Improvement Undertakings 5 DGR FINANCE AND INFRASTRUCTURE Finance and Infrastructure Committee feedback Committee 056.20 10.35 25th February 2020 (for information) 6 Chair 17th March 2020 o Operating Budget 2020 – 21 057.20 10.45 Financial performance report analysis N** CFO QUALITY, SAFETY AND PERFORMANCE Quality and Performance Committee feedback Committee 058.20 10.55 19th March 2020 7 Chair o Safer Staffing o Information Governance Toolkit o Trust response to Paterson Inquiry 3 of 133 Safety, quality and operational performance MD / COO 059.20 11.05 N** report analysis / CN WORKFORCE -

Palliative Care Clinical Data Set: Evaluation Report
National End of Life Care Intelligence Network Palliative care clinical data set Evaluation report V1.0/ December 2016 Palliative care clinical data set: evaluation report About Public Health England Public Health England exists to protect and improve the nation's health and wellbeing, and reduce health inequalities. We do this through world-class science, knowledge and intelligence, advocacy, partnerships and the delivery of specialist public health services. We are an executive agency of the Department of Health, and are a distinct delivery organisation with operational autonomy to advise and support government, local authorities and the NHS in a professional independent manner. Public Health England Wellington House 133-155 Waterloo Road London SE1 8UG Tel: 020 7654 8000 www.gov.uk/phe Twitter: @PHE_uk Facebook: www.facebook.com/PublicHealthEngland About NHS England NHS England leads the National Health Service (NHS) in England. They set the priorities and direction of the NHS and encourage and inform the national debate to improve health and care. They want everyone to have greater control of their health and their wellbeing, and to be supported to live longer, healthier lives by high quality health and care services that are compassionate, inclusive and constantly improving. Prepared by: National End of Life Care Intelligence Network For queries relating to this document, please contact: [email protected] © Crown copyright 2016 You may re-use this information (excluding logos) free of charge in any format or medium, under the terms of the Open Government Licence v3.0. To view this licence, visit OGL or email [email protected]. -

National Cardiac Arrest Audit Participating Hospitals List England
Updated June 2014 National Cardiac Arrest Audit Participating hospitals list The total number of hospitals signed up to participate in NCAA is 177. England Avon, Gloucestershire and Wiltshire NCAA participants Cheltenham General Hospital Gloucestershire Hospitals NHS Foundation Trust Gloucestershire Royal Hospital Gloucestershire Hospitals NHS Foundation Trust Royal United Hospital Royal United Hospital Bath NHS Trust Southmead Hospital, Bristol North Bristol NHS Trust The Great Western Hospital Great Western Hospitals NHS Foundation Trust University Hospitals Bristol NHS Foundation Trust University Hospitals Bristol NHS Foundation Trust Non-NCAA participants Weston General Hospital Weston Area Health NHS Trust Birmingham and Black Country NCAA participants Alexandra Hospital Worcestershire Acute Hospitals NHS Trust Birmingham Heartlands Hospital Heart of England NHS Foundation Trust City Hospital Sandwell and West Birmingham Hospitals NHS Trust Good Hope Hospital Heart of England NHS Foundation Trust Manor Hospital Walsall Healthcare NHS Trust Russells Hall Hospital The Dudley Group of Hospitals NHS Trust Sandwell General Hospital Sandwell and West Birmingham Hospitals NHS Trust Solihull Hospital Heart of England NHS Foundation Trust Worcestershire Royal Hospital Worcestershire Acute Hospitals NHS Trust Non-NCAA participants Hereford County Hospital Wye Valley NHS Trust New Cross Hospital The Royal Wolverhampton Hospitals NHS Trust Queen Elizabeth Hospital, Birmingham University Hospital Birmingham NHS Foundation Trust Supported by Resuscitation -
Provider Section
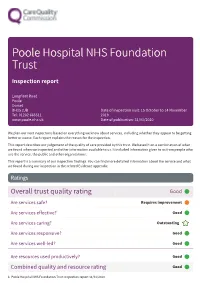
Poole Hospital NHS Foundation Trust Inspection report Longfleet Road Poole Dorset BH15 2JB Date of inspection visit: 15 October to 14 November Tel: 01202 665511 2019 www.poole.nhs.uk Date of publication: 31/01/2020 We plan our next inspections based on everything we know about services, including whether they appear to be getting better or worse. Each report explains the reason for the inspection. This report describes our judgement of the quality of care provided by this trust. We based it on a combination of what we found when we inspected and other information available to us. It included information given to us from people who use the service, the public and other organisations. This report is a summary of our inspection findings. You can find more detailed information about the service and what we found during our inspection in the related Evidence appendix. Ratings Overall trust quality rating Good ––– Are services safe? Requires improvement ––– Are services effective? Good ––– Are services caring? Outstanding Are services responsive? Good ––– Are services well-led? Good ––– Are resources used productively? Good ––– Combined quality and resource rating Good ––– 1 Poole Hospital NHS Foundation Trust Inspection report 31/01/2020 Summary of findings We rated well-led (leadership) from our inspection of trust management, taking into account what we found about leadership in individual services. We rated other key questions by combining the service ratings and using our professional judgement. Background to the trust Poole Hospital NHS Foundation Trust operates from Poole Hospital, located close to the centre of the town of Poole in Dorset, and provides acute services for the local population of around 500,000 people. -

ESR User Notice
UNdw275 Electronic Staff Record Programme 1 of 2 USER NOTICE 08th DEC 2020 Title Data Warehouse – Organisational Changes Purpose The purpose of this user notice is to inform users of Data Warehouse Organisational Changes Intended All Data Warehouse Users Audience SUBJECT To advise Data Warehouse users of the following Organisational changes. DETAIL Organisation Updates The following changes are being made to the Data Warehouse. These changes will not become effective until after the next Data Warehouse Load which is scheduled for completion at 08:00 on Monday 14th December 2020. The following Organisation names have changed within Data Warehouse. VPD Current Name New Name 153 ROYAL BOURNEMOUTH AND CHRISTCHURCH UNIVERSITY HOSPITALS DORSET NHS HOSPITALS NHS FOUNDATION TRUST FOUNDATION TRUST 428 POOLE HOSPITAL NHS FOUNDATION TRUST UNIVERSITY HOSPITALS DORSET NHS FOUNDATION TRUST The following Organisation EA Codes have been changed. VPD Organisation Name Current EA Code New EA Code 153 ROYAL BOURNEMOUTH AND RDZ R0D CHRISTCHURCH HOSPITALS NHS FOUNDATION TRUST 428 POOLE HOSPITAL NHS FOUNDATION RD3 R0D TRUST _______________________________________________________________________________________________________________ NOT PROTECTIVELY MARKED UNdw275 - Data Warehouse – Organisational Changes 2020 08/12/2020 UNdw275 Electronic Staff Record Programme 2 of 2 USER NOTICE 08th DEC 2020 Title Data Warehouse – Organisational Changes Purpose The purpose of this user notice is to inform users of Data Warehouse Organisational Changes Intended All Data -
What Matters to People Using Poole Hospital Accident & Emergency?
What matters to people using Poole Hospital Accident & Emergency? Local health and social care shaped by you 1 What matters to people using Poole Hospital A&E? Contents Page Introduction 3 Background 3 What we did 4 Who we spoke to 4 What people told us • Communication 5 • Waiting times 5 • Local hospital services 6 • Staff 6 • Environment 6 • Case study I 6 • Case study II 7 Recommendations 7 Next steps 8 Stakeholder’s response 8 Thank you 8 © Healthwatch Dorset (published February 2020) The material must be acknowledged as Healthwatch Dorset copyright and the document title specified. Where third party material has been identified, permission from the respective copyright holder must be sought. Any enquiries regarding this publication should be sent to us at [email protected] You can download this publication from healthwatchdorset.co.uk Healthwatch Dorset 2 Introduction Healthwatch Dorset is the county’s independent health and social care champion. It exists to ensure that people are at the heart of care. A dedicated team of staff and volunteers listen to what people like about local health and social care services, and what could be improved. These views are then shared with the decision-making organisations, so together a real difference can be made. This report is an example of how views are shared. Background Healthwatch England has been helping NHS England to understand the potential impact of new Accident and Emergency targets by finding out what matters most to patients and the public when it comes to A&E. The ongoing national review of A&E performance measures offers hospitals and their staff an opportunity to consider how targets align with patient priorities, and how data gathered as part of national performance reporting can be used in innovative ways to improve patient experience.