Global Perspective on Kidney Transplantation: Turkey Oya Andacoglu1* and Fazil Tuncay Aki2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
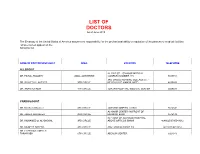
LIST of DOCTORS As of June 2018
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -
Certified by
Flesh yours, Bones Mine The Making of the Biomedical Subject in Turkey by Aslihan Sanal SUBMITTED TO THE PROGRAM IN SCIENCE, TECHNOLOGY AND SOCIETY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THeEDEGREE OF DOCTOR OF PHILOSOPHY IN THE DEPARTMENT OF HISTORY, ANTHROPOLOGY, SCIENCE, TECHNOLOGY AND SOCIETY AT THE MAS H OFTECHNOLOGY MASSACHUSETTS INSTITUTE OF TECHNOLOGY OF T ECHNO JUNE 2005G 1 8 © 2005 Aslihan Sanal All rights reserved LlBA RI The author hereby grants to MIT permission to reproduce and to distribute publicly paper and electronic copies of this thesis document in whole or in part. .I Signatureof Author ......................... ......................... Program inS on-Tcbrology and Society - April 29, 2005 Certified by.... ......... o..................... /7'JgG 1 Michael M J Fischer /\. Jofessor o fAnthropoloy3gnd,Science and Technology Studies Thesis Advisor Certified by ........ ........ ................... U,' I- Harriet Ritvo Professor of History Committee memtber Certified by............ - . ....................................................................... Sherry Turkle Professor of the Social Studies of Science and Technology Committee member Certified by.... ....................................... Joseph Dumit ctC9 Associate Professor of Anthropology Committee member Certifiedby . ........................ .................................... - Jodo Biehl Assistant Professor of Anthropology Princeton University Committee member Accepted by ..... .. ........ ...... ........................................... -
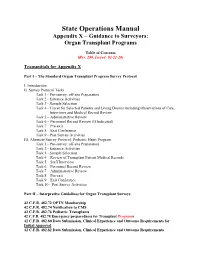
State Operations Manual Appendix X – Guidance to Surveyors: Organ Transplant Programs
State Operations Manual Appendix X – Guidance to Surveyors: Organ Transplant Programs Table of Contents (Rev. 200, Issued: 02-21-20) Transmittals for Appendix X Part I – The Standard Organ Transplant Program Survey Protocol I. Introduction II. Survey Protocol Tasks Task 1 - Pre-survey: off-site Preparation Task 2 - Entrance Activities Task 3 - Sample Selection Task 4 - Tracer for Selected Patients and Living Donors including Observations of Care, Interviews and Medical Record Review Task 5 – Administrative Review Task 6 – Personnel Record Review (If Indicated) Task 7 – Pre-exit Task 8 – Exit Conference Task 9 - Post Survey Activities III. Alternate Survey Protocol: Pediatric Heart Program Task 1 - Pre-survey: off-site Preparation Task 2 - Entrance Activities Task 3 - Sample Selection Task 4 – Review of Transplant Patient Medical Records Task 5 – Staff Interview Task 6 – Personnel Record Review Task 7 – Administrative Review Task 8 – Pre-exit Task 9 – Exit Conference Task 10 - Post Survey Activities Part II – Interpretive Guidelines for Organ Transplant Surveys 42 C.F.R. 482.72 OPTN Membership 42 C.F.R. 482.74 Notification to CMS 42 C.F.R. 482.76 Pediatric Transplants 42 C.F.R. 482.78 Emergency preparedness for Transplant Programs 42 C.F.R. 482.80 Data Submission, Clinical Experience and Outcome Requirements for Initial Approval 42 C.F.R. 482.82 Data Submission, Clinical Experience and Outcome Requirements Re-approval 42 C.F.R. 482.90 Patient and Living Donor Selection 42 C.F.R. 482.92 Organ Recovery and Receipt 42 C.F.R. 482.94 Patient and Living Donor Management 42 C.F.R. -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Intestine Transplant Manual
Intestine Transplant Manual Toronto Intestine Transplant Program TRANSPLANT MANUAL E INTESTIN This manual is dedicated to our donors, our patients and their families Acknowledgements Dr. Mark Cattral, MD, (FRCSC) Dr. Yaron Avitzur, MD Andrea Norgate, RN, BScN Sonali Pendharkar, BA (Hons), BSW, MSW, RSW Anna Richardson, RD We acknowledge the contribution of previous members of the team and to Cheryl Beriault (RN, BScN) for creating this manual. 2 TABLE OF CONTENTS Dedications and Acknowledgements 2 Welcome 5 Our Values and Philosophy of Care Our Expectations of You Your Transplant Team 6 The Function of the Liver and Intestines 9 Where are the abdominal organs located and what do they look like? What does your Stomach do? What does your Intestine do? What does your Liver do? What does your Pancreas do? When Does a Patient Need an Intestine Transplant? 12 Classification of Intestine Failure Am I Eligible for an Intestine Transplant? Advantages and Disadvantages of Intestine Transplant The Transplant Assessment 14 Investigations Consultations Active Listing for Intestine Transplantation (Placement on the List) 15 Preparing for the Intestine Transplant Trillium Drug Program Other Sources of Funding for Drug Coverage Financial Planning Insurance Issues Other Financial Considerations Related to the Hospital Stay Legal Considerations for Transplant Patients Advance Care Planning Waiting for the Intestine Transplant 25 Your Place on the Waiting List Maintaining Contact with the Transplant Team Coping with Stress Maintaining your Health While -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Akademik Faaliyet Raporu 2005-2006
BAŞKENT ÜNİVERSİTESİ 1 Ekim 2005 - 30 Eylül 2006 BAŞK ENT ÜN İV E R S İT E S İ 2 0 0 5 - 2 0 0 6 E ğ i t i m - Ö ğ r e t i m Y ı l ı Ç a l ı ş m a R a p o r u 2 Amfi Tiyatro / Bağlıca Kampüsü BAŞKENT ÜNİVERSİTESİ 2005-2006 Eğitim-Öğretim Yılı Çalışma Raporu İÇİNDEKİLER Ýçindekiler İlkyardım Eğitim Merkezi . .77 Kadın-Çocuk Sağlığı ve Aile Planlaması Araştırma ve I. Kuruluþ ve Geliþme . 4 Uygulama Merkezi . 78 Akademik Değerlendirme Koordinatörlüğü . 8 Ölçümbilim ve Kalibrasyon Uyguluma ve Araştırma Merkezi . .78 Prof.Dr.Mithat Çoruh Toplam Kalite Yönetim Merkezi . 9 Kültür ve Sanat Araştırma Merkezi . 79 Stratejik Araştırmalar Merkezi . 82 II. Yerleþme Düzeni . 12 Dil Araştırma ve Uygulama Merkezi . .84 Şehir Kampüsü . 12 Afet Eğitim, Müdahale Uygulama ve Araştırma Merkezi . 84 Bağlıca Kampüsü . 14 IX. Diðer Birimler ve Hizmetler . 86 III. Personel . 18 Uluslararası İlişkiler Koordinatörlüğü . .86 Akademik Personel . 18 Bilgi İşlem Hizmetleri . .90 İdari, Sağlık ve Teknik Personel . 20 Foto-Film Merkezi . 97 IV. Eðitim-Öðretim . 21 İnsan Kaynakları ve Kariyer Yönlendirme Merkezi . .98 Önlisans ve Lisans . 21 Kütüphane ve Dokümantasyon Hizmetleri . 99 Tıpta Uzmanlık Eğitimi . 32 Mediko-Sosyal Hizmetler . .103 Lisansüstü Eğitimi . 34 Sağlık Hizmetleri . .103 Burslar . 36 Özürlü Öğrenciler Birimi . .103 V. Baþkent Üniversitesine Baðlý Ýlk ve Ortaöðretim Yurtlar . 104 3 Okullarý . 40 Beslenme . 106 Ulaşım . 107 VI. Bilimsel Faaliyetler . 48 Psikolojik Danışma ve Rehberlik Merkezi . .108 Yayınlar . 48 Tanıtım Ofisi . 110 Atıflar . 52 Basın-Yayın ve Halkla İlişkiler . 112 Bilimsel Toplantılar . 52 Araştırma Projeleri . -

100 Years. 100 Facts
100 Years. 100 Facts. Celebrating 100 Years as the United Voice of Ohio Hospitals 1819 Daniel Drake obtains a charter for the Medical 001 College of Ohio, the forerunner of the University of Cincinnati College of Medicine. 100 Years. 100 Facts. | 3 1823 Ohio’s first hospital, the Cincinnati Commercial 002 Hospital and Lunatic Asylum, opens. 4 | Ohio Hospital Association 100 Years. 100 Facts. | 5 Starling Medical Center College/Saint 003 Francis Hospital is established on the 1849 present site of Grant Medical Center in Columbus as the first teaching hospital in the U.S. It is the forerunner for the College of Medicine at Ohio State University. 6 | Ohio Hospital Association Charity Hospital Medical Center, now 004 St. Vincent Charity Hospital, opens 1873 Cleveland’s first amphitheater for demonstration of surgery and clinical procedures. 100 Years. 100 Facts. | 7 8 | Ohio Hospital Association 1886 Mother M. Angela and Sister M. Rufina Dunn, of the 005 Congregation of the Sisters of the Holy Cross of Notre Dame, Indiana, convert a sturdy four-story red brick building to two wards, 18 private rooms and an operating room with an amphitheater. The facility is called Hawkes Hospital of Mount Carmel and eventually becomes Mount Carmel West. 100 Years. 100 Facts. | 9 A 10-bed Christ Hospital opens in 006 Cincinnati after a group of local 1889 businessmen led by James Gamble (whose prospering soap business eventually became Procter & Gamble) invited Isabella Thornburg to the city in 1888 to train deaconesses and missionaries. She soon expands beyond training to open a hospital in the west end of the city. -
Go Inside a Surgeon's Typical
HealthSigns Spring 2016 Go Inside a Surgeon’s Typical Day Top in Cancer Getting the Planet Friendly Care Picture Healthcare Earning kudos on quality More advanced imaging How we care for patients for nearly a decade tools in your community and the environment HealthSigns Spring 2016 5 10 Sustaining Going Quality Green Cancer program We’re leading the earns top national way to a healthier, award for third more sustainable time. environment. 6 11 Focused on Parking Garage Healing Near Opening General surgeon More convenient starts each day access helps with energy and patients, families endurance. and our community. 8 Easy Access to Imaging Outpatient center VISIT US ONLINE offers screenings, Stay connected to Washington Hospital at www.whhs.com diagnostics and and on Facebook. Browse our calendar of upcoming events and treatment. other happenings taking place at your community hospital. 2 | SPRING 2016 Information You Can Use MISSION STATEMENT Free, science-based diabetes education classes for people with diabetes and their families or anyone who wants to As the local Health Care District, find out more about this chronic disease affecting more our mission is to meet the than 29 million Americans. health care needs of the District Diabetes Matters residents through medical services, education and research. When: First Thursday of every month (except for July), 7 to 8 p.m. Within this scope, Washington Stay for the Diabetes Support Township Health Care District Group, 8 to 9 p.m. is committed to assuming the Location: Conrad E. Anderson, MD, Auditorium (Washington West) leadership role in improving and 2500 Mowry Ave., Fremont maintaining the health status of No registration needed. -

Our Mission: to Advance the Art and Science of Transplant Surgery Through Leadership, Advocacy, Education, and Training
Published for Members of the American Society of Transplant Surgeons Summer 2014 7th Annual Surgical Fellows Symposium: Elevating the Educational Experience Snowbird, Utah Our Mission: To advance the art and science of transplant surgery through leadership, advocacy, education, and training. ASTS.org Chimera Summer 2014 1 ASTS Council July 2014 – May 2015 Vol. XXIV, No. 3 Summer 2014 President Lloyd E. Ratner, MD, MPH (2015) Peter G. Stock, MD, PhD (2015) Columbia University University of California-San Francisco Department of Surgery Department of Surgery, 622 West 168th Street, New York, NY 10032 Division of Transplant 212-342-3539 [email protected] 505 Parnassus Avenue, Box 0780 San Francisco, CA 94143-0780 Douglas G. Farmer, MD (2016) 415-353-1551 [email protected] Ronald Reagan UCLA Medical Center Surgery-Liver & Pancreas Transplant President-Elect MC7054 Charles M. Miller, MD (2015) 757 Westwood Plaza, Suite 8501 Cleveland Clinic Foundation Los Angeles, CA 90095-9574 9500 Euclid Avenue, Mail Code A-110 310-267-9612 [email protected] Cleveland, OH 44195 216-445-2381 [email protected] James F. Markmann, MD, PhD (2016) Division of Transplantation 20 Immediate Past President 55 Fruit Street Alan N. Langnas, DO (2014) 503 White Building Editor’s Letter 3 University of Nebraska Medical Center Boston, MA 02114 PO Box 983280, 600 South 42nd Street 617-643-4533 [email protected] President’s Letter 4 Omaha, NE 68198 402-559-8390 [email protected] Mark D. Stegall, MD (2016) ASTS News 5 Mayo Clinic Past President 200 First Street, SW ASTS Fellowship Training 8 Kim M. -

14 Glossary of Healthcare Terms
Premera Reference Manual Premera Blue Cross 1144 GGlloossssaarryy ooff HHeeaalltthhccaarree TTeerrmmss A Accreditation: Health plan accreditation is a rigorous, comprehensive and transparent evaluation process through which the quality of the systems, processes and results that define a health plan are assessed. Acute: A condition that begins suddenly and does not last very long (e.g., broken arm). ‘acute” is the opposite of “chronic.” Acute Care: Treatment for a short-term or episodic illness or health problem. Adequacy: The extent to which a network offers the appropriate types and numbers of providers in a designated geographic distribution according to the relative availability of such providers in the area and the needs of the plan's members. Adjudication: The process of handling and paying claims. Also see Claim. Admission Notification: Hospitals routinely notify Premera of all inpatient admissions that link members to other care coordination programs, such as readmission prevention. The process includes verification of benefits and assesses any need for case management. Advance Directives: Written instructions that describe a member’s healthcare decision regarding treatment in the event of a serious medical condition which prevents the member from communicating with his/her physician; also called Living Wills. Allied Health Personnel: Specially trained and licensed (when necessary) healthcare workers other than physicians, optometrists, dentists, chiropractors, podiatrists, and nurses. Allowable: An amount agreed upon by the carrier and the practitioner as payment for covered services. Alpha Prefix: Three characters preceding the subscriber identification number on Blue Cross and/or Blue Shield plan ID cards. The alpha prefix identifies the member’s Blue Cross and/or Blue Shield plan or national account and is required for routing claims. -

C = Committee Chair I = Incoming Chair R = Representative L = Councilor Liaison S = Staff Liaison G=Guest
Mission: To advance the art and science of transplant surgery through leadership, advocacy, education, and training. 1 Vision: Saving and improving lives with transplantation. Strategic Plan Goals: Advocacy, Research, Training & Prof Development, Optimal Patient Care, & Organizational Excellence. Core Values: Integrity, Respect, Excellence, Diversity, Compassion, and Forward Focus. Council & Committee Chair Meeting Agenda April 29, 2017 Hyatt McCormick Place Hotel 2nd Floor, Regency Ballroom Time Agenda Items Presenter Tab Action Items Organizational Excellence 7:30 AM Call to Order • COI review • Meeting structure/strategic T. Pruett A plan • In memoriam 7:45 AM Financial Update L. Ratner – C K. Gifford – S 7:55 AM Foundation Report C. Miller – C B M. K-Bullock – S 8:10 AM Nominating Report • Election results T. Pruett – C • Committee appointments M. K-Bullock – S C • Recognition of outgoing cmte E. Proffitt – S chairs 8:20 AM Membership & Workforce Report 1. Request feedback on WF survey • Workforce survey manuscript manuscript • New member approval policy J. Rocca – C D-1 2. Request approval of update to the update K. Chavin – L D-2 new member approval policy • Collection of workforce N. Duan – S D-3 3. Request feedback on selected WF metrics metrics for systematic collection by ASTS 8:40 AM Bylaws Report • Bylaws amendment for vote at R. Pelletier – C E-1 business meeting K. Chavin – L E-2 • Non-clinical member L. Kulikosky – S E-3 participation policy 8:50 AM Historian Report T. Peters – C 4. Request approval for funding of F • Future Chimera Chronicles D. Mossholder – S future Chimera Chronicles N/A Written Reports Only • Communications – J.