Stapedectomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CASE REPORT Resolution of Delayed Sudden Sensorineural Hearing Loss After Stapedectomy
The Mediterranean Journal of Otology CASE REPORT Resolution of Delayed Sudden Sensorineural Hearing Loss After Stapedectomy: A Case Report and Review of the Literature Noam Yehudai, MD, Michal Luntz, MD From the Department of Significant sensorineural hearing loss may develop immediately after suc- Otolaryngology, Head and Neck cessful stapedectomy but sometimes occurs months or even years later. Surgery, Bnai-Zion Medical The rate of recovery from that disorder has not been determined. Several Center, Technion-Israel School of Technology, Haifa, Israel reports in the 1960s described patients with delayed sensorineural hear- ing loss, but that entity has not been mentioned in the English-language Correspondence literature for the last 30 years. We present a review of the literature on this Michal Luntz, MD postsurgical auditory complication and describe a patient with delayed Department of Otolaryngology, Head and Neck Surgery poststapedectomy sensorineural hearing loss that developed 15 months Bnai-Zion Medical Center, after surgery and resolved completely after treatment with an oral steroid. Technion-Israel School of Technology 47 Golomb St, PO Box 4940, Haifa 31048, Israel Phone: 972-4-8359544 Fax: 972-4-8361069 E-mail: [email protected] Submitted: 05 February, 2006 Revised: 07 May, 2006 Accepted: 09 May, 2006 Mediterr J Otol 2006; 3: 156-160 Copyright 2005 © The Mediterranean Society of Otology and Audiology 156 Resolution of Delayed Sudden Sensorineural Hearing Loss After Stapedectomy: A Case Report and Review of the Literature -
A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: a Clinical Study
Int Adv Otol 2014; 10(2): 102-6 • DOI: 10.5152/iao.2014.40 Original Article A Post-Tympanoplasty Evaluation of the Factors Affecting Development of Myringosclerosis in the Graft: A Clinical Study Can Özbay, Rıza Dündar, Erkan Kulduk, Kemal Fatih Soy, Mehmet Aslan, Hüseyin Katılmış Department of Otorhinolaryngology, Şifa University Faculty of Medicine, İzmir, Turkey (CÖ) Department of Otorhinolaryngology, Mardin State Hospital, Mardin, Turkey (RD, EK, KFS, MA) Department of Otorhinolaryngology, Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Turkey (HK) OBJECTIVE: Myringosclerosis (MS) is a pathological condition characterized by hyaline degeneration and calcification of the collagenous structure of the fibrotic layer of the tympanic membrane, which may develop after trauma, infection, or inflammation as myringotomy, insertion of a ventila- tion tube, or myringoplasty. The aim of our study was to both reveal and evaluate the impact of the factors that might be effective on the post-tym- panoplasty development of myringosclerosis in the graft. MATERIALS and METHODS: In line with this objective, a total of 108 patients (44 males and 64 females) aged between 11 and 66 years (mean age, 29.5 years) who had undergone type 1 tympanoplasty (TP) with an intact canal wall technique and type 2 TP, followed up for an average of 38.8 months, were evaluated. In the presence of myringosclerosis, in consideration of the tympanic membrane (TM) quadrants involved, the influential factors were analyzed in our study, together with the development of myringosclerosis, including preoperative factors, such as the presence of myringosclerosis in the residual and also contralateral tympanic membrane, extent and location of the perforation, and perioperative factors, such as tympanosclerosis in the middle ear and mastoid cavity, cholesteatoma, granulation tissue, and type of the operation performed. -
Auditory Brainstem Response Latency in Noise As a Marker of Cochlear Synaptopathy
The Journal of Neuroscience, March 30, 2016 • 36(13):3755–3764 • 3755 Systems/Circuits Auditory Brainstem Response Latency in Noise as a Marker of Cochlear Synaptopathy X Golbarg Mehraei,1,2 XAnn E. Hickox,1,4 X Hari M. Bharadwaj,2,7 Hannah Goldberg,1 Sarah Verhulst,2,6 M. Charles Liberman,1,4,5 and XBarbara G. Shinn-Cunningham2,3 1Program in Speech and Hearing Bioscience and Technology, Harvard University/Massachusetts Institute of Technology, Cambridge, Massachusetts 02139, 2Center for Computational Neuroscience and Neural Technology, Boston University, Boston, Massachusetts 02215, 3Department of Biomedical Engineering, Boston University, Boston, Massachusetts 02215, 4Eaton-Peabody Laboratory, Massachusetts Eye and Ear Infirmary, Boston, Massachusetts 02114, 5Department of Otology and Laryngology, Harvard Medical School, Boston, Massachusetts 02114, 6Cluster of Excellence Hearing4All and Medical Physics, Department of Medical Physics and Acoustics, Oldenburg University, 26129 Oldenburg, Germany, 7Martinos Center for Biomedical Imaging, Department of Neurology, Massachusetts General Hospital/Harvard Medical School, Charlestown, Massachusetts 02129 Evidence from animal and human studies suggests that moderate acoustic exposure, causing only transient threshold elevation, can nonetheless cause “hidden hearing loss” that interferes with coding of suprathreshold sound. Such noise exposure destroys synaptic connections between cochlear hair cells and auditory nerve fibers; however, there is no clinical test of this synaptopathy in humans. In animals, synaptopathy reduces the amplitude of auditory brainstem response (ABR) wave-I. Unfortunately, ABR wave-I is difficult to measure in humans, limiting its clinical use. Here, using analogous measurements in humans and mice, we show that the effect of masking noise on the latency of the more robust ABR wave-V mirrors changes in ABR wave-I amplitude. -

Hearing Loss Due to Myringotomy and Tube Placement and the Role of Preoperative Audiograms
ORIGINAL ARTICLE Hearing Loss Due to Myringotomy and Tube Placement and the Role of Preoperative Audiograms Mark Emery, MD; Peter C. Weber, MD Background: Postoperative complications of myrin- erative and postoperative sensorineural and conductive gotomy and tube placement often include otorrhea, tym- hearing loss. panosclerosis, and tympanic membrane perforation. How- ever, the incidence of sensorineural or conductive hearing Results: No patient developed a postoperative sensori- loss has not been documented. Recent efforts to curb the neural or conductive hearing loss. All patients resolved use of preoperative audiometric testing requires docu- their conductive hearing loss after myringotomy and tube mentation of this incidence. placement. There was a 1.3% incidence of preexisting sen- sorineural hearing loss. Objective: To define the incidence of conductive and sensorineural hearing loss associated with myrin- Conclusions: The incidence of sensorineural or con- gotomy and tube placement. ductive hearing loss after myringotomy and tube place- ment is negligible and the use of preoperative audiomet- Materials and Methods: A retrospective chart re- ric evaluation may be unnecessary in selected patients, view of 550 patients undergoing myringotomy and tube but further studies need to be done to corroborate this placement was performed. A total of 520 patients under- small data set. going 602 procedures (1204 ears), including myrin- gotomy and tube placement, were assessed for preop- Arch Otolaryngol Head Neck Surg. 1998;124:421-424 TITIS MEDIA (OM) is one erative hearing status and whether it has of the most frequent dis- either improved or remained stable after eases of childhood, af- MTT. A recent report by Manning et al11 fecting at least 80% of demonstrated a 1% incidence of preop- children prior to school erative sensorineural hearing loss (SNHL) Oentry.1-4 Because of the high incidence of in children undergoing MTT. -
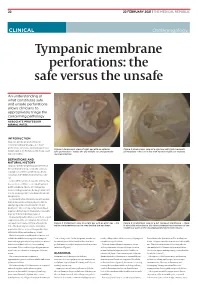
Tympanic Membrane Perforations: the Safe Versus the Unsafe
TMR_210222_22 2021-02-12T14:56:54+11:00 22 22 FEBRUARY 2021 | THE MEDICAL REPUBLIC CLINICAL Otolaryngology Tympanic membrane perforations: the safe versus the unsafe An understanding of what constitutes safe and unsafe perforations allows clinicians to appropriately triage the concerning pathology ASSOCIATE PROFESSOR NIRMAL PATEL INTRODUCTION Tympanic membrane perforations are seen frequently in general practice. Some perforations can be associated with significant Figure 1: Endoscopic view of right ear with an anterior Figure 2: Endoscopic view of a right ear with twin traumatic disease, such as cholesteatoma which may cause safe perforation – notice the dry middle ear and posterior perforations – the ear is dry with normal middle ear mucosa. major morbidity. myringosclerosis DEFINITIONS AND NATURAL HISTORY Tympanic membrane perforations are holes in the ear drum that most commonly occur as a consequence of either ear infections, chronic eustachian tube dysfunction or trauma to the ear. Acute middle ear infection (acute otitis media) is a common condition occurring at least once in 80% of children. Most acute otitis media resolves with spontaneous discharge of infected secretions through the eustachian tube into the nasopharynx. Occasionally when the infections are frequent, there is extensive scarring (tympanosclerosis and myringosclerosis) of the ear drum and middle ear . This scarring compromises blood supply to the healing ear drum and occasionally stops the hole from healing. (Figure 1) Traumatically induced holes occur from a rapid compression of the air column in the external ear canal, most commonly from a blow to the Figure 3: Endoscopic view of a right ear with an attic wax – the Figure 4: Endoscopic view of a left tympanic membrane – there white cholesteatoma can be seen behind the ear drum. -

Hearing Thresholds, Tinnitus, and Headphone Listening Habits in Nine-Year-Old Children
International Journal of Audiology ISSN: 1499-2027 (Print) 1708-8186 (Online) Journal homepage: http://www.tandfonline.com/loi/iija20 Hearing thresholds, tinnitus, and headphone listening habits in nine-year-old children Sara Båsjö, Claes Möller, Stephen Widén, Göran Jutengren & Kim Kähäri To cite this article: Sara Båsjö, Claes Möller, Stephen Widén, Göran Jutengren & Kim Kähäri (2016) Hearing thresholds, tinnitus, and headphone listening habits in nine-year-old children, International Journal of Audiology, 55:10, 587-596, DOI: 10.1080/14992027.2016.1190871 To link to this article: http://dx.doi.org/10.1080/14992027.2016.1190871 © 2016 The Author(s). Published by Informa UK Limited, trading as Taylor & Francis Group. Published online: 22 Jun 2016. Submit your article to this journal Article views: 456 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=iija20 Download by: [Linköping University Library] Date: 07 November 2016, At: 05:25 International Journal of Audiology 2016; 55: 587–596 Original Article Hearing thresholds, tinnitus, and headphone listening habits in nine-year-old children Sara Ba˚sjo¨1,2, Claes Mo¨ller1, Stephen Wide´n1,Go¨ran Jutengren3 & Kim Ka¨ha¨ri4 1Audiological Research Centre, School of Health and Medical Sciences / Swedish Institute for Disability Research, O¨ rebro University Hospital, O¨ rebro University, O¨ rebro, Sweden, 2HEAD Graduate School, Linko¨ping University, Linko¨ping, Sweden, 3School of Health Sciences, University of Bora˚s, Bora˚s, Sweden, and 4Division of Audiology, Sahlgrens’ Academy at Go¨teborg University, Go¨teborg, Sweden ABSTRACT Objective: Investigate hearing function and headphone listening habits in nine-year-old Swedish children. -

Correlations Between Audiogram and Objective Hearing Tests in Sensorineural Hearing Loss
International Tinnitus Journal, Vol. 5, No.2, 107-112 (1999) Correlations Between Audiogram and Objective Hearing Tests in Sensorineural Hearing Loss L. Bishara,1 J. Ben-David,l L. Podoshin,1 M. Fradis,l C.B. Teszler,l H. Pratt,2 T. Shpack,3 H. Feiglin,3 H. Hafner,3 and N. Herlinger2 I Department of Otolaryngology, Head and Neck Surgery, and 3Institute of Audiology, Bnai-Zion Medical Center, and 2Evoked Potentials Laboratory, Technion, Haifa, Israel Abstract: Owing to its subjective nature, behavioral pure-tone audiometry often is an unre liable testing method in uncooperative subjects, and assessing the true hearing threshold be comes difficult. In such cases, objective tests are used for hearing-threshold determination (i.e., auditory brainstem evoked potentials [ABEP] and frequency-specific auditory evoked potentials: slow negative response at 10 msec [SN-1O]). The purpose of this study was to evaluate the correlation between pure-tone audiogram shape and the predictive accuracy of SN-IO and ABEP in normal controls and in patients suf fering from sensorineural hearing loss (SNHL). One-hundred-and-fifty subjects aged 15 to 70, some with normal hearing and the remainder with SNHL, were tested prospectively in a double-blind design. The battery of tests included pure-tone audiometry (air and bone conduction), speech reception threshold, ABEP, and SN- 10. Patients with SNHL were divided into four categories according to audiogram shape (i.e., flat, ascending, descending, and all other shapes). The results showed that ABEP predicts behavioral thresholds at 3 kHz and 4 kHz in cases of high-frequency hearing loss. -
Introduction to Tympanometry
Tympanometry – Quick Guide Page 1 of 6 Introduction to Tympanometry This is an introduction to understanding and reporting on tympanometry measurements. This guide should be used in conjunction with your own clinic’s protocols and current research in the area of acoustic immittance testing. Some Useful Terminology Ear Canal Volume “The equivalent ear canal volume (ECV) is an estimate of the volume of air medial to the probe, which includes the volume between the probe tip and the tympanic membrane if the tympanic membrane is intact, or the volume of the ear canal and the middle ear space if the tympanic membrane is perforated” (Fowler & Shanks, 2002, p. 180). Averages Children 3 – 5yrs: 0.4cc to 1.0cc Adults: 0.6cc to 1.5cc Ear canal volume with an ECV >2.0 with a type B tympanogram in children suggests a perforated TM or patent grommet. Very small ECV with a type B tympanogram suggested impacted wax or middle ear pathology (glue ear?). Tympanometric Peak Pressure/Middle Ear Pressure Tympanometric peak pressure (TTP) or middle ear pressure (MEP) is the ear canal pressure at which the peak of the tympanogram occurs (Margolis & Hunter, 2000). Static Compliance Static compliance (SC) “is the greatest amount of acoustic energy absorbed by the middle ear system (the vertical peak of the tympanic tracing)” (Onusko, 2004, p. 1716). Gradient “Tympanogram gradient is an objective measure that describes the steepness of the slope of the tympanogram near the peak” (Fowler & Shanks, 2002, p.182). The gradient is not commonly used in Australia to analyse -

Hearing Screening Training Manual REVISED 12/2018
Hearing Screening Training Manual REVISED 12/2018 Minnesota Department of Health (MDH) Community and Family Health Division Maternal and Child Health Section 1 2 For more information, contact Minnesota Department of Health Maternal Child Health Section 85 E 7th Place St. Paul, MN 55164-0882 651-201-3760 [email protected] www.health.state.mn.us Upon request, this material will be made available in an alternative format such as large print, Braille or audio recording. 3 Revisions made to this manual are based on: Guidelines for Hearing Screening After the Newborn Period to Kindergarten Age http://www.improveehdi.org/mn/library/files/afternewbornperiodguidelines.pdf American Academy of Audiology, Childhood Screening Guidelines http://www.cdc.gov/ncbddd/hearingloss/documents/AAA_Childhood%20Hearing%2 0Guidelines_2011.pdf American Academy of Pediatrics (AAP), Hearing Assessment in Children: Recommendations Beyond Neonatal Screening http://pediatrics.aappublications.org/content/124/4/1252 4 Contents Introduction .................................................................................................................... 7 Audience ..................................................................................................................... 7 Purpose ....................................................................................................................... 7 Overview of hearing and hearing loss ............................................................................ 9 Sound, hearing, and hearing -

Consultation Diagnoses and Procedures Billed Among Recent Graduates Practicing General Otolaryngology – Head & Neck Surger
Eskander et al. Journal of Otolaryngology - Head and Neck Surgery (2018) 47:47 https://doi.org/10.1186/s40463-018-0293-8 ORIGINALRESEARCHARTICLE Open Access Consultation diagnoses and procedures billed among recent graduates practicing general otolaryngology – head & neck surgery in Ontario, Canada Antoine Eskander1,2,3* , Paolo Campisi4, Ian J. Witterick5 and David D. Pothier6 Abstract Background: An analysis of the scope of practice of recent Otolaryngology – Head and Neck Surgery (OHNS) graduates working as general otolaryngologists has not been previously performed. As Canadian OHNS residency programs implement competency-based training strategies, this data may be used to align residency curricula with the clinical and surgical practice of recent graduates. Methods: Ontario billing data were used to identify the most common diagnostic and procedure codes used by general otolaryngologists issued a billing number between 2006 and 2012. The codes were categorized by OHNS subspecialty. Practitioners with a narrow range of procedure codes or a high rate of complex procedure codes, were deemed subspecialists and therefore excluded. Results: There were 108 recent graduates in a general practice identified. The most common diagnostic codes assigned to consultation billings were categorized as ‘otology’ (42%), ‘general otolaryngology’ (35%), ‘rhinology’ (17%) and ‘head and neck’ (4%). The most common procedure codes were categorized as ‘general otolaryngology’ (45%), ‘otology’ (23%), ‘head and neck’ (13%) and ‘rhinology’ (9%). The top 5 procedures were nasolaryngoscopy, ear microdebridement, myringotomy with insertion of ventilation tube, tonsillectomy, and turbinate reduction. Although otology encompassed a large proportion of procedures billed, tympanoplasty and mastoidectomy were surprisingly uncommon. Conclusion: This is the first study to analyze the nature of the clinical and surgical cases managed by recent OHNS graduates. -

Tympanostomy Tubes in Children Final Evidence Report: Appendices
Health Technology Assessment Tympanostomy Tubes in Children Final Evidence Report: Appendices October 16, 2015 Health Technology Assessment Program (HTA) Washington State Health Care Authority PO Box 42712 Olympia, WA 98504-2712 (360) 725-5126 www.hca.wa.gov/hta/ [email protected] Tympanostomy Tubes Provided by: Spectrum Research, Inc. Final Report APPENDICES October 16, 2015 WA – Health Technology Assessment October 16, 2015 Table of Contents Appendices Appendix A. Algorithm for Article Selection ................................................................................................. 1 Appendix B. Search Strategies ...................................................................................................................... 2 Appendix C. Excluded Articles ....................................................................................................................... 4 Appendix D. Class of Evidence, Strength of Evidence, and QHES Determination ........................................ 9 Appendix E. Study quality: CoE and QHES evaluation ................................................................................ 13 Appendix F. Study characteristics ............................................................................................................... 20 Appendix G. Results Tables for Key Question 1 (Efficacy and Effectiveness) ............................................. 39 Appendix H. Results Tables for Key Question 2 (Safety) ............................................................................ -

ICD-9 Diseases of the Ear and Mastoid Process 380-389
DISEASES OF THE EAR AND MASTOID PROCESS (380-389) 380 Disorders of external ear 380.0 Perichondritis of pinna Perichondritis of auricle 380.00 Perichondritis of pinna, unspecified 380.01 Acute perichondritis of pinna 380.02 Chronic perichondritis of pinna 380.1 Infective otitis externa 380.10 Infective otitis externa, unspecified Otitis externa (acute): NOS circumscribed diffuse hemorrhagica infective NOS 380.11 Acute infection of pinna Excludes: furuncular otitis externa (680.0) 380.12 Acute swimmers' ear Beach ear Tank ear 380.13 Other acute infections of external ear Code first underlying disease, as: erysipelas (035) impetigo (684) seborrheic dermatitis (690.10-690.18) Excludes: herpes simplex (054.73) herpes zoster (053.71) 380.14 Malignant otitis externa 380.15 Chronic mycotic otitis externa Code first underlying disease, as: aspergillosis (117.3) otomycosis NOS (111.9) Excludes: candidal otitis externa (112.82) 380.16 Other chronic infective otitis externa Chronic infective otitis externa NOS 380.2 Other otitis externa 380.21 Cholesteatoma of external ear Keratosis obturans of external ear (canal) Excludes: cholesteatoma NOS (385.30-385.35) postmastoidectomy (383.32) 380.22 Other acute otitis externa Excerpted from “Dtab04.RTF” downloaded from website regarding ICD-9-CM 1 of 11 Acute otitis externa: actinic chemical contact eczematoid reactive 380.23 Other chronic otitis externa Chronic otitis externa NOS 380.3 Noninfectious disorders of pinna 380.30 Disorder of pinna, unspecified 380.31 Hematoma of auricle or pinna 380.32 Acquired